25. Digestive System Infections
25.3 Bacterial Infections of the Gastrointestinal Tract
Learning Objectives
- Identify the most common bacteria that can cause infections of the GI tract
- Compare the major characteristics of specific bacterial diseases affecting the GI tract
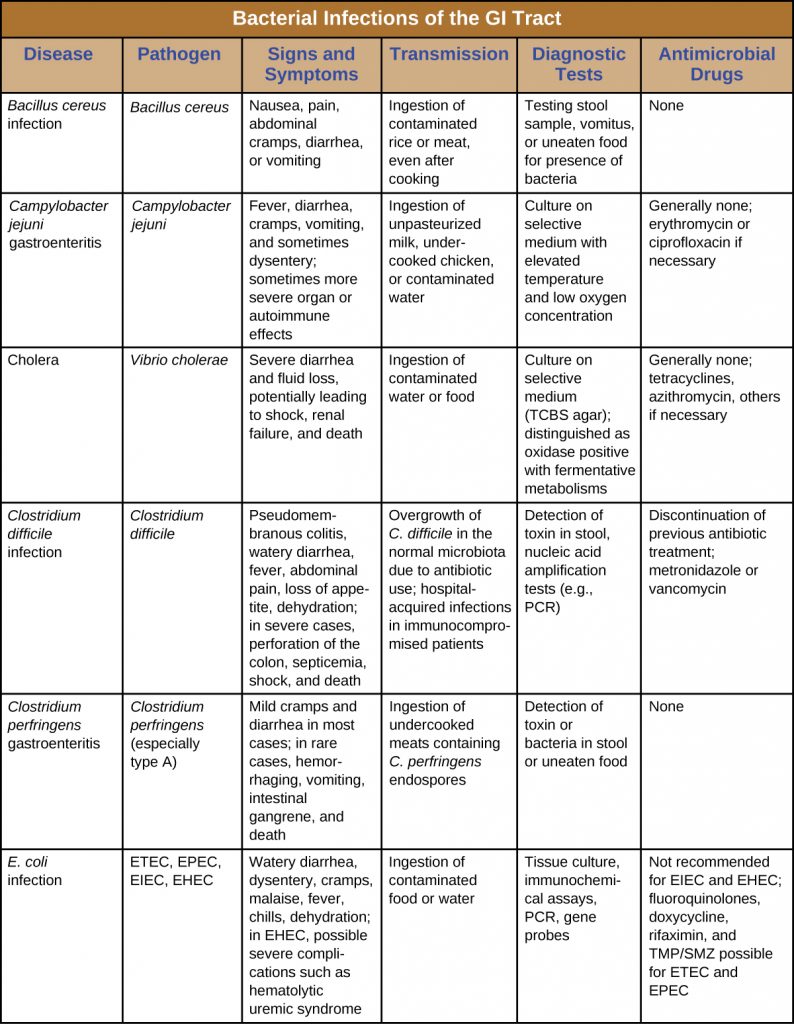
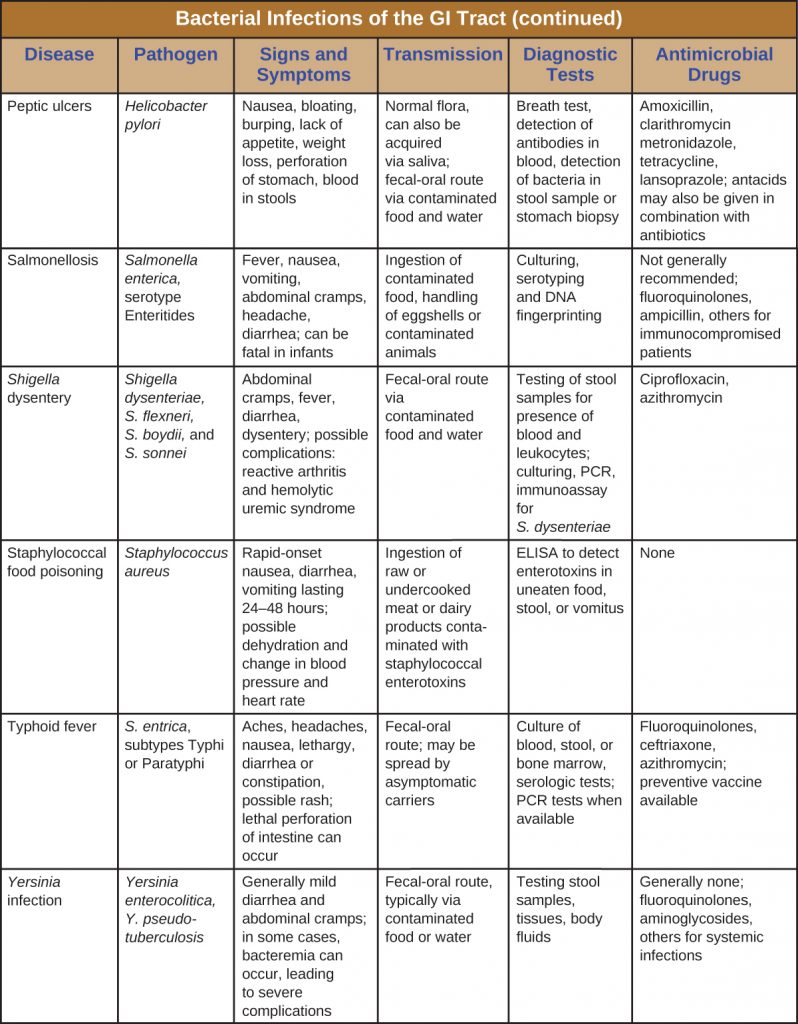
A wide range of gastrointestinal diseases are caused by bacterial contamination of food. Recall that food-borne disease can arise from either infection or intoxication. In both cases, bacterial toxins are typically responsible for producing disease signs and symptoms. The distinction lies in where the toxins are produced. In an infection, the microbial agent is ingested, colonizes the gut, and then produces toxins that damage host cells. In an intoxication, bacteria produce toxins in the food before it is ingested. In either case, the toxins cause damage to the cells lining the gastrointestinal tract, typically the colon. This leads to the common signs and symptoms of diarrhoea or watery stool and abdominal cramps, or the more severe dysentery. Symptoms of food-borne diseases also often include nausea and vomiting, which are mechanisms the body uses to expel the toxic materials.
Most bacterial gastrointestinal illness is short-lived and self-limiting; however, loss of fluids due to severe diarrhoeal illness can lead to dehydration that can, in some cases, be fatal without proper treatment. Oral rehydration therapy with electrolyte solutions is an essential aspect of treatment for most patients with GI disease, especially in children and infants.
