Chapter 13: Burn Injury: Assessment and Management Principles
Author:
- Alan David Rogers (MBChB, MMed, FC Plast Surg, FRCSI, MSc, FACS)
Learning Objectives
- Evaluate accurate depth and extent of burns to determine appropriate treatment
- Recognize the role and criteria for referral to centralized burn units equipped with resources and multi-professional staff
- Review the sequelae of burn injuries (and its treatment) that may include long term functional and psychosocial effects
Introduction
Although most burns are minor and can be managed on an ambulatory basis, severe burns and those that meet specific criteria should be referred to regional burn units (Palmieri, 2015) (Table 1).
Table 1. American Burn Association criteria for referral to a burn unit (Palmieri, 2015).
| 1 | Partial-thickness burns >10% of the total body surface area |
| 2 | Deep burns |
| 3 | Burns involving the face, hands, feet, genitalia, perineum, or major joints |
| 4 | Circumferential extremity burns |
| 5 | Electrical burns and lightning injury |
| 6 | Chemical burns |
| 7 | Inhalational injury |
| 8 | Potentially complicating comorbidities |
| 9 | Significant associated trauma |
| 10 | Lack of qualified personnel or equipment for the care of children |
| 11 | Patients who require special social, emotional, rehabilitation, e.g., suspected child abuse |
These units are staffed by specialist nurses, therapists, social workers, surgeons, dietitian, amongst others. Within such settings, burn care is a systematized, goal-directed process.
Etiology and Pathogenesis
The severity of thermal injuries is influenced by patient age, the mechanism of injury, the duration of contact with the agent, the depth and extent of the burn, and the anatomical site involved. Most pediatric and geriatric burns are caused by scalds from boiling water or cooking oil. Flame burns are more common in adults, are often deeper and more extensive, and are responsible for most mortalities. Contact, electrical and chemical burns account for the balance, are frequently deep injuries to the palms of the hands, and may result in significant morbidity relative to the size of the burn.
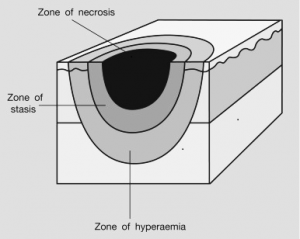
Thermal injury is a unique form of traumatic injury; direct tissue injury to the skin with associated inflammation and plasma loss may compromise multiple organ systems if extensive. Three concentric ‘Jackson zones’ of tissue injury characterize a full-thickness burn: coagulation, stasis, and hyperemia (Hettiaratchy S, 2004) (Figure 2).
The central zone of coagulation results from coagulative and ischemic necrosis from direct contact with the heat source and may appear white or charred. The intermediate zone of stasis is usually red, and while it may initially blanch with pressure, the area may evolve to be deeper, depending on the success or otherwise of local and systemic resuscitation efforts. The outer zone of hyperemia blanches with the application of pressure, indicating that it has intact circulation.
Major burn injury is characterized by a syndrome of sustained hypermetabolism, with an exaggerated systemic release of cytokines and other mediators of inflammation. Increased vascular permeability leads to extravasation and edema, which becomes greater with the administration of the fluid necessary to maintain organ perfusion. Hypovolemia accounts for decreased perfusion and oxygen delivery which is exaggerated by evaporative and conductive water loss from the deficient epidermis. (Jeschke M, 2020) (Figure 3)
Table 2. Functions of the skin
| 1 | Provides a protective barrier against mechanical, thermal and physical injury and hazardous substances. |
| 2 | Prevents loss of moisture. |
| 3 | Reduces harmful effects of UV radiation. |
| 4 | Acts as a sensory organ (touch, detects temperature). |
| 5 | Helps regulate temperature. |
| 6 | An immune organ to detect infections. |
Emergency Management
Initial assessment of a patient with a burn injury entails an Advanced Trauma Life Support (ATLS) style approach, including a primary survey to identify and treat immediately life-threatening conditions, followed by a secondary head-to-toe examination. For suspected inhalation injury, deep facial burns, and extensive burns, 100% oxygen is administered by face mask; early intubation and mechanical ventilation may be required. Patients with inhalational injury may experience upper airway swelling, acute respiratory failure (via several mechanisms), and carbon monoxide intoxication. For extensive burns, edema of the upper airway may increase rapidly during fluid resuscitation, especially in the context of facial burns, necessitating urgent preemptive intubation (Snell, 2013).
