Moisture Management for Maintenance Wounds
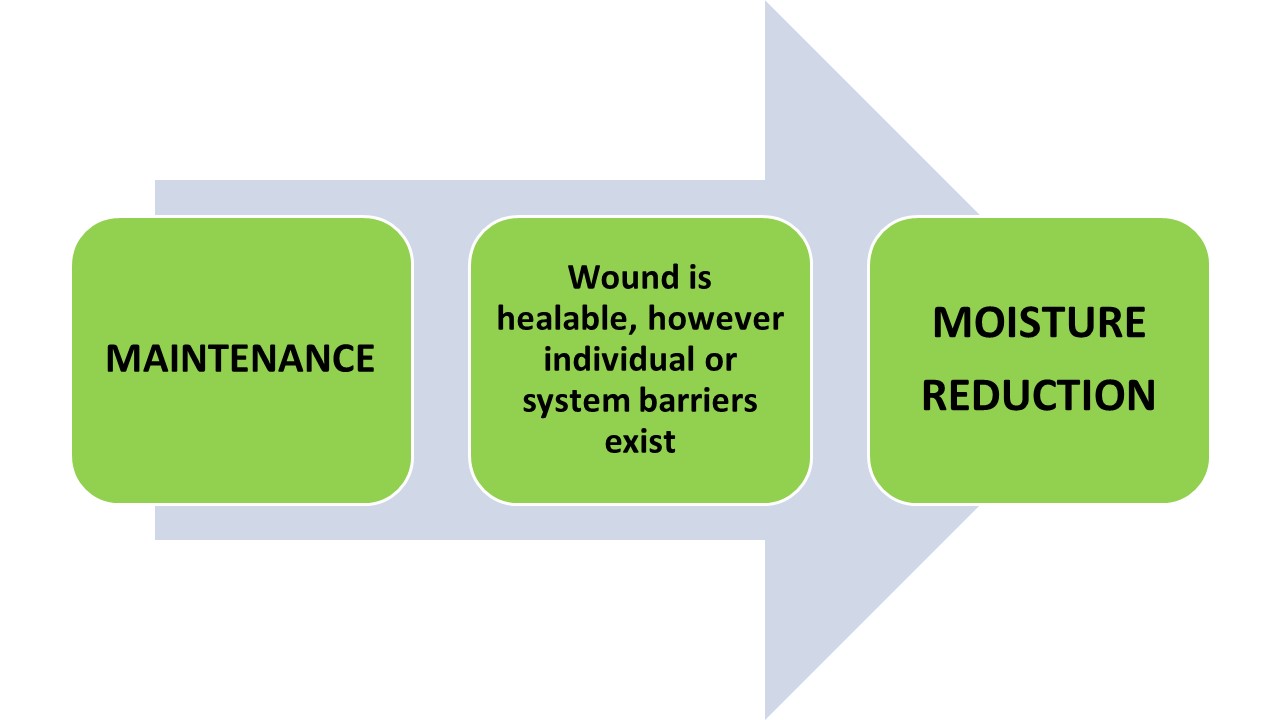
Figure 3. Moisture Management for Maintenance Wounds (Goodman, 2021)
The cautious and similar approach used for nonhealable wounds should be also taken for maintenance wounds. These wounds usually have adequate arterial blood supply, are free of malignancy and should ideally progress to healing however individual and/or system challenges prevent the healing. Some common examples to illustrate the maintenance wound include:
- An individual with longstanding chronic venous leg edema and subsequent lower leg ulcers, confirmed adequate arterial blood supply however refuses to wear compression therapy. Other individuals may have the compression bandages for treatment provided through home services. Lack of financial resources to purchase the compression stockings ongoing for years may result in maintenance wounds with frequent recurrences.
- An individual with neurotrophic foot ulcer has confirmed adequate arterial blood supply, requires plantar pressure redistribution, is willing to wear the offloading device however cannot afford the purchase of the specialized footwear. They have no extended benefits or financial resources. This is a maintenance wound.
- A paraplegic individual with chronic pressure injuries to ischial tuberosities uses a wheelchair for mobility. The wounds have nearly closed on several occasions but the individual has a pattern of occasional excessive alcohol and tobacco use for a few weeks at time. During these binges the wounds deteriorate rapidly. The team has repeatedly educated the patient on the impact these binges have on wound healing, the risks of infection, sepsis and possibly death. This individual has repeatedly declined substance abuse counselling and therapy.
Once an individual with a maintenance wound is identified, using the correct approach for “moisture reduction” is key. It is by adequately reducing moisture that bacteria are thereby reduced, subsequentially decreasing the risk of potential infection, sepsis and death.
For a maintenance wound, the goal is to simply “maintain” a stable wound status and prevent infection (control edema, exudate). Goals are shifted to patient-centered concerns including the optimization of pain management and activities of daily living and healing is not the focus. Counselling the patient and / or their circle of care is needed as they accept that the wound may not heal. The inclusion of an interprofessional team is often advantageous to confirm that treatment elements are not overlooked.
Antiseptics are used for the purposes of moisture reduction and bacteria reduction for these individuals. Using these antiseptics, the benefit of reducing bacteria gains precedent over the potential risk of cytotoxicity to the wound bed.
As stated previously, healability classifications of wounds can change. For example, funding for the offloading boot or compression therapy may be obtained, smoking and alcohol use may discontinue. In these cases, the wound healing classification would move from maintenance status (requiring moisture reduction) to a healable wound (now requiring moisture balance). In some instances, maintenance wounds may still progress in a healing trajectory and close. It is through optimizing each individual risk and causative factor that could potentially tip the wound into a healing trajectory.

