Negative-Pressure Wound Therapy
Negative-Pressure Wound Therapy (NPWT)
NPWT is an adjunctive therapy that promotes wound healing. It is a sealed wound-care system that delivers a controlled suction across the surface of the wound bed. Figure 2 demonstrates NPWT primary mechanisms of action and their associated secondary effects (C. Huang et al. 2014; Orgill and Bayer 2013). Braakenburg et al. (2006) demonstrated that NPWT offers more comfort for patients and the treating team because of the fewer dressing changes and less leakage and odour. Because of faster healing, NPWT may not result in overall higher costs despite the expenses of the pumping device and specialized accessories. However, the available data on the efficacy of NPWT has significant heterogeneity in the type of wounds treated as well as clinical indicators assessed (Brassard and Tardif 2015). It is difficult to generalize results and favour NPWT over standard treatment for all wounds. Higher quality evidence assessing NPWT efficacy is required for an accurate cost-effectiveness analysis (Canadian Agency for Drugs and Technologies, 2014).
Figure 2: Negative pressure wound therapy: A sponge is placed into the wound and covered by an adhesive sheet, within which a suction tube is placed.
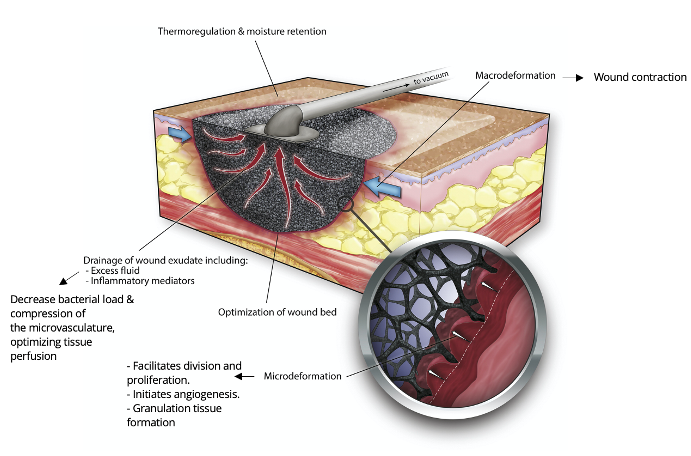
When Negative Pressure Wound Therapy (NPWT) is initiated and the wound has an occlusive seal, there are 4 primary mechanisms of action:
1. Macrodeformation (macrostrain)
2. Microdeformation (microstrain)
3. Fluid / exudate removal into the tubing.
4. Changes in the wound environment
When negative pressure is initiated and applied to the wound, there is a collapse of the sponge. The wound edges are pulled together (macrostrain). The small circular image shows the black foam with the open reticulated cells (pores). With the negative pressure “pull” between the black foam and wound bed cell layer, the top layer of the wound bed is drawn up into each of the black foam cells causing microstrain. This is what promotes the granulation tissue to proliferate at a faster than normal rate – due to the strain. This is unique action that only occurs with NPWT. Interstitial fluid is pulled into the tubing and canister. Edema is reduced. There are many changes in the wound environment. Growth factors and antibiotics can now get to this previously edematous area. The dressing is occlusive (air tight) and this promotes moist wound healing at an optimal rate.
Studies on neurotrophic diabetic foot ulcers (DFUs) with adequate blood supply to heal suggest that NPWT is associated with increased proportion of healed DFUs, reduced time to wound closure and decreased secondary amputations (Brassard and Tardif, 2015; Canadian Agency for Drugs and Technologies, 2014). In addition, NPWT has been found to increase split-thickness skin graft survival rate following surgical cover. The Canadian Agency for Drugs and Technologies in Health (2015) recommends the use of NWPT in acute and chronic wounds as an adjunctive therapy since it accelerates wound healing. For surgical wounds, NPWT may decrease the rate of surgical site infection in comparison to standard therapy (Webster et al. 2019).
Candidates for NPWT should be appropriately selected according to their clinical situation, wound-related factors, patient preferences, healthcare settings and available resources (Brassard and Tardif 2015) (Table 1). High-quality randomized controlled trials are needed to explore the co-use of NPWT with instilled materials (e.g., antiseptics, other antimicrobials) and parameters of application to determine optimal use of NPWT.
Table 1: NPWT indications, contraindications, precautions for use, and discontinuation criteria
| Indications | Contraindications | Precautions for use | Discontinuation Criteria | |
|---|---|---|---|---|
| Chronic Wound Closure (secondary intention |
|
|
|
|
| Acute Wound Closure |
|
|||
| Stabilize skin graft or flap | ||||