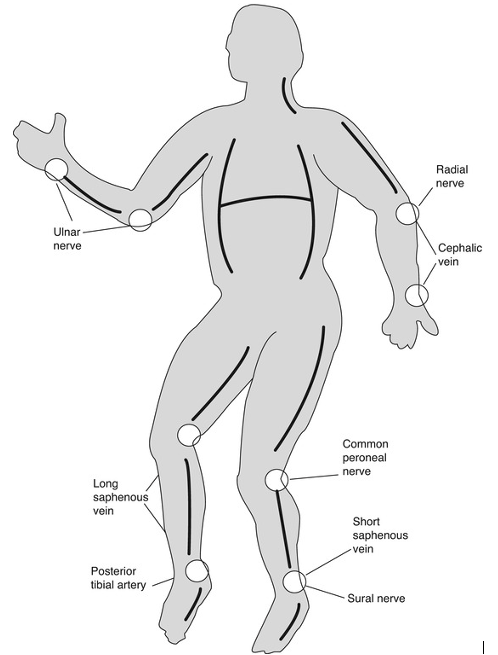
For major burns, intravenous access should be obtained and a urinary catheter inserted. All burns should be immersed in cool running water (not ice-water) for 20 minutes and then covered. Copious irrigation of the wound with water is indicated for chemical burns, and should continue until the surface of the wound has a neutral pH. Decompressive escharotomies are emergency procedures for constricting circumferential deep burns of the arms, legs, abdomen, and chest. The purpose of these procedures is to avoid ischemia distally or the restriction of chest excursion and breathing (Figure 4).
Figure 4. Locations for Escharotomy
Burn wound assessment
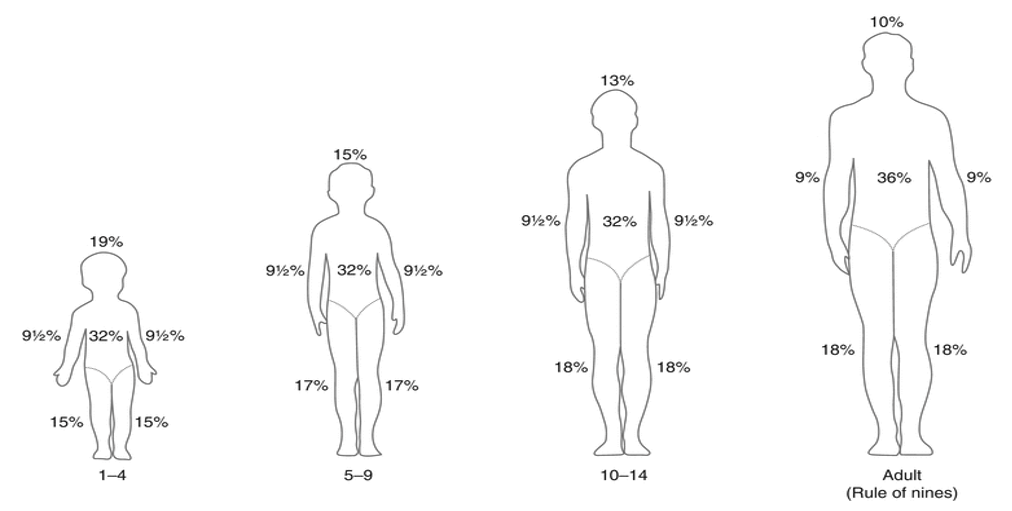
The size of the burn injury is expressed as a percentage of the total body surface area (TBSA).
A number of methods of assessment are used, often in conjunction with each other. Methods used include:
- The open adducted volar surface of the hand (including fingers) of the patient representing 1% of the TBSA
- Regions of the body are allocated percentages of the TBSA depending on the age of the patient (Figure 5). (Strobel, 2018).
Figure 5. The Rule of Nines
The depth of the burn dictates whether conservative wound care (dressings) or surgical management should be employed and correlates with long-term appearance and function (Figure 6).