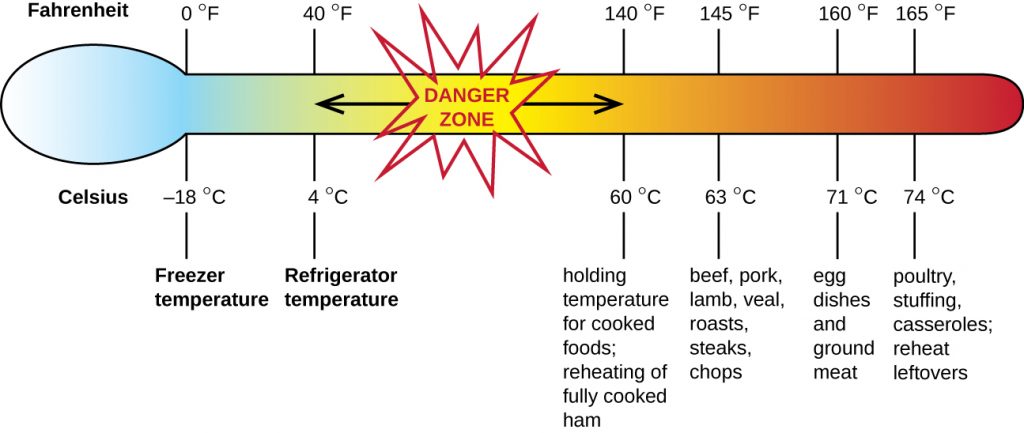
Staphylococcal Food Poisoning
Staphylococcal food poisoning is one form of food intoxication. When Staphylococcus aureus grows in food, it may produce enterotoxins that, when ingested, can cause symptoms such as nausea, diarrhoea, cramping, and vomiting within one to six hours. In some severe cases, it may cause headache, dehydration, and changes in blood pressure and heart rate. Signs and symptoms resolve within 24 to 48 hours. S. aureus is often associated with a variety of raw or undercooked and cooked foods including meat (e.g., canned meat, ham, and sausages) and dairy products (e.g., cheeses, milk, and butter). It is also commonly found on hands and can be transmitted to prepared foods through poor hygiene, including poor hand washing and the use of contaminated food preparation surfaces, such as cutting boards. The greatest risk is for food left at a temperature below 60 °C (140 °F), which allows the bacteria to grow. Cooked foods should generally be reheated to at least 60 °C (140 °F) for safety and most raw meats should be cooked to even higher internal temperatures (Figure 25.15).
There are at least 21 Staphylococcal enterotoxins and Staphylococcal enterotoxin-like toxins that can cause food intoxication. The enterotoxins are proteins that are resistant to low pH, allowing them to pass through the stomach. They are heat stable and are not destroyed by boiling at 100 °C. Even though the bacterium itself may be killed, the enterotoxins alone can cause vomiting and diarrhoea, although the mechanisms are not fully understood. At least some of the symptoms may be caused by the enterotoxin functioning as a superantigen and provoking a strong immune response by activating T cell proliferation.
The rapid onset of signs and symptoms helps to diagnose this food-borne illness. Because the bacterium does not need to be present for the toxin to cause symptoms, diagnosis is confirmed by identifying the toxin in a food sample or in biological specimens (faeces or vomitus) from the patient. Serological techniques, including ELISA, can also be used to identify the toxin in food samples.
The condition generally resolves relatively quickly, within 24 hours, without treatment. In some cases, supportive treatment in a hospital may be needed.
- How can S. aureus cause food intoxication?
Shigellosis (Bacillary Dysentery)
When gastrointestinal illness is associated with the rod-shaped, gram-negative bacterium Shigella, it is called bacillary dysentery, or shigellosis. Infections can be caused by S. dysenteriae, S. flexneri, S. boydii, and/or S. sonnei that colonize the GI tract. Shigellosis can be spread from hand to mouth or through contaminated food and water. Most commonly, it is transmitted through the faecal-oral route.
Shigella bacteria invade intestinal epithelial cells. When taken into a phagosome, they can escape and then live within the cytoplasm of the cell or move to adjacent cells. As the organisms multiply, the epithelium and structures with M cells of the Peyer’s patches in the intestine may become ulcerated and cause loss of fluid. Stomach cramps, fever, and watery diarrhoea that may also contain pus, mucus, and/or blood often develop. More severe cases may result in ulceration of the mucosa, dehydration, and rectal bleeding. Additionally, patients may later develop hemolytic uremic syndrome (HUS), a serious condition in which damaged blood cells build up in the kidneys and may cause kidney failure, or reactive arthritis, a condition in which arthritis develops in multiple joints following infection. Patients may also develop chronic post-infection irritable bowel syndrome (IBS).
S. dysenteriae type 1 is able to produce Shiga toxin, which targets the endothelial cells of small blood vessels in the small and large intestine by binding to a glycosphingolipid. Once inside the endothelial cells, the toxin targets the large ribosomal subunit, thus affecting protein synthesis of these cells. Hemorrhaging and lesions in the colon can result. The toxin can target the kidney’s glomerulus, the blood vessels where filtration of blood in the kidney begins, thus resulting in HUS.
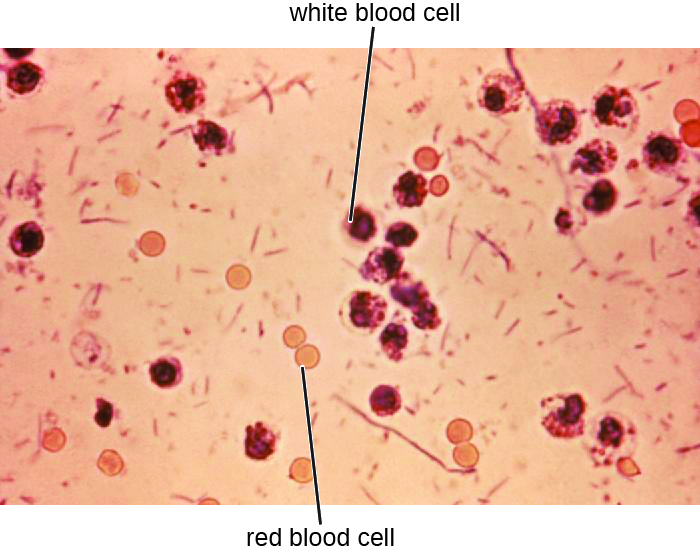
Stool samples, which should be processed promptly, are analyzed using serological or molecular techniques. One common method is to perform immunoassays for S. dysenteriae. (Other methods that can be used to identify Shigella include API test strips, Enterotube systems, or PCR testing. The presence of white blood cells and blood in faecal samples occurs in about 70% of patients[1] (Figure 25.16). Severe cases may require antibiotics such as ciprofloxacin and azithromycin, but these must be carefully prescribed because resistance is increasingly common.
