Documentation
Wound documentation is a valuable process that helps clinicians to monitor the progress of a wound. Newer technology and point of care innovations have paved the way for documentation using wound photography, digital measurements, and electronic health records. Electronic wound documentation platforms also allow for real-time reporting. (See Figure 1). Wound assessment parameters should be documented in a consistent format to facilitate comparison and communication to team members. This begins with a comprehensive patient and wound history, along with a detailed wound assessment.
Table 1 – Sample of a Wound Electronic Documentation (Humber River Hospital, 2021). Used with Permission.
| Drainage Amount | None Small (Scant) Moderate Large |
|---|---|
| Wound Drainage | |
| Drainage Description | Serous Sanguinneous Serosanquinneous Purulent (yellow, green or brown) Seropurulent Other – if selected, specify |
| Other (Specified) | |
| Periwound / Edge Assessment | |
| Periwound/Edge | Intact Excoriated Rolled Bleeding Induration Undermining/Tunneling Dry Macerated |
| Signs of Infection | |
| Signs of Superficial Infection | Non-healing Debris Exudate Increased Smell Red & Bleeding (Friable) |
| *** 3 or More, Use Topical Antimicrobial*** | |
| Signs of deep and Surrounding Tissue | Size is Larger Exudate Increased Temperature Increased Erydate and Edema Exposed or Probe to Bone Smell New Breakdown |
| Wound Measurement | |
| Length (cm) | |
| Width (cm) | |
| Area (cm) | |
| Depth (cm) |
When assessing a wound, the specific location should be identified and documented e.g. left heel, coccyx, right gluteal fold or lower leg. Often, multiple wounds may also be present in one location at a time. Wound cleansing should be preformed prior to wound assessment for improved visualization of the wound bed in its natural state. When wound debridement occurs, wound measurements should be recorded both pre and post debridement.
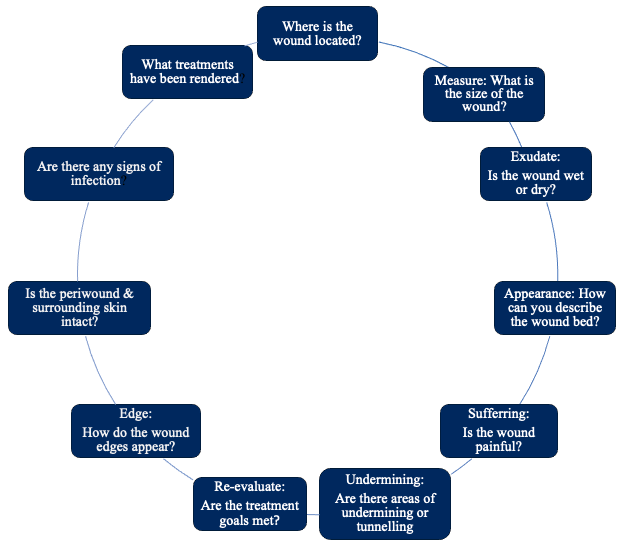
The MEASURE mnemonic is a well accepted framework for detailed wound assessment (Keast et al, 2004). Other validated assessment tools include the Bates-Jensen Wound Assessment Tool or Pressure Ulcer Scale for Healing.
Figure 2 – Additional factors to consider for wound assessment