Managing the Burn Wound
Superficial partial-thickness burns are usually healed within 3 weeks and are treated conservatively, which may include cleaning, debridement of blisters, topical antimicrobials, and/or occlusive or semi-occlusive dressings. Certain dressings may have an advantage over others in the management of partial-thickness burns and donor sites in terms of time to wound healing, number of dressing changes, ease of use, pain experienced, exudate management, and cost.
Silver sulfadiazine (flamazine) has been in use for several decades and remains an important dressing modality globally in the treatment of burns. It offers a cooling effect and is quick and easy to apply, smothered first in gauze. The Cochrane Review (2013) on dressings for superficial and partial thickness burns concluded “it is impossible to draw firm and confident conclusions regarding the effectiveness of specific dressings, however, silver sulfadiazine was consistently associated with poorer healing outcomes than biosynthetic, silicone coated and silver dressings whilst, hydrogel-treated had better healing outcomes than those treated with usual care.” [Wasiak et al 2013]
An alternative may be a tulle gras (petroleum gauze or variant thereof) covered by moistened gauze and wrapped. Dressing choice may be influenced by the adherence of the wound contact layer, preferred duration and interval, the wound’s moisture balance, and the presence of necrosis, slough, infection or eschar.
One should appreciate that all antiseptics are inherently cytotoxic. Selected agents can be diluted to offer a more biocompatible balance of antimicrobial efficacy and keratinocyte survival. Definitive temporary skin substitutes have been shown to effectively facilitate spontaneous healing in superficial partial thickness burns with a single application, and are able to reduce painful dressing changes considerably [Rogers, 2011].
Once surgically excised, deep burn wounds need to be covered with skin grafts harvested with a dermatome from unburned areas at that time or at a later surgery. These grafts can be meshed and then expanded to obtain greater wound coverage [Figure 7].
 |
A Weck:Goulian blade |
 |
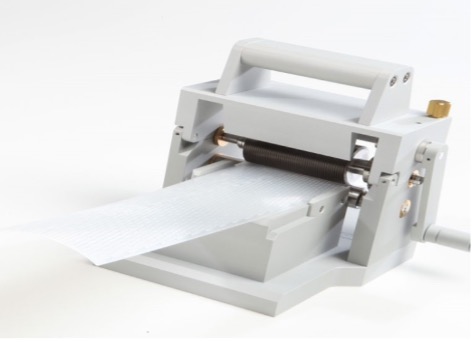 |
| Humby knife (a) and Weck/Goulian blade (b) for the tangential excision of deep burns for large and small/ special areas respectively. A dermatome (c) for harvesting split skin grafts, and skin graft mesher (d) to enable expansion. The ridges on the derma-carrier or on the mesher itself, depending on the design, determine the mesh ratio. | |
Wherever possible, the wound should be healed or operated within three weeks, in order to reduce scar hypertrophy, contracture, as well as infection. For extensive burns with limited donor sites, cadaver skin is the most effective strategy for temporary coverage [Table 2] [Allorto, 2016].
Table 2. Major indications for deceased donor allograft skin in burn centre
| Indication | Application |
|---|---|
| Extensive Burn | Staged application at time of excision and removal when autograft applied Over wide meshed autograft (3:1 or Meek) |
| Smaller burns | Burn involving special areas (hand / face) to improve sheet autograft take Management of burn wound infection |
| Necrotizing Soft Tissue Infection | ‘Test’ of wound bed/ optimize general condition prior to definitive closure |
| Exfoliative Skin Condition | Avoid repeated painful and traumatic dressings (alternative to Biobrane) |
| Complex Wound | ‘Test’ of wound bed / optimize general condition prior to definitive closure |
Pain control
Pain management is a prominent consideration throughout the course of treatment; the goal is to have a comfortable patient who is able to participate in rehabilitation and tolerate wound care and operative interventions [Shah, 2017; Pardesi, 2017]. Acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDS) should be administered by the clock unless there are contraindications. One should make use of adjunctive agents to reduce the reliance of opioid analgesics; we use both long and short acting hydromorphone and avoid analgesics containing more than one active agent. Gabapentin and pregabalin are effective in managing neuropathic pain, especially associated with donor sites and pruritic healing wounds [Nieuwendijk, 2018]. The N-methyl-D-aspartate (NMDA) receptor agonist ketamine has both analgesic and dissociative effects and may be used for conscious sedation during dressing changes but can also be provided orally. Alpha-2 agonists, like oral clonidine or a Dexmedetomidine infusion, may be used in addition to or as an alternative to benzodiazepines to manage anxiety. Non-pharmacological methods, including virtual reality, are an important consideration for awake patients [Schmitt, 2011].
Nutritional support
Patients should be regularly assessed by a dietitian to ensure that all caloric requirements are being met, and these may be corroborated by resting energy expenditure calculations [Rousseau, 2013]. For mechanically ventilated patients with extensive burns, continuous nutritional support is essential to obtain wound healing; volume-based feeding strategies compensate for any interruptions in enteral feeding over a 24-hour period, but feeds should generally not be withheld preoperatively and should be continued throughout surgical interventions [Sudenis, 2015]. Post pyloric feeding tubes may reduce the risk of aspiration and safely facilitates continuous feeds. Many of the pharmacological strategies investigated in the area of burn care aim to suppress the hypermetabolic response to major burn injury, and the consumption of resources to sustain it, redirecting them towards anabolism and wound healing [Brown, 2016].
Infection
Infection remains the main cause of morbidity and mortality after burn injury. These include ventilator associated pneumonia, wound infection, and bloodstream infections associated with indwelling vascular lines, urinary catheters and endotracheal tubes necessary for their critical care [Rogers, 2014]. Infection prevention and control protocols, patient isolation, timely surgery, optimal antimicrobial dressing use and reduced duration of invasive devices, all contribute to limiting infection rates. Antibiotics are initiated empirically for systemic infection according to known resistance patterns, as well as the timing and location of infections, and adjusted subsequently based on cultures. A wide variety of topical antimicrobial dressings are in use for the management of burns and burn wound infections, and decisions should usually be made based on the dressing interface and the desired duration between dressing changes, in addition to the active antimicrobial agent.
Rehabilitation and Reconstruction
Social workers play an integral role in coordinating important decisions and facilitating reintegration. Similarly, occupational and physical therapists help to prevent or decrease deconditioning, maintain function and joint range of motion, and reduce the negative sequelae of scarring. Splinting, pressure garment use, steroid injection and silicone gel sheeting are modalities that may reduce the need for burn reconstruction [Tredget, 2014] but laser therapy offers a number of beneficial effects [Zuccaro, 2018]. Burn reconstruction surgery is sometimes required to address extensive burn scarring and contracture through reorienting, resurfacing and lengthening procedures [Friedstadt, 2014; Cartotto, 2014] [Figure 9].
Figure 9: Surgical release of the right first web space burn contracture
 |
 |
| Surgical release of the right first web space burn contracture nine months after autografting of a right-hand flame burn injury. The left picture depicts the hand prior to surgery, while the right picture depicts the hand after surgery. (Photos courtesy of Alan David Rogers) | |
Author
Alan David Rogers (MBChB, MMed, FC Plast Surg, FRCSI, MSc, FACS)
Ross Tilley Burn Centre, Sunnybrook Health Sciences Centre, Toronto, Canada; Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Toronto, Canada. Email: alandavid.rogers@sunnybrook.ca


