22. Skin and Eye Infections
22.5 Protozoan Infections of the Skin and Eyes
Learning Objectives
- Identify two parasites that commonly cause infections of the skin and eyes
- Identify the major characteristics of specific parasitic diseases affecting the skin and eyes
Many parasitic protozoans and helminths use the skin or eyes as a portal of entry. Some may physically burrow into the skin or the mucosa of the eye; others breach the skin barrier by means of an insect bite. Still others take advantage of a wound to bypass the skin barrier and enter the body, much like other opportunistic pathogens. Although many parasites enter the body through the skin, in this chapter we will limit our discussion to those for which the skin or eyes are the primary site of infection. Parasites that enter through the skin but travel to a different site of infection will be covered in other chapters. In addition, we will limit our discussion to microscopic parasitic infections of the skin and eyes. Macroscopic parasites such as lice, scabies, mites, and ticks are beyond the scope of this text.
Acanthamoeba Infections
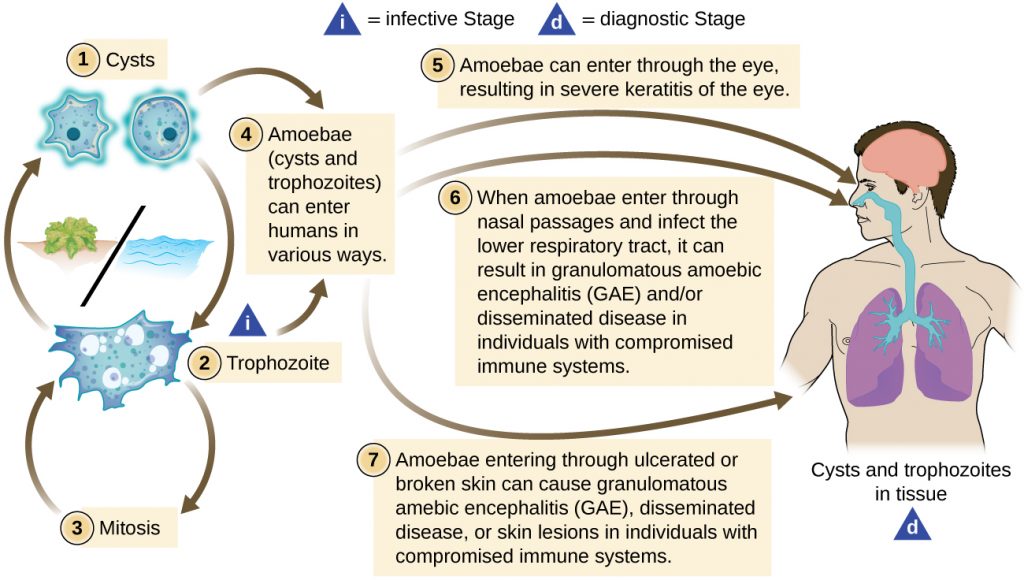
Acanthamoeba is a genus of free-living protozoan amoebae that are common in soils and unchlorinated bodies of fresh water. (This is one reason why some swimming pools are treated with chlorine.) The genus contains a few parasitic species, some of which can cause infections of the eyes, skin, and nervous system. Such infections can sometimes travel and affect other body systems. Skin infections may manifest as abscesses, ulcers, and nodules. When acanthamoebae infect the eye, causing inflammation of the cornea, the condition is called Acanthamoeba keratitis. Figure 22.30 illustrates the Acanthamoeba life cycle and various modes of infection.
While Acanthamoeba keratitis is initially mild, it can lead to severe corneal damage, vision impairment, or even blindness if left untreated. Similar to eye infections involving P. aeruginosa, Acanthamoeba poses a much greater risk to wearers of contact lenses because the amoeba can thrive in the space between contact lenses and the cornea. Prevention through proper contact lens care is important. Lenses should always be properly disinfected prior to use, and should never be worn while swimming or using a hot tub.
Acanthamoeba can also enter the body through other pathways, including skin wounds and the respiratory tract. It usually does not cause disease except in immunocompromised individuals; however, in rare cases, the infection can spread to the nervous system, resulting in a usually fatal condition called granulomatous amoebic encephalitis (GAE) (see Fungal and Parasitic Diseases of the Nervous System). Disseminated infections, lesions, and Acanthamoeba keratitis can be diagnosed by observing symptoms and examining patient samples under the microscope to view the parasite. Skin biopsies may be used.
Acanthamoeba keratitis is difficult to treat, and prompt treatment is necessary to prevent the condition from progressing. The condition generally requires three to four weeks of intensive treatment to resolve. Common treatments include topical antiseptics (e.g., polyhexamethylene biguanide, chlorhexidine, or both), sometimes with painkillers or corticosteroids (although the latter are controversial because they suppress the immune system, which can worsen the infection). Azoles are sometimes prescribed as well. Advanced cases of keratitis may require a corneal transplant to prevent blindness.

- How are Acanthamoeba infections acquired?
DISEASE PROFILE: Parasitic Skin and Eye Infections
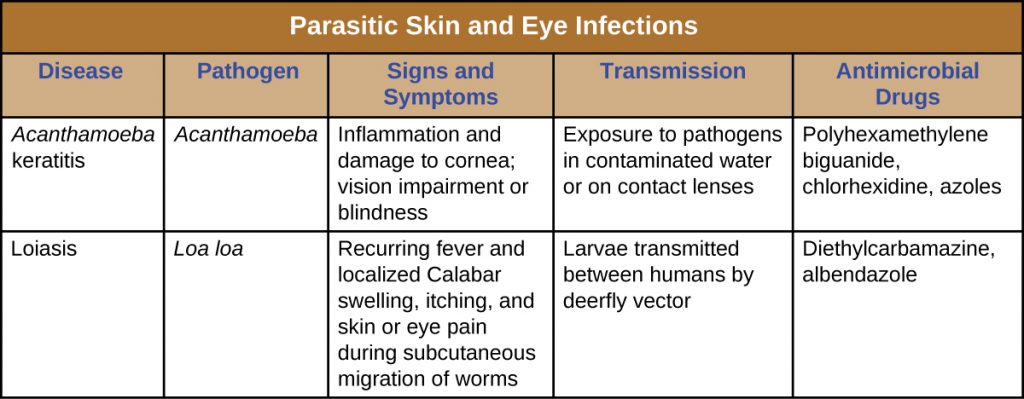
The protozoan Acanthamoeba is a parasite capable of causing infections of the skin and eyes. Table 22.8 summarizes the characteristics of some common protozoal infections of the skin.
Key Takeaways
- The protozoan Acanthamoeba is a parasite that can breach the skin barrier, causing infections of the skin and eyes.
- Acanthamoeba keratitis is a parasitic infection of the eye that often results from improper disinfection of contact lenses or swimming while wearing contact lenses.
Multiple Choice
Fill in the Blank
Media Attributions
- OSC_Microbio_21_05_acanthaLC
- OSC_Microbio_21_05_acanthamoe
- OSC_Microbio_21_05_parasiticInf