Figure 6 Long-term appearance and function
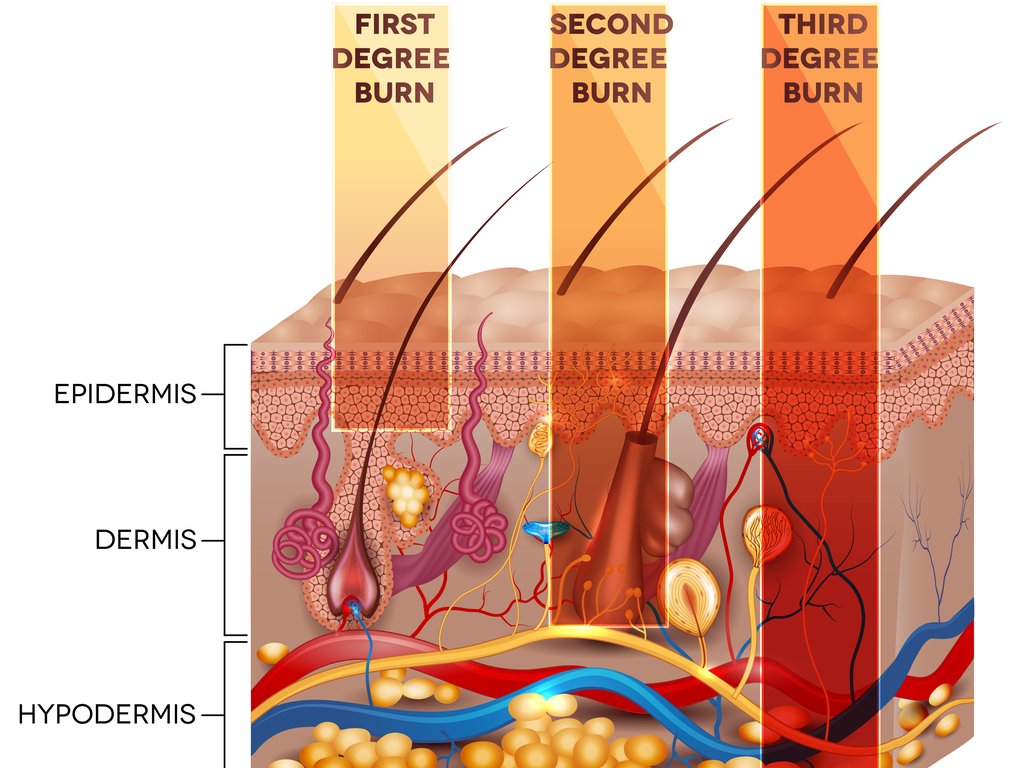 |
The layers of the skin showing the extent of the depth of the burn injury on the skin’s surface. Burns are classified depending on how deeply First degree burns only affect the other layer of the skin, the epidermis. These are not included in TBSA calculation. Second degree (deep partial thickness) burns involve the epidermis and part of the dermis. Third degree (full thickness) penetrate the epidermis and dermis and may extend to the subcutaneous tissue. Second and third degree burns are included in the TBSA calculation and usually warrant surgical management. |
Early excision and skin grafting for deep burns has been shown to be beneficial in reducing infection and scarring, shortening hospital stays, and improving ultimate function. Skin grafting creates a donor site that is itself a superficial partial thickness injury, and must heal by secondary intention.
Superficial (first degree) burns injure only the epidermis, are erythematous without blistering, and are not included in the TBSA burn estimation. Superficial partial-thickness burns (superficial second degree), on the other hand, are confined to the epidermis and the papillary layer of the dermis and usually heal within two to three weeks. Deep dermal/deep partial-thickness burns (deep second degree) involve the epidermis and dermis into the reticular layer and may require surgery. Full-thickness burns (third degree) have irreversible destruction of all elements of the skin. Many burns are a combination of injury depth, and accurate assessment may only be possible after a few days of observation, before a surgical course is chosen.
Fluid Resuscitation
Adequate fluid resuscitation is the most critically important aspects of early major burn care, and aims to maintain tissue and organ perfusion and minimize systemic sequelae, especially renal failure (Ho, 2020). Formal fluid resuscitation is required for burns exceeding 20% TBSA. This is usually admistered in the form of a crystalloid solution (usually lactated Ringers) at a volume of 3–4 ml per kilogram body mass per % TBSA during the first 24 h, titrated to maintain a urine output of 1ml per kg per hour in children, and 0.5ml per kg per hour in adults.
Patients who may require relatively more volume include those with full-thickness burns, inhalational injuries, electrical burns, and concomitant trauma, and for whom there was a delay in initiating resuscitation. A syndrome of overhydration has come to be known as “fluid creep” and may manifest as acute respiratory failure, pneumonia, multi-organ failure, the conversion of superficial into deeper burns, as well as abdominal, limb and orbital compartment syndromes (Saffle, 2007). Fluid resuscitation ‘failure’ may stem from an error in burn size estimation, fluid volume calculation, delay in initiating resuscitation, over-reliance on formula without titrating to effect, as well as neglecting the impact of sedating agents and analgesia on hemodynamics. Blind adherence to formula without regular evaluation and ongoing monitoring using urine output and clinical (blood pressure, pulse, sensorium) and biochemical tests (lactate, hematocrit) is perhaps the most significant concern.

