Statements 2 to 4
Statement 2 – Patient centered concerns
The patient should be at the center of their care. Management plans should be prepared, modified and adapted to the individual patient, taking into consideration their specific, unique needs and concerns. Sackett et al. (1996) stated that the practice of evidence based medicine includes scientific evidence, expert opinion and patient preference that should consider the patients’ rights and opinions (Sackett et al., 1996).
2a) Optimal pain management: Wound associated pain is a frequent source of distress for patients with chronic wounds. The intensity of wound pain can be high with any chronic wound but may be more evident depending on the wound etiology and aggravating factors (e.g., ischemic arterial ulcers or inflammatory ulcers including pyoderma gangrenosum). Pain is derived from two physiological pathways that require different and focused therapeutic management. Nociceptive pain occurs from tissue damage caused by trauma or injury (Mudge & Orsted, 2010). It is often acute and described as aching, throbbing, tender or gnawing (Sibbald et al., 2021). Neuropathic pain occurs as a result of damage to the nervous system, usually spontaneous and described as shooting, burning stinging or stabbing (Sibbald et al.,2021).
There are various causes of wound pain that are usually interrelated including pain (from the wound itself), external stimuli due to dressing changes, compression, and other local causes (edema, ischemia, skin disease) (Mudge & Orsted, 2010). It is essential to perform consistent and regular pain assessments for effective therapeutic interventions. These should be documented at every assessment. There are many validated tools that either qualitatively or quantitatively assess pain. They range from simple (the visual analog scale, numerical rating scale and pain faces scale) to more complex tools (including questionnaires and pain diaries) (Mudge & Orsted, 2010).
2b) Evaluate activities of daily living, exercise/mobility, psychological well-being, mental health, support system (circle of care, access to care, financial constraints). A patient centered approach addresses the patient as a whole and their circle of care. Many patients lack the social and financial support necessary to facilitate the chronic wound journey. Wound pain has many debilitating effects and has been shown to reduce activities of daily living, often measured indirectly with quality of life assessment tools (Woo & Sibbald, 2008). Mental health and psychosocial wellbeing should be addressed. Many patients have difficulty coping with the chronicity of some wounds and other factors including copious exudate, excessive odour, negative body image and social isolation. Healthcare system factors including accessibility to care need to be assessed as these directly impact clinical outcomes. Therefore, clinicians should advocate for their patients and tailor treatment plans to accommodate the patient and their unique situation.
2c) Evaluate habits – smoking, alcohol, substance use, hygiene. Cigarette smoke affects the arterial endothelial function and decreases vascular supply by as much as 40%, producing ischemia and subsequently, affecting wound healing (Weller et al., 2021). Mechanisms to deal with smoking cessation and control of alcohol and substance abuse will facilitate wound healing but this often takes time and clinician patience as relapses are common.
2d) Empower patients with education and support to increase treatment adherence (coherence). Chronic wound care management is a collaborative effort that requires negotiation with the patient to include their perspective. This will increase subsequent adherence to the plan of care. These actions can include, but are not limited to, compression therapy, offloading devices, mobility/turning schedules, smoking cessation and adequate nutritional intake. It is important to explore the reasons why patients are non-adherent and plan strategies that align with both clinician and patient needs (Weller et al., 2021).
Statement 3 – Determine ability to heal
Wounds are classified into three categories based on their ability to heal: healable, maintenance and nonhealable (Sibbald et al., 2021).
3a) Healable wounds constitute approximately two-thirds of wounds seen in the community. For these wounds, the cause can be identified and corrected, and they follow the healing trajectory. Healing can take a variable period depending on the correct diagnosis and treatment, comorbidities and the patient’s adherence to the standard of care.
3b) Maintenance wounds occur in cases where the patient refuses to adhere to the treatment plan or there are health care system barriers, or both, that prevent the cause from being corrected. For example, a patient may refuse to use the recommended compression therapy that is vital for venous insufficiency ulcer to heal. Another example is when a patient refuses to wear appropriate footwear for the high-risk diabetic foot. For system barriers, chiropody services and offloading footwear are not covered by many health care systems including universal Ontario health care. Patients often cannot financially afford to pay for these much needed services necessary for neuropathic or ischemic ulcers often in persons with diabetes (Sibbald et al., 2011, 2021). The main approach for maintenance wounds is based on the fact that the wound is healable, but the appropriate treatment is either not attainable for system reasons or due to individual patient choices (patient non-adherence).
3c) Nonhealable wounds have inadequate blood supply or an underlying cause that cannot be corrected are classified as nonhealable wounds (e.g., due to unresponsive malignancy, critical ischemia) and account for 5-10% of all wounds. The priorities of care for these patients are not aimed at wound healing, but instead at maintaining quality of life, minimizing pain, exudate, odour, infection and facilitate continuation of activities of daily living (Sibbald et al., 2021). If the cause of the wound is corrected, the wound may change to a healable or maintenance healing classification.
Statement 4 – Local wound care: Wound history and clinical examination
4a) A comprehensive wound history and assessment is a pivotal aspect of wound care, thereby defining the status of the wound and establishing a baseline for subsequent assessments.
