Moisture Management for Nonhealable Wounds
Figure 2. Moisture Management for Nonhealable Wounds (Goodman, 2021)
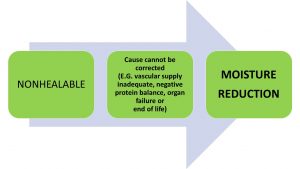
A cautious and conservative approach should be taken when wounds are identified as lacking the ability to heal. Lack of arterial blood supply (ischemia), malignancy with cutaneous metastasis, progressing non-treatable dermal disorders or end of life skin changes where the individual may be in a negative protein balance and multiple organ failure are some examples of a nonhealable wound. For these wounds, moisture reduction is key. By reducing the moisture levels on the wound surface, bacteria are thereby reduced, subsequentially decreasing the risk of potential infection. This is especially true when the host defence is weakened as in an immunocompromised individual.
In many cases with a nonhealable wound, the goal is to simply “maintain” a stable wound status and prevent infection. A case example would be a 90-year-old female on renal dialysis (end stage renal disease) with a non-operable ischemic foot. The foot presents as a black mummified, dry and stable necrotic state. Prevention of deep and surrounding tissue infection and sepsis is the goal and povidone iodine with a dry dressing was implemented. Extra diligence should be taken to have the antimicrobial solution applied to into the surface between the necrotic and non-narcotic tissue around the ankle to minimize the chance of tissue becoming moist and promoting bacteria spread. With this moisture reduction and control of bacterial growth, this individual could continue with their activities of every day life for weeks, months and possibly years.
In the case of the nonhealable wound, the goals of healing the wound are secondary. Instead, emphasis is shifted to patient-centered concerns including the optimization of pain management and activities of daily living. This often requires some counselling with the patient and / or their circle of care as this is may be new and uncharted waters as they realize the wound may not heal. Providing support through a trusting patient-to-caregiver relationship is needed. Unique goals from the patient and their circle of care should be prioritized, documented and shared with the interprofessional team.
The healability classification of wounds can change necessitating prompt treatment changes. An individual with a nonhealable ischemic foot may have revascularization surgery, ideally resulting with palpable pulses in this limb. The wound is no longer considered a nonhealable wound since the cause has been corrected. This requires a different moisture management approach by appropriate use of moist wound healing strategies, as the wound is now considered healable. Healing may be delayed with reperfusion injury.
Antiseptics applied topically are often used for the purposes of moisture reduction and bacteria reduction. Here, the goal of reducing bacteria takes priority and subsequent impact of cytotoxicity is less important. Antiseptic solutions vary in their degree of cytotoxicity. Antiseptics will be discussed later in the chapter.
Another case example in the nonhealable classification would be the common presentation of black necrotic heel caps for a frail elderly individual confined to bed. A monophasic pulse is determined by audible handheld doppler assessment and a weak pulse may be palpable. It was determined that this patient is not amenable for foot revascularization and tissue debridement would be considered to be contraindicated except to remove “non-viable slough” without causing bleeding. Painting the black eschar cap and surrounding skin with povidone iodine daily and keeping the heel open to air could be the safest and most appropriate approach for reducing moisture and bacteria. Other strategies would be to float the heel to reduce any causative pressure concerns. In many cases, these black heel caps over time may further desiccate, loosen and fall off with the slow healing process occurring under the cap.