- Compare and contrast Shigella infections and intoxications.
Salmonellosis
Salmonella gastroenteritis, also called salmonellosis, is caused by the rod-shaped, gram-negative bacterium Salmonella. Two species, S. enterica and S. bongori, cause disease in humans, but S. enterica is the most common. The most common serotypes of S. enterica are Enteritidis and Typhi. We will discuss typhoid fever caused by serotypes Typhi and Paratyphi A separately. Here, we will focus on salmonellosis caused by other serotypes.
Salmonella is a part of the normal intestinal microbiota of many individuals. However, salmonellosis is caused by exogenous agents, and infection can occur depending on the serotype, size of the inoculum, and overall health of the host. Infection is caused by ingestion of contaminated food, handling of eggshells, or exposure to certain animals. Salmonella is part of poultry’s microbiota, so exposure to raw eggs and raw poultry can increase the risk of infection. Hand-washing and cooking foods thoroughly greatly reduce the risk of transmission. Salmonella bacteria can survive freezing for extended periods but cannot survive high temperatures.
Once the bacteria are ingested, they multiply within the intestines and penetrate the epithelial mucosal cells via M cells where they continue to grow (Figure 25.17). They trigger inflammatory processes and the hypersecretion of fluids. Once inside the body, they can persist inside the phagosomes of macrophages. Salmonella can cross the epithelial cell membrane and enter the bloodstream and lymphatic system. Some strains of Salmonella also produce an enterotoxin that can cause an intoxication.
Infected individuals develop fever, nausea, abdominal cramps, vomiting, headache, and diarrhoea. These signs and symptoms generally last a few days to a week. According to the Centers for Disease Control and Prevention (CDC), there are 1,000,000 cases annually, with 380 deaths each year.[2] However, because the disease is usually self-limiting, many cases are not reported to doctors and the overall incidence may be underreported. Diagnosis involves culture followed by serotyping and DNA fingerprinting if needed. Positive results are reported to the CDC. When an unusual serotype is detected, samples are sent to the CDC for further analysis. Serotyping is important for determining treatment. Oral rehydration therapy is commonly used. Antibiotics are only recommended for serious cases. When antibiotics are needed, as in immunocompromised patients, fluoroquinolones, third-generation cephalosporins, and ampicillin are recommended. Antibiotic resistance is a serious concern.

Typhoid Fever
Certain serotypes of S. enterica, primarily serotype Typhi (S. typhi) but also Paratyphi, cause a more severe type of salmonellosis called typhoid fever. This serious illness, which has an untreated mortality rate of 10%, causes high fever, body aches, headache, nausea, lethargy, and a possible rash.
Some individuals carry S. typhi without presenting signs or symptoms (known as asymptomatic carriers) and continually shed them through their faeces. These carriers often have the bacteria in the gallbladder or intestinal epithelium. Individuals consuming food or water contaminated with these faeces can become infected.
S. typhi penetrate the intestinal mucosa, grow within the macrophages, and are transported through the body, most notably to the liver and gallbladder. Eventually, the macrophages lyse, releasing S. typhi into the bloodstream and lymphatic system. Mortality can result from ulceration and perforation of the intestine. A wide range of complications, such as pneumonia and jaundice, can occur with disseminated disease.
S. typhi have Salmonella pathogenicity islands (SPIs) that contain the genes for many of their virulence factors. Two examples of important typhoid toxins are the Vi antigen, which encodes for capsule production, and chimeric A2B5 toxin, which causes many of the signs and symptoms of the acute phase of typhoid fever.
Clinical examination and culture are used to make the diagnosis. The bacteria can be cultured from faeces, urine, blood, or bone marrow. Serology, including ELISA, is used to identify the most pathogenic strains, but confirmation with DNA testing or culture is needed. A PCR test can also be used, but is not widely available.
The recommended antibiotic treatment involves fluoroquinolones, ceftriaxone, and azithromycin. Individuals must be extremely careful to avoid infecting others during treatment. Typhoid fever can be prevented through vaccination for individuals traveling to parts of the world where it is common.
- Why is serotyping particularly important in Salmonella infections and typhoid fever?
EYE ON ETHICS: Typhoid Mary
Because she herself had never been ill, Mallon found it difficult to believe she could be the source of the illness. She fled from Soper and the authorities because she did not want to be quarantined or forced to give up her profession, which was relatively well paid for someone with her background. However, Mallon was eventually caught and kept in an isolation facility in the Bronx, where she remained until 1910, when the New York health department released her under the condition that she never again work with food. Unfortunately, Mallon did not comply, and she soon began working as a cook again. After new cases began to appear that resulted in the death of two individuals, the authorities tracked her down again and returned her to isolation, where she remained for 23 more years until her death in 1938. Epidemiologists were able to trace 51 cases of typhoid fever and three deaths directly to Mallon, who is unflatteringly remembered as “Typhoid Mary.”
The Typhoid Mary case has direct correlations in the health-care industry. Consider Kaci Hickox, an American nurse who treated Ebola patients in West Africa during the 2014 epidemic. After returning to the United States, Hickox was quarantined against her will for three days and later found not to have Ebola. Hickox vehemently opposed the quarantine. In an editorial published in the British newspaper The Guardian,[3] Hickox argued that quarantining asymptomatic health-care workers who had not tested positive for a disease would not only prevent such individuals from practicing their profession, but discourage others from volunteering to work in disease-ridden areas where health-care workers are desperately needed.
What is the responsibility of an individual like Mary Mallon to change her behaviour to protect others? What happens when an individual believes that she is not a risk, but others believe that she is? How would you react if you were in Mallon’s shoes and were placed in a quarantine you did not believe was necessary, at the expense of your own freedom and possibly your career? Would it matter if you were definitely infected or not?
E. coli Infections
The gram-negative rod Escherichia coli is a common member of the normal microbiota of the colon. Although the vast majority of E. coli strains are helpful commensal bacteria, some can be pathogenic and may cause dangerous diarrhoeal disease. The pathogenic strains have additional virulence factors such as type 1 fimbriae that promote colonization of the colon or may produce toxins (see Virulence Factors of Bacterial and Viral Pathogens). These virulence factors are acquired through horizontal gene transfer.
Extra-intestinal disease can result if the bacteria spread from the gastrointestinal tract. Although these bacteria can be spread from person to person, they are often acquired through contaminated food or water. There are six recognized pathogenic groups of E. coli, but we will focus here on the four that are most commonly transmitted through food and water.