Local wound care interventions are then based on the ability to heal wound classification (healable, maintenance or nonhealable). Wound assessments and documentation should follow a standardized approach with consistent measurement units and parameters (Hess, 2019). The MEASURE mnemonic is a common tool used for wound assessments that describes specific wound parameters (Keast et al., 2004).
- Measure (length, width, depth, and area): Wound measurement techniques can vary. The most common method is using the longest length by the widest width perpendicular to each other with a wound ruler (some institutions also use the head-to-toe configuration). Another simple method includes wound tracing on calibrated acetate or transparent film. More technical methods include computer imagery, wound photography with digital tracing on mobile apps, etc. (Flanagan, 2003)
- Exudate (quantity and quality): Amount (none, scant, moderate, heavy) and characteristics should be documented (serous, sanguineous, pustular or combinations with the most predominant component stated first)
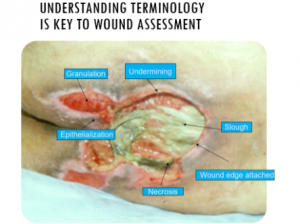
- Appearance: Wound bed including tissue type (black necrotic tissue, healthy firm pink granulation tissue , soft yellow to brown slough, new purple re-epithelialization) and their relative proportion of the wound surface
- Suffering: Wound pain score, pain type(s) and characteristics
- Undermining: Presence or absence; if present, assessed for using the hands of the clock to document (where the patient’s head direction signifies 12 o’clock and their feet being 6 o’clock)
- Reevaluate: Monitoring all parameters at regular intervals
- Edge: Condition of the edge and surrounding skin (rolled edges, maceration, thick callus, dryness, erythema, edema)
Figure 2 Wound Bed Appearance: Courtesy of Sharon Baranoski
Precise and standardized wound assessments are vital for monitoring the progress of wound healing and early identification of wounds that are stalled or deteriorating with interventions. This is necessary to correct factors that are impeding wound healing and avoid unnecessary use of advanced modalities (Flanagan, 2003). Wounds that are nonhealable are ideally identified early. Various studies in reduction of surface area of different wound etiologies concur that a surface area reduction of 20-30% at week 4 is a good predictor for healing at week 12 (Chronic Wounds and Delayed Healing Risk, 2010; Flanagan, 2003; Sheehan et al., 2003). Wound assessments and individualized care plans should be accurately documented and communicated to the patient and their circle of care.
4b) Gently cleanse the wound with low toxicity solutions (water, saline, antiseptic agents). The cleansing solution used depends on the characteristics of the wound and availability in practice. There is poor consensus in the literature on wound cleansing recommendations. An updated 2021 Cochrane review on cleansing solutions of venous leg ulcers concluded that there is a “lack of RCT evidence to guide decision making about the effectiveness of wound cleansing compared with no cleansing and the optimal approaches to cleansing of venous leg ulcers” (McLain et al., 2021). However, general wound care principles recommend using low toxicity solutions such as water, saline and other skin friendly antiseptic agents (Sibbald et al., 2011). This avoids cytotoxic effects and damage to healthy granulation tissue. Acetic acid (diluted to 0.5-1.0%) or hypochlorous acid can also be used in some cases where an acidic environment is preferred (e.g., used to topically treat species of pseudomonas) (Block & Rowan, 2020). Based on the healing classification of the wound, antiseptic agents with some tissue cytotoxicity may be used with a benefit versus risk scenario [low concentration chlorhexidine or its derivative polyhexamethylene biguanide (PHMB) or povidone iodine]. This may be in the cases of maintenance and nonhealable wounds that have a high potential for infection where these agents can be used to manage odour, exudate, and control bioburden. See Table 3. Wound irrigation is also a controversial topic. However, expert opinion recommends that wounds should not be irrigated if the base of the wound is not visible to avoid accumulation of the irrigation solution in closed spaces (Sibbald et al., 2011).
Table 3. Common antiseptic agents for use in nonhealable wounds. Cytotoxicity is less important than antimicrobial action.
| AGENT | TOXICITY | EFFECTS |
|---|---|---|
| Chlorhexidine (PHMB) | • Low | • Neutral, non-release • Does not treat wound surface • Kills bacterial cell wall – no bacteria left for resistance |
| Povidone Iodine | • Low • Less toxic with slow-release formulations |
• Pro-inflammatory • Treats wound surface • Broad spectrum • Good penetration of biofilm glycocalyx |
| Acetic Acid (diluted to 0.5-1.0%) Hypochlorous Acid |
• Moderate | • Lowers pH of wounds (bacteria thrives in alkaline environment) • Pseudomonas • Disinfectants |
| Saline | • Neutral | |
| Dyes-Scarlet red, Proflavine |
• Toxic | • Select out gram negatives |
| Na Hypochlorite-Dakin’s solution, Eusol | • Toxic = bleach | |
| Hydrogen Peroxide | • Action = Fizz | • Caution with deep wounds and open vessels |
| Quaternary Ammonia- Cetrimide |
• Very high toxicity |
Colour legend: Green – Low toxicity Yellow – Neutral Pink – High toxicity
Adapted from Wound Bed Preparation 2021

