Chapter 1: Introduction and Statement 1
Wound Bed Preparation
Authors:
- Reneeka Jaimangal, MD, MScCH, IIWCC (CAN)
- Laurie Goodman, RN, MHScN, IIWCC (CAN)
- R. Gary Sibbald, BSc. Md. M.Ed., D.SC (Hon), FRCPC (Med)(Derm), FAAD, MAPWCA, JM
Learning Objectives
Type your learning objectives here.
- Review the importance of identifying/treating the cause and patient centered concerns
- Describe healable, nonhealable and maintenance wounds
- Evaluate local wound care and holistic care planning for the person with a wound
Wound healing is a dynamic and complex process that involves four phases: hemostasis, inflammation, proliferation and remodeling (Guo & DiPietro, 2010). All four phases need to follow a certain sequence and time interval to achieve optimal wound healing. Acute wound healing follows the normal healing trajectory and often closes in less than 30 days.
Chronic wounds are often present for more than 30 days, although some authors cite periods of up to 12 weeks before wounds are considered chronic. When the wound becomes “stuck” in one or more phases, most commonly the inflammatory stage, there is delayed healing that results in a chronic wound. Many factors including abnormal vascular supply, poorly controlled diabetes, malnutrition, infection and active autoimmune diseases may impair wound healing (Guo & DiPietro, 2010).
Chronic wound patients with prolonged wound healing that do not close with conservative wound care interventions become a major healthcare burden (Cukjati et al., 2001; Schultz et al., 2003). A 2018 systematic chronic wound review concluded that these wounds incur extensive health care costs (Olsson et al., 2019). Patients with chronic wounds also have reduced activities of daily living as reflected in poor quality of life assessments (Olsson et al., 2019). Therefore, it is imperative to accurately identify causes for impaired wound healing and correct them accordingly (Frykberg & Banks, 2015).
Wound Bed Preparation (WBP) provides a structured and systematic approach to wound management that facilitates wound healing and the use of other therapeutic interventions (Schultz et al., 2003). WBP was first published in 2000 (Falanga, 2000; Sibbald et al., 2000) with continuing updates over the years, the most recent being in 2021 (Sibbald et al., 2021). WBP focuses on identification of the cause, prevention and management of various wound types along with addressing patient-centered concerns for a holistic approach (Sibbald et al., 2021). See Figure 1.
Figure 1. Wound Bed Preparation Algorithm 2021
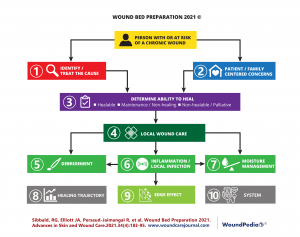
Wound Bed Preparation 2021 is a revision of previous iterations along with literature updates and was formalized by a consensus from wound care experts that produced 10 statement recommendations for chronic wound care (Sibbald et al., 2021). The following 10 statements presented in Chapter 1 have been adapted from WBP 2021.
Statement 1 – Treat the cause (s) of the wound
Early and accurate identification of the cause(s) and appropriate treatment are crucial to wound care and entails three steps: 1a, 1b & 1c
1a) Determine if there is adequate blood supply to heal: Adequate tissue oxygenation is vital for cell metabolism and many wound healing mechanisms, especially collagen synthesis, prevention of infection, re-epithelialization and angiogenesis (Gottrup, 2004). Clinicians should examine the leg and foot for signs of poor vascular supply (pallor on elevation, dependent rubor, cool distal extremity) and palpate for the pedal pulses (dorsalis pedis or posterior tibial). These are recorded as absent or present (Sibbald et al., 2011, 2021). About 8% of the general population have an aberrant dorsalis pedis artery and the posterior tibial artery should be alternatively palpated. A palpable pedal pulse (either of the two, not necessarily both) implies that the arterial pressure in the foot is at least 80mmHg or more.
The ankle brachial pressure index (ABPI) is a standard test used to determine the degree of arterial blood supply to the extremity and is calculated by dividing the ankle systolic pressure by the brachial (arm) systolic pressure (Al-Qaisi et al., 2009). A normal ABPI is equal to or greater than 0.9 and less than 1.4 (Beaumier et al., 2020; Gerhard-Herman et al., 2017). Less than 0.9 indicates some degree of arterial comprise, while an ABPI of more than 1.4 is an incorrect value that indicates calcification of the vessels in the foot (Beaumier et al., 2020; Gerhard-Herman et al., 2017). Calcification of the vessels is present in 80% of patients with diabetes and in approximately 20% of older adults (Sibbald et al., 2021). In these cases, toe pressure measurements are useful.
