Pain Assessment & Management
Pain Assessment
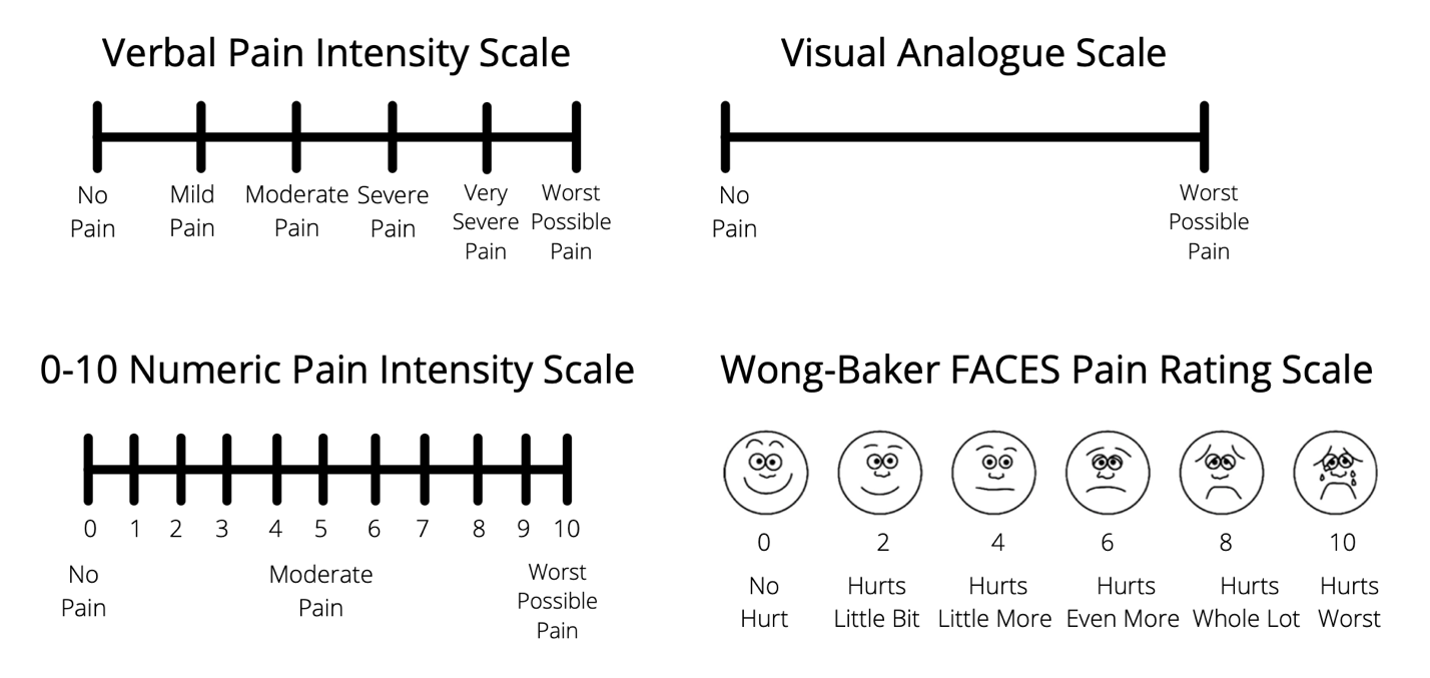
A thorough pain history is essential to wound pain management (Price et al, 2007). The nature, onset, duration, and exacerbating and relieving factors will help determine the cause of the pain and direct strategies for relief. Pain intensity can be reliably measured using validated pain scales. Several pain scales (Figure 2) have been widely accepted for use among older adults, including people with mild to moderate cognitive impairment (Herr and Garand, 2001). A verbally administered 0 to 10 numeric rating scale is a good first choice for measuring pain intensity. Anchors for pain may have more meaning by stating 0 is no pain, 5 is equivalent to a bee sting and 10 represents slamming the car door on your thumb! If the patient has difficulty with the scale, other verbal descriptor scales, pain thermometers, and faces pain scales (Hicks et al, 2001) also have accepted validity and reliability in this population (Bieri et al, 1990; AGS Panel, 2002). The scale of choice should be appropriate for the individual and used consistently with each assessment (Ferrell, 2002).
Figure 2 – Examples of Pain Assessment Tools
Although sensory and cognitive impairment may be present, pain can usually be assessed accurately using techniques adapted for the individual’s disabilities (Herr et al, 1995; Gagliese and Melzack, 1997). Older patients may be challenged with pain assessment tools (Ferrell et al, 1990; Grossberg et al, 2000). Many patients and their families accept pain as an inevitable consequence of aging, do not believe pain can be treated, may fear diagnostic tests, and/or assign too much importance to hypothetical medication side-effects or addiction (AGS Panel, 2002). A patient with severe dementia who suffers from pain presents a greater challenge. In this case (or in the case of a nonverbal patient) pain can be assessed by directly observing the patient for grimacing, other body withdrawal movements or obtaining a history from caregivers.