Enterotoxigenic E. coli (ETEC), also known as traveler’s diarrhoea, causes diarrhoeal illness and is common in less developed countries. In Mexico, ETEC infection is called Montezuma’s Revenge. Following ingestion of contaminated food or water, infected individuals develop a watery diarrhoea, abdominal cramps, malaise (a feeling of being unwell), and a low fever. ETEC produces a heat-stable enterotoxin similar to cholera toxin, and adhesins called colonization factors that help the bacteria to attach to the intestinal wall. Some strains of ETEC also produce heat-labile toxins. The disease is usually relatively mild and self-limiting. Diagnosis involves culturing and PCR. If needed, antibiotic treatment with fluoroquinolones, doxycycline, rifaximin, and trimethoprim-sulfamethoxazole (TMP/SMZ) may shorten infection duration. However, antibiotic resistance is a problem.
Enteroinvasive E. coli (EIEC) is very similar to shigellosis, including its pathogenesis of intracellular invasion into intestinal epithelial tissue. This bacterium carries a large plasmid that is involved in epithelial cell penetration. The illness is usually self-limiting, with symptoms including watery diarrhoea, chills, cramps, malaise, fever, and dysentery. Culturing and PCR testing can be used for diagnosis. Antibiotic treatment is not recommended, so supportive therapy is used if needed.
Enteropathogenic E. coli (EPEC) can cause a potentially fatal diarrhoea, especially in infants and those in less developed countries. Fever, vomiting, and diarrhoea can lead to severe dehydration. These E. coli inject a protein (Tir) that attaches to the surface of the intestinal epithelial cells and triggers rearrangement of host cell actin from microvilli to pedestals. Tir also happens to be the receptor for Intimin, a surface protein produced by EPEC, thereby allowing E. coli to “sit” on the pedestal. The genes necessary for this pedestal formation are encoded on the locus for enterocyte effacement (LEE) pathogenicity island. As with ETEC, diagnosis involves culturing and PCR. Treatment is similar to that for ETEC.
The most dangerous strains are enterohaemorrhagic E. coli (EHEC), which are the strains capable of causing epidemics. In particular, the strain O157:H7 has been responsible for several recent outbreaks. Recall that the O and H refer to surface antigens that contribute to pathogenicity and trigger a host immune response (“O” refers to the O-side chain of the lipopolysaccharide and the “H” refers to the flagella). Similar to EPEC, EHEC also forms pedestals. EHEC also produces a Shiga-like toxin. Because the genome of this bacterium has been sequenced, it is known that the Shiga toxin genes were most likely acquired through transduction (horizontal gene transfer). The Shiga toxin genes originated from Shigella dysenteriae. Prophage from a bacteriophage that previously infected Shigella integrated into the chromosome of E. coli. The Shiga-like toxin is often called verotoxin.
EHEC can cause disease ranging from relatively mild to life-threatening. Symptoms include bloody diarrhoea with severe cramping, but no fever. Although it is often self-limiting, it can lead to haemorrhagic colitis and profuse bleeding. One possible complication is HUS. Diagnosis involves culture, often using MacConkey with sorbitol agar to differentiate between E. coli O157:H7, which does not ferment sorbitol, and other less virulent strains of E. coli that can ferment sorbitol.
Serological typing or PCR testing also can be used, as well as genetic testing for Shiga toxin. To distinguish EPEC from EHEC, because they both form pedestals on intestinal epithelial cells, it is necessary to test for genes encoding for both the Shiga-like toxin and for the LEE. Both EPEC and EHEC have LEE, but EPEC lacks the gene for Shiga toxin. Antibiotic therapy is not recommended and may worsen HUS because of the toxins released when the bacteria are killed, so supportive therapies must be used. Table 25.2 summarizes the characteristics of the four most common pathogenic groups.
Table 25.2. Some Pathogenic Groups of E. coli
| Group | Virulence Factors and Genes | Signs and Symptoms | Diagnostic Tests | Treatment |
|---|---|---|---|---|
| Enterotoxigenic E. coli (ETEC) | Heat stable enterotoxin similar to cholera toxin | Relatively mild, watery diarrhoea | Culturing, PCR | Self-limiting; if needed, fluoroquinolones, doxycycline, rifaximin, TMP/SMZ; antibiotic resistance is a problem |
| Enteroinvasive E. coli (EIEC) | Inv (invasive plasmid) genes | Relatively mild, watery diarrhoea; dysentery or inflammatory colitis may occur | Culturing, PCR; testing for inv gene; additional assays to distinguish from Shigella | Supportive therapy only; antibiotics not recommended |
| Enteropathogenic E. coli (EPEC) | Locus of enterocyte effacement (LEE) pathogenicity island | Severe fever, vomiting, nonbloody diarrhoea, dehydration; potentially fatal | Culturing, PCR; detection of LEE lacking Shiga-like toxin genes | Self-limiting; if needed, fluoroquinolones, doxycycline, rifaximin (TMP/SMZ); antibiotic resistance is a problem |
| Enterohaemorrhagic E. coli (EHEC) | Verotoxin | May be mild or very severe; bloody diarrhoea; may result in HUS | Culturing; plate on MacConkey agar with sorbitol agar as it does not ferment sorbitol; PCR detection of LEE containing Shiga-like toxin genes | Antibiotics are not recommended due to the risk of HUS |
- Compare and contrast the virulence factors and signs and symptoms of infections with the four main E. coli groups.