The audible handheld Doppler (AHHD) test is an alternative method, where based on the audible Doppler waveforms, the degree of arterial compromise can be determined. A monophasic sound indicates arterial compromise and the need for non-invasive sequential lower leg Duplex Doppler studies to identify bypassable or dilatable vessels. A multiphasic sound (triphasic or biphasic) indicates an audible ABPI equal to or greater than 0.9 with adequate arterial supply for healing and the use of high compression bandaging (Sibbald et al., 2011). A 2015 study on 379 legs on 200 patients concluded that the “AHHD proved to be a reliable, simple, rapid, and inexpensive bedside exclusion test of peripheral arterial disease in diabetic and nondiabetic patients” (Nabavizadeh et al., 2015). The AHHD test is quicker to perform than the traditional ABPI. It is not falsely elevated with calcified vessels, does not require the patient to be recumbent for 20 minutes and there is no need to inflate a blood pressure cuff just above the ankle on the lower leg (lower calf), which is often painful! (Sibbald & Ayello, 2021). See Table 1.
Table 1 Vascular Assessment Methods
| Method | Indication for Healability |
|---|---|
| Palpable pulse – dorsalis pedis, posterior tibial | >80 mmHg |
| Ankle-brachial pressure index (ABPI) | >0.5 and <1.4 |
| Transcutaneous oxygen tension | >30 mmHg |
| Toe pressure | >30-55 mmHg |
| Audible handheld Doppler | Triphasic or biphasic sound (represents ABPI >0.9) |
1b) Identify the cause(s) as precisely as possible or make appropriate referrals: Wound etiologies can often be unclear and misleading, resulting in inappropriate management strategies. The cause of the wound should be accurately identified, taking into consideration different wound types including vascular leg ulcers (venous is most common but also arterial, mixed, lymphatic or a combination), pressure injuries and foot ulcers often in persons with diabetes. See Table 2.
Other wounds include inflammatory ulcers (pyoderma gangrenosum, vasculitis) malignant ulcers, post-surgical, traumatic wounds and other factors that contribute to skin breakdown (moisture, fragile skin, additional comorbidities, etc.) (Sibbald et al., 2021).
Table 2: Treating the cause of three main wound types
| Wound Type | Treatment of the Cause |
|---|---|
| All wounds |
|
Venous ulcers
 |
|
Pressure injuries

|
|
Diabetic foot ulcers(V.I.P.S.)
 |
|
1c) Evaluate comorbidities and other factors that may delay/suppress healing: All modifiable cofactors and comorbidities should be focused on to expedite the wound healing process.
These factors include (Guo & DiPietro, 2010):
- systemic disease (especially uncontrolled diabetes, immunocompromised state, obesity, active autoimmune diseases)
- malnutrition
- previous wound related surgical interventions
- prescribed medication (immunosuppressants, oral corticosteroids over 20 mg daily)
- non-steroidal anti-inflammatory agents (some are over the counter), chemotherapy)
- substance use including smoking, alcoholism, street/illicit drug use
All medications and chronic diseases need to be optimized. This may require follow up with the family doctor and other specialists. Relevant laboratory investigations, especially complete blood count, hemoglobin, hemoglobin A1c (HbA1c), albumin, C-reactive protein, X-ray, ultrasound, etc., should be ordered where necessary.
The Canadian Nutritional Taskforce validated a 2 question screening tool to perform a quick nutritional assessment without requiring laboratory tests (Laporte et al., 2015; Screening – CMTF – Canadian Malnutrition Task Force, n.d.).
- Have you lost weight in the past 6 months without trying?
- Have you been eating less than usual for more than a week?
If the patient answers “yes” to both questions, a referral to a registered dietitian to perform a detailed nutritional assessment is required (Screening – CMTF – Canadian Malnutrition Task Force, n.d.).
Following a thorough assessment of patient that includes determining perfusion, cofactors and comorbidities that may inhibit healing, care plan goals focus on optimizing or treating the cause of the wound.