Patients should be observed for evidence of pain-related behaviors during movement or dressing changes. Deteriorating cognitive status or agitation also should elicit assessment for pain as a potential cause (AGS Panel, 2002).
Clinicians should have a high index of suspicion regarding sub-optimally treated pain when people with cognitive impairment have comorbid diseases that may include chronic wounds, arthritis, ischemia or cancer. Patients with persistent pain should be reassessed regularly for improvement, deterioration, or adherence to medication regimens. A good management strategy is using a pain diary. This could include logging pain intensity, medications used, mood and response to treatment (AGS Panel, 2002). Many barriers exist to optimal pain management (see Table 3).
Pain Management
The management of wound pain should be integrated into the Wound Bed Preparation paradigm (Sibbald et al, 2000; Reddy et al, 2003; Sibbald et al, 2021): treat the cause, address patient-centered concerns and optimize local wound factors . Treating the cause should determine the correct diagnosis and initiate treatment of the wound pain.
Patient-centered concerns must focus on what the patient perceives as the primary cause for the pain. To accomplish this, open discussions with the patient and family are needed, with the patient’s expectations being central. Care planning and education at regular intervals is also required, recognizing that this takes time. Patient anticipatory pain and suffering can be just as disruptive to activities of daily living as the actual experience of pain.
Local wound care needs to revolve around the four pillars of local wound care practice: DIME: Debridement, Infection / Inflammation, Moisture management, Edge effect. The Krasner model (Table 1) emphasizes the association of wound pain to identify the appropriate trigger and treatment (Krasner, 1995).
1. Treat the cause.
Treating the cause of chronic wound pain involves identifying and removing the source of the causative factor(s). For example, surfaces should be assessed to minimize excess pressure in the case of pressure injuries.
Wound infection and inflammation can cause wound pain. Treating the surface bacterial load and inflammatory stimulus can minimize the chance of deep and surrounding infection. Surface infection can be treated topically (ionized silver, iodine, PHMB / chlorhexidine, methylene blue / gentian violet). Deep and surrounding infections require systemic agents.
Pharmacological pain-reducing interventions are most effective when coupled with non-pharmacologic interventions that acknowledge patient-centered concerns (Jacox et al, 1994; Ferrell, 1996). By the gate control theory of Melzack and Wall (Katz and Rosenbloom, 2015), the nervous system only transmits one predominant signal. The non-pharmacological management strategies could include music, diaphragmatic breathing, meditation, yoga, TENS (Transcutaneous Electrical Nerve Stimulation), ultrasound, heat, cold, etc.
2. Patient-Centered Concerns in Wound Care
Pain in the context of wound care often has been described as the patient’s subjective experience. However, it is the caregiver who often interprets the patient’s pain according to his/her own cultural/environmental perspective.
Wound pain management can remain an inaccurate science if it is not tailored to the patient’s situation. Although “pain management experts” are available, patients in pain are frequently at the mercy of less well-informed members of the healthcare team whose approach can range from feast (the more pain medication the better) to famine (limiting pain medication because of fears of addictive or drug-seeking behaviors). In addition, the pain experience of the elderly is often neglected and poorly controlled. The more experienced healthcare professional carefully integrates pain management into the wound management process.
Consider each of the following steps (Sibbald et al, 2021):
A) Identify barriers to effective pain management
B) Activate a patient-centered approach to wound care
C) Address anxiety, depression and pain
D) Consider non-pharmacological management of pain
E) Debride wounds appropriately
F) Manage infection/inflammation
G) Initiate appropriate topical treatment
H) Optimize moisture management
Wound Pain Fundamentals
Assume that every wound is painful and that every patient who has a wound is in pain (Briggs et al, 2004). Patients frequently experience pain during dressing changes (e.g., strong adhesives, debridement), especially around wound edges and in infected or inflamed wounds (Collier and Hollingworth, 2000; World Union, 2004; Tegegne et al, 2020).
Wound pain can serve as an important indicator of inadequate wound management, untreated underlying cause and/or infection (Sibbald et al, 2003).
Debridement and wound cleansing are often main sources of pain or discomfort (Rodeheaver, 2001). Both procedures are necessary to facilitate wound healing (O’Brien, 2002).
Moist wound healing results in faster healing, (Winter, 1963; Hinman and Maibach, 1963) less scarring and less pain. The pain reduction is attributed to the nerve endings being covered in fluid that prevents dehydration (Kannon and Garrett, 1995).