Cholera and Other Vibrios
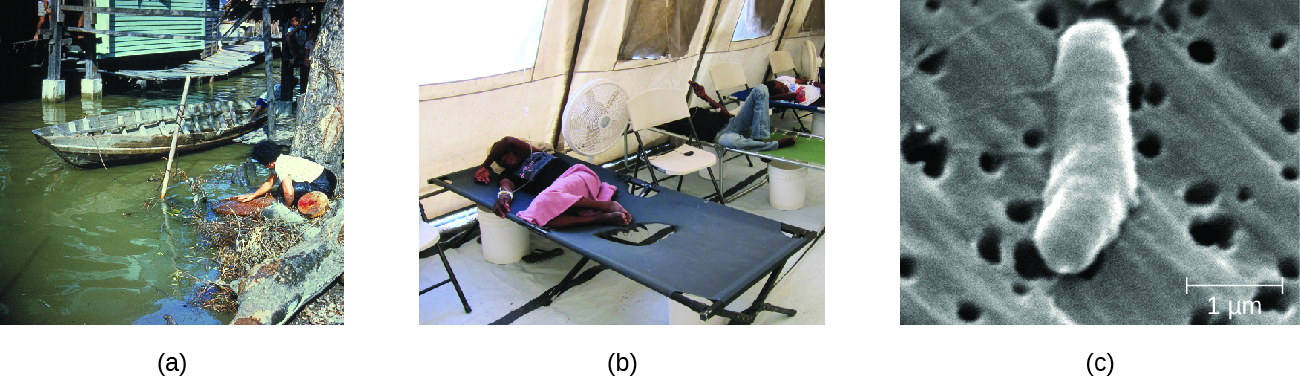
The gastrointestinal disease cholera is a serious infection often associated with poor sanitation, especially following natural disasters, because it is spread through contaminated water and food that has not been heated to temperatures high enough to kill the bacteria. It is caused by Vibrio cholerae serotype O1, a gram-negative, flagellated bacterium in the shape of a curved rod (vibrio). According to the CDC, cholera causes an estimated 3 to 5 million cases and 100,000 deaths each year.[4]
Because V. cholerae is killed by stomach acid, relatively large doses are needed for a few microbial cells to survive to reach the intestines and cause infection. The motile cells travel through the mucous layer of the intestines, where they attach to epithelial cells and release cholera enterotoxin. The toxin is an A-B toxin with activity through adenylate cyclase (see Virulence Factors of Bacterial and Viral Pathogens). Within the intestinal cell, cyclic AMP (cAMP) levels increase, which activates a chloride channel and results in the release of ions into the intestinal lumen. This increase in osmotic pressure in the lumen leads to water also entering the lumen. As the water and electrolytes leave the body, it causes rapid dehydration and electrolyte imbalance. Diarrhea is so profuse that it is often called “rice water stool,” and patients are placed on cots with a hole in them to monitor the fluid loss (Figure 25.18).
Cholera is diagnosed by taking a stool sample and culturing for Vibrio. The bacteria are oxidase positive and show non-lactose fermentation on MacConkey agar. Gram-negative lactose fermenters will produce red colonies while non-fermenters will produce white/colourless colonies. Gram-positive bacteria will not grow on MacConkey. Lactose fermentation is commonly used for pathogen identification because the normal microbiota generally ferments lactose while pathogens do not. V. cholerae may also be cultured on thiosulphate citrate bile salts sucrose (TCBS) agar, a selective and differential media for Vibrio spp., which produce a distinct yellow colony.
Cholera may be self-limiting and treatment involves rehydration and electrolyte replenishment. Although antibiotics are not typically needed, they can be used for severe or disseminated disease. Tetracyclines are recommended, but doxycycline, erythromycin, orfloxacin, ciprofloxacin, and TMP/SMZ may be used. Recent evidence suggests that azithromycin is also a good first-line antibiotic. Good sanitation—including appropriate sewage treatment, clean supplies for cooking, and purified drinking water—is important to prevent infection (Figure 25.18)
V. cholera is not the only Vibrio species that can cause disease. V. parahemolyticus is associated with consumption of contaminated seafood and causes gastrointestinal illness with signs and symptoms such as watery diarrhoea, nausea, fever, chills, and abdominal cramps. The bacteria produce a heat-stable haemolysin, leading to dysentery and possible disseminated disease. It also sometimes causes wound infections. V. parahemolyticus is diagnosed using cultures from blood, stool, or a wound. As with V. cholera, selective medium (especially TCBS agar) works well. Tetracycline and ciprofloxacin can be used to treat severe cases, but antibiotics generally are not needed.
Vibrio vulnificus is found in warm seawater and, unlike V. cholerae, is not associated with poor sanitary conditions. The bacteria can be found in raw seafood, and ingestion causes gastrointestinal illness. It can also be acquired by individuals with open skin wounds who are exposed to water with high concentrations of the pathogen. In some cases, the infection spreads to the bloodstream and causes septicaemia. Skin infection can lead to oedema, ecchymosis (discolouration of skin due to bleeding), and abscesses. Patients with underlying disease have a high fatality rate of about 50%. It is of particular concern for individuals with chronic liver disease or who are otherwise immunodeficient because a healthy immune system can often prevent infection from developing. V. vulnificus is diagnosed by culturing for the pathogen from stool samples, blood samples, or skin abscesses. Adult patients are treated with doxycycline combined with a third generation cephalosporin or with fluoroquinolones, and children are treated with TMP/SMZ.
Two other vibrios, Aeromonas hydrophila and Plesiomonas shigelloides, are also associated with marine environments and raw seafood; they can also cause gastroenteritis. Like V. vulnificus, A. hydrophila is more often associated with infections in wounds, generally those acquired in water. In some cases, it can also cause septicaemia. Other species of Aeromonas can cause illness. P. shigelloides is sometimes associated with more serious systemic infections if ingested in contaminated food or water. Culture can be used to diagnose A. hydrophila and P. shigelloides infections, for which antibiotic therapy is generally not needed. When necessary, tetracycline and ciprofloxacin, among other antibiotics, may be used for treatment of A. hydrophila, and fluoroquinolones and trimethoprim are the effective treatments for P. shigelloides.
- How does V. cholera infection cause rapid dehydration?
Campylobacter jejuni Gastroenteritis
Campylobacter is a genus of gram-negative, spiral or curved bacteria. They may have one or two flagella. Campylobacter jejuni gastroenteritis, a form of campylobacteriosis, is a widespread illness that is caused by Campylobacter jejuni. The primary route of transmission is through poultry that becomes contaminated during slaughter. Handling of the raw chicken in turn contaminates cooking surfaces, utensils, and other foods. Unpasteurized milk or contaminated water are also potential vehicles of transmission. In most cases, the illness is self-limiting and includes fever, diarrhoea, cramps, vomiting, and sometimes dysentery. More serious signs and symptoms, such as bacteraemia, meningitis, pancreatitis, cholecystitis, and hepatitis, sometimes occur. It has also been associated with autoimmune conditions such as Guillain-Barré syndrome, a neurological disease that occurs after some infections and results in temporary paralysis. HUS following infection can also occur. The virulence in many strains is the result of haemolysin production and the presence of Campylobacter cytolethal distending toxin (CDT), a powerful deoxyribonuclease (DNase) that irreversibly damages host cell DNA.
Diagnosis involves culture under special conditions, such as elevated temperature, low oxygen tension, and often medium supplemented with antimicrobial agents. These bacteria should be cultured on selective medium (such as Campy CV, charcoal selective medium, or cefaperazone charcoal deoxycholate agar) and incubated under microaerophilic conditions for at least 72 hours at 42 °C. Antibiotic treatment is not usually needed, but erythromycin or ciprofloxacin may be used.
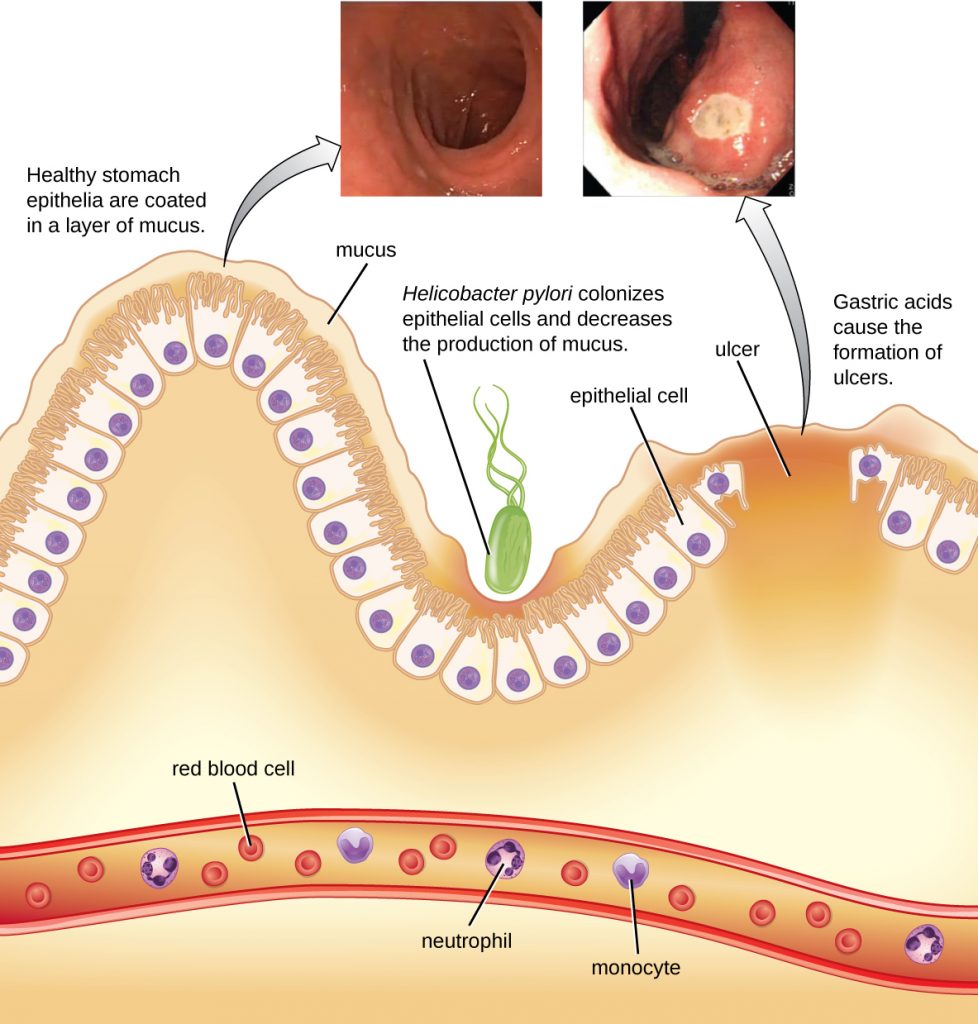
Peptic Ulcers
The gram-negative bacterium Helicobacter pylori is able to tolerate the acidic environment of the human stomach and has been shown to be a major cause of peptic ulcers, which are ulcers of the stomach or duodenum. The bacterium is also associated with increased risk of stomach cancer (Figure 25.19). According to the CDC, approximately two-thirds of the population is infected with H. pylori, but less than 20% have a risk of developing ulcers or stomach cancer. H. pylori is found in approximately 80% of stomach ulcers and in over 90% of duodenal ulcers.[5]
H. pylori colonizes epithelial cells in the stomach using pili for adhesion. These bacteria produce urease, which stimulates an immune response and creates ammonia that neutralizes stomach acids to provide a more hospitable microenvironment. The infection damages the cells of the stomach lining, including those that normally produce the protective mucus that serves as a barrier between the tissue and stomach acid. As a result, inflammation (gastritis) occurs and ulcers may slowly develop. Ulcer formation can also be caused by toxin activity. It has been reported that 50% of clinical isolates of H. pylori have detectable levels of exotoxin activity in vitro.[6] This toxin, VacA, induces vacuole formation in host cells. VacA has no primary sequence homology with other bacterial toxins, and in a mouse model, there is a correlation between the presence of the toxin gene, the activity of the toxin, and gastric epithelial tissue damage.
Signs and symptoms include nausea, lack of appetite, bloating, burping, and weight loss. Bleeding ulcers may produce dark stools. If no treatment is provided, the ulcers can become deeper, more tissues can be involved, and stomach perforation can occur. Because perforation allows digestive enzymes and acid to leak into the body, it is a very serious condition.
To diagnose H. pylori infection, multiple methods are available. In a breath test, the patient swallows radio-labeled urea. If H. pylori is present, the bacteria will produce urease to break down the urea. This reaction produces radio-labeled carbon dioxide that can be detected in the patient’s breath. Blood testing can also be used to detect antibodies to H. pylori. The bacteria themselves can be detected using either a stool test or a stomach wall biopsy.
Antibiotics can be used to treat the infection. However, unique to H. pylori, the recommendation from the US Food and Drug Administration is to use a triple therapy. The current protocols are 10 days of treatment with omeprazole, amoxicillin, and clarithromycin (OAC); 14 days of treatment with bismuth subsalicylate, metronidazole, and tetracycline (BMT); or 10 or 14 days of treatment with lansoprazole, amoxicillin, and clarithromycin (LAC). Omeprazole, bismuth subsalicylate, and lansoprazole are not antibiotics but are instead used to decrease acid levels because H. pylori prefers acidic environments.
Although treatment is often valuable, there are also risks to H. pylori eradication. Infection with H. pylori may actually protect against some cancers, such as esophageal adenocarcinoma and gastroesophageal reflux disease.[7][8]
- How does H. pylori cause peptic ulcers?
Clostridium perfringens Gastroenteritis
Clostridium perfringens gastroenteritis is a generally mild food-borne disease that is associated with undercooked meats and other foods. C. perfringens is a gram-positive, rod-shaped, endospore-forming anaerobic bacterium that is tolerant of high and low temperatures. At high temperatures, the bacteria can form endospores that will germinate rapidly in foods or within the intestine. Food poisoning by type A strains is common. This strain always produces an enterotoxin, sometimes also present in other strains, that causes the clinical symptoms of cramps and diarrhoea. A more severe form of the illness, called pig-bel or enteritis necroticans, causes hemorrhaging, pain, vomiting, and bloating. Gangrene of the intestines may result. This form has a high mortality rate but is rare in the United States.
Diagnosis involves detecting the C. perfringens toxin in stool samples using either molecular biology techniques (PCR detection of the toxin gene) or immunology techniques (ELISA). The bacteria itself may also be detected in foods or in faecal samples. Treatment includes rehydration therapy, electrolyte replacement, and intravenous fluids. Antibiotics are not recommended because they can damage the balance of the microbiota in the gut, and there are concerns about antibiotic resistance. The illness can be prevented through proper handling and cooking of foods, including prompt refrigeration at sufficiently low temperatures and cooking food to a sufficiently high temperature.
Clostridium difficile
Clostridium difficile is a gram-positive rod that can be a commensal bacterium as part of the normal microbiota of healthy individuals. When the normal microbiota is disrupted by long-term antibiotic use, it can allow the overgrowth of this bacterium, resulting in antibiotic-associated diarrhoea caused by C. difficile. Antibiotic-associated diarrhoea can also be considered a nosocomial disease. Patients at the greatest risk of C. difficile infection are those who are immunocompromised, have been in health-care settings for extended periods, are older, have recently taken antibiotics, have had gastrointestinal procedures done, or use proton pump inhibitors, which reduce stomach acidity and allow proliferation of C. difficile. Because this species can form endospores, it can survive for extended periods of time in the environment under harsh conditions and is a considerable concern in health-care settings.
This bacterium produces two toxins, Clostridium difficile toxin A (TcdA) and Clostridium difficile toxin B (TcdB). These toxins inactivate small GTP-binding proteins, resulting in actin condensation and cell rounding, followed by cell death. Infections begin with focal necrosis, then ulceration with exudate, and can progress to pseudomembranous colitis, which involves inflammation of the colon and the development of a pseudomembrane of fibrin containing dead epithelial cells and leukocytes (Figure 25.20). Watery diarrhoea, dehydration, fever, loss of appetite, and abdominal pain can result. Perforation of the colon can occur, leading to septicaemia, shock, and death. C. difficile is also associated with necrotizing enterocolitis in premature babies and neutropenic enterocolitis associated with cancer therapies.
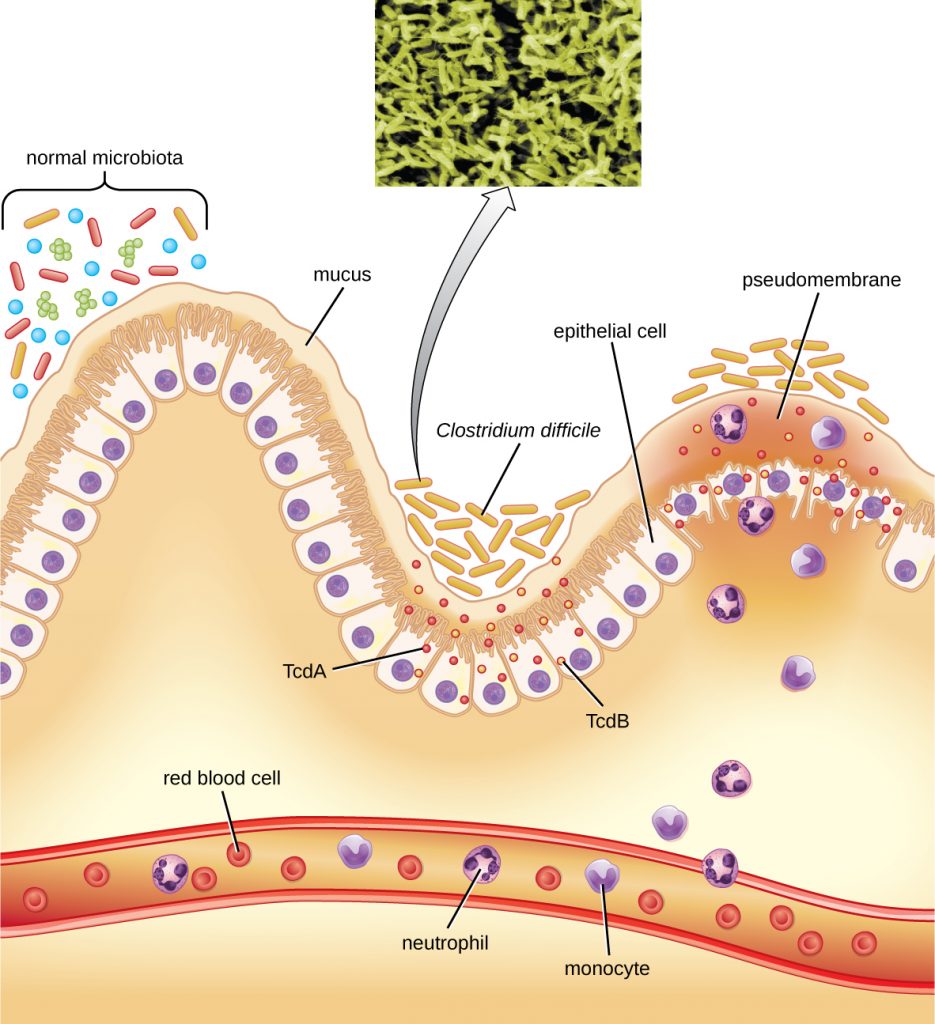
Diagnosis is made by considering the patient history (such as exposure to antibiotics), clinical presentation, imaging, endoscopy, lab tests, and other available data. Detecting the toxin in stool samples is used to confirm diagnosis. Although culture is preferred, it is rarely practical in clinical practice because the bacterium is an obligate anaerobe. Nucleic acid amplification tests, including PCR, are considered preferable to ELISA testing for molecular analysis.
The first step of conventional treatment is to stop antibiotic use, and then to provide supportive therapy with electrolyte replacement and fluids. Metronidazole is the preferred treatment if the C. difficile diagnosis has been confirmed. Vancomycin can also be used, but it should be reserved for patients for whom metronidazole was ineffective or who meet other criteria (e.g., under 10 years of age, pregnant, or allergic to metronidazole).
A newer approach to treatment, known as a faecal transplant, focuses on restoring the microbiota of the gut in order to combat the infection. In this procedure, a healthy individual donates a stool sample, which is mixed with saline and transplanted to the recipient via colonoscopy, endoscopy, sigmoidoscopy, or enema. It has been reported that this procedure has greater than 90% success in resolving C. difficile infections.[9]
- How does antibiotic use lead to C. difficile infections?
Foodborne Illness Due to Bacillus cereus
Bacillus cereus, commonly found in soil, is a gram-positive endospore-forming bacterium that can sometimes cause food-borne illness. B. cereus endospores can survive cooking and produce enterotoxins in food after it has been heated; illnesses often occur after eating rice and other prepared foods left at room temperature for too long. The signs and symptoms appear within a few hours of ingestion and include nausea, pain, and abdominal cramps. B. cereus produces two toxins: one causing diarrhoea, and the other causing vomiting. More severe signs and symptoms can sometimes develop.
Diagnosis can be accomplished by isolating bacteria from stool samples or vomitus and uneaten infected food. Treatment involves rehydration and supportive therapy. Antibiotics are not typically needed, as the illness is usually relatively mild and is due to toxin activity.
Foodborne Illness Due to Yersinia
The genus Yersinia is best known for Yersinia pestis, a gram-negative rod that causes the plague. However, Y. enterocolitica and Y. pseudotuberculosis can cause gastroenteritis. The infection is generally transmitted through the faecal-oral route, with ingestion of food or water that has been contaminated by faeces. Intoxication can also result because of the activity of its endotoxin and exotoxins (enterotoxin and cytotoxin necrotizing factor). The illness is normally relatively mild and self-limiting. However, severe diarrhoea and dysentery can develop in infants. In adults, the infection can spread and cause complications such as reactive arthritis, thyroid disorders, endocarditis, glomerulonephritis, eye inflammation, and/or erythema nodosum. Bacteraemia may develop in rare cases.
Diagnosis is generally made by detecting the bacteria in stool samples. Samples may also be obtained from other tissues or body fluids. Treatment is usually supportive, including rehydration, without antibiotics. If bacteraemia or other systemic disease is present, then antibiotics such as fluoroquinolones, aminoglycosides, doxycycline, and trimethoprim-sulfamethoxazole may be used. Recovery can take up to two weeks.
- Compare and contrast food-borne illnesses due to B. cereus and Yersinia.
DISEASE PROFILE: Bacterial Infections of the Gastrointestinal Tract
Bacterial infections of the gastrointestinal tract generally occur when bacteria or bacterial toxins are ingested in contaminated food or water. Toxins and other virulence factors can produce gastrointestinal inflammation and general symptoms such as diarrhoea and vomiting. Bacterial GI infections can vary widely in terms of severity and treatment. Some can be treated with antibiotics, but in other cases antibiotics may be ineffective in combating toxins or even counterproductive if they compromise the GI microbiota. Table 25.2 summarizes the key features of common bacterial GI infections.
Table 25.2. Bacterial Infections of the GI Tract
CLINICAL FOCUS: Part 2
At the hospital, Carli’s doctor began to think about possible causes of her severe gastrointestinal distress. One possibility was food poisoning, but no one else in her family was sick. The doctor asked about what Carli had eaten the previous day; her mother mentioned that she’d had eggs for lunch, and that they may have been a little undercooked. The doctor took a sample of Carli’s stool and sent it for laboratory testing as part of her workup. She suspected that Carli could have a case of bacterial or viral gastroenteritis, but she needed to know the cause in order to prescribe an appropriate treatment.
In the laboratory, technicians microscopically identified gram-negative bacilli in Carli’s stool sample. They also established a pure culture of the bacteria and analyzed it for antigens. This testing showed that the causative agent was Salmonella.
- What should the doctor do now to treat Carli?
Jump to the next Clinical Focus box. Go back to the previous Clinical Focus box.
Key Takeaways
- Major causes of gastrointestinal illness include Salmonella spp., Staphylococcus spp., Helicobacter pylori, Clostridium perfringens, Clostridium difficile, Bacillus cereus, and Yersinia bacteria.
- C. difficile is an important cause of hospital acquired infection.
- Vibrio cholerae causes cholera, which can be a severe diarrhoeal illness.
- Different strains of E. coli, including ETEC, EPEC, EIEC, and EHEC, cause different illnesses with varying degrees of severity.
- H. pylori is associated with peptic ulcers.
- Salmonella enterica serotypes can cause typhoid fever, a more severe illness than salmonellosis.
- Rehydration and other supportive therapies are often used as general treatments.
- Careful antibiotic use is required to reduce the risk of causing C. difficile infections and when treating antibiotic-resistant infections.
Multiple Choice
Fill in the Blank
Critical Thinking
- Why does use of antibiotics and/or proton pump inhibitors contribute to the development of C. difficile infections?
- Why did scientists initially think it was unlikely that a bacterium caused peptic ulcers?
- Does it makes a difference in treatment to know if a particular illness is caused by a bacterium (an infection) or a toxin (an intoxication)?
Media Attributions
- OSC_Microbio_24_03_DangerZone
- OSC_Microbio_24_03_Shigella
- OSC_Microbio_24_03_Salmonella
- OSC_Microbio_24_03_VibrioChol
- OSC_Microbio_24_03_Ulcers
- OSC_Microbio_24_03_pseudocoli
- Jaya Sureshbabu. “Shigella Infection Workup.” Medscape. Updated Jun 28, 2016. http://emedicine.medscape.com/article/968773-workup. ↵
- Centers for Disease Control and Prevention. Salmonella. Updated August 25, 2016. https://www.cdc.gov/salmonella. ↵
- Kaci Hickox. “Stop Calling Me the ‘Ebola Nurse.’” The Guardian. November 17, 2014. http://www.theguardian.com/commentisfree/2014/nov/17/stop-calling-me-ebola-nurse-kaci-hickox. ↵
- Centers for Disease Control and Prevention. Cholera—Vibrio cholerae Infection. Updated November 6, 2014. http://www.cdc.gov/cholera/general. Accessed May 14, 2019. ↵
- Centers for Disease Control and Prevention. “Helicobacter pylori: Fact Sheet for Health Care Providers.” Updated July 1998. http://www.cdc.gov/ulcer/files/hpfacts.pdf. ↵
- T. L. Cover. “The Vacuolating Cytotoxin of Helicobacter pylori.” Molecular Microbiology 20 (1996) 2: pp. 241–246. http://www.ncbi.nlm.nih.gov/pubmed/8733223. ↵
- Martin J. Blaser. “Disappearing Microbiota: Helicobacter pylori Protection against Esophageal Adenocarcinoma.” Cancer Prevention Research 1 (2008) 5: pp. 308–311. http://cancerpreventionresearch.aacrjournals.org/content/1/5/308.full.pdf+html. ↵
- Ivan F. N. Hung and Benjamin C. Y. Wong. “Assessing the Risks and Benefits of Treating Helicobacter pylori Infection.” Therapeutic Advances in Gastroenterology 2 (2009) 3: pp, 141–147. doi: 10.1177/1756283X08100279. ↵
- Faith Rohlke and Neil Stollman. “Fecal Microbiota Transplantation in Relapsing Clostridium difficile Infection,” Therapeutic Advances in Gastroenterology 5 (2012) 6: 403–420. doi: 10.1177/1756283X12453637. ↵