Table 3: Dressing and Treatment Approaches
Clinical Nuggets: Sometimes Forgotten Pain-Relieving Strategies
- Clinician & patient (+ family) should have a planning discussion for dressing changes, debridement or procedures with patient consent and input prior to starting. This helps the patient to positively anticipate the steps involved shifting some sense of control to them. Debriefing patients by reflecting on the procedure is beneficial to improve the next planned intervention
- Ask the patient what has previously worked or not worked to include the feedback into the planning of the next procedure
- Be organized and have all anticipated equipment ready prior to starting a dressing change or procedure. Minimizing the time the wound is exposed to air reduces irritation, cooling of the wound bed and pain
- Handle all wounds gently (Moffatt et al, 2002)
- Avoid unnecessary stimulus to the wound, including unnecessary prodding or poking
- Avoid drafts from an open window, fan or vent
- Protect wound edges with barrier products (film forming liquid acrylates, petrolatum, zinc oxide, windowed dressings)
- Allow patients to change their own dressing if possible (Reddy et al, 2003)
- Allow patients to call “time out” verbally or by some nonverbal cue like raising their hand (Krasner et al, 2006).
- Encourage slow, rhythmic breathing and other relaxation techniques.
- Let patients know that there are “no points for bravery” and that blood flow may be decreased during episodes of pain.
- Topical anesthesia prior to debridement / medical procedures: Apply approximately 20 to 30 (or up to 60 – depending on the region) minutes prior to the procedure, under occlusive plastic wrap (Evans and Gray, 2005)
- A systematic review of topical analgesic & anesthetic agents determined that lidocaine / prilocaine cream (EMLA – Eutectic Mixture of Local Anesthetics) and ibuprofen foam are effective agents for reducing wound-related pain associated with chronic leg ulcers (Purcell et al. 2020). These products need to make direct contact with the wound surface and surrounding skin to be effective
- Use dressings least likely to adhere and to cause pain including hydrogels, hydrofibers, alginates, soft silicones (Alvarez et al, 2006) and cellulose (Hollingsworth, 2000). Gauze can reduce moisture but may cause tremendous pain, especially when adherent to the wound surface and is subsequently removed (Puntillo et al, 2001)
- Avoid the pain associated with gauze for healable wounds (Moffatt et al, 2002). Novel alternatives to gauze include calcium alginates, hydrogels, hydrocolloids & polyacrylate dressings. These promote efficient moisture management and debridement without pain (Percival et al, 2005)
- Fill but avoid overpacking wound cavities (“Fluff, don’t stuff”)
- Match absorbency with exudate levels (Moffatt et al, 2002)
- Choose advanced wound care dressings for longer wear times.
Dressing removal is often associated with increased pain (Moffatt et al, 2002). Dry dressing and adherent products are most likely to cause pain and trauma at dressing changes. Products designed to be non-traumatic should be used to prevent pain. Gauze is most likely to cause pain and should be avoided, including wet-to-dry regimens (Ovington, 2001).
One of the most important dressing selection considerations involves choosing a dressing that minimizes pain (Briggs et al, 2004; Woo et al, 2009).
Be sure to select dressings with absorbency that matches exudate levels (Queen et al, 2004; Briggs et al, 2004). Choose dressings with longer wear times to minimize wound manipulation and aggravation of the wound healing cycle. Contact layers or dressings that remain in close proximity to the wound bed prior to dressing changes also have proven beneficial for pain reduction (Reddy et al, 2003). Do not neglect pain management during wound cleansing. Appropriate noncytotoxic wound cleansing (potable water, normal saline) used at body temperature are best to reduce discomfort (Van Rijswijk and Braden, 1999).
When removing a dressing, avoid unnecessarily manipulating the wound, thus preventing further damage to the delicate granulation and healing tissue within the wound bed and periwound skin. If the dressing has become dried out, moisten it with an isotonic solution before removal (Queen et al, 2003). Choose dressings that allow less frequent and therefore less painful dressing changes (Sibbald et al, 2021). An exception to the moisture balance rules are persons with maintenance or nonhealable wounds (bacterial and moisture reduction is more important than tissue toxicity). These individuals should have bacterial and moisture reduction using topical antiseptics and superabsorbent dressings. This avoids the use of more expensive dressings, including foams with moisture exchange. If the dressing becomes dried onto the wound surface, the wound dressing can be hydrated with saline or water for easy removal.
Too often clinicians ignore pain because it is not easy to measure, yet unrelieved pain may seriously hamper efforts to heal chronic wounds. A paradigm that integrates pain management into an approach to wound bed management provides the clinician with a framework for improved care. An approach to chronic wound pain management that treats the cause and addresses local wound factors may lead to improved outcomes as patients may be more adherent to optimal care plans. Patient-centered wound care management strategies requires further interprofessional education and training to create an environment where pain and trauma are minimized. A patient-centered regimen ensures appropriate care in a reduced pain environment (see Table 4).
Table 4 – MANAGEMENT OF WOUND-RELATED PAIN (Sibbald et al, 2021)
| Simplified Pain Component | Therapeutic Action |
|---|---|
| Use a measurement tool |
|
| Differentiate neuropathic pain |
|
| Differentiate nociceptive pain |
|
| Dressing removal |
|
| Wound cleansing (sterile only required with immune compromise, deep postsurgical wounds) |
|
| Debridement
Healable wounds – sharp surgical, autolytic, enzymatic, mechanical, biological Maintenance or nonhealable wounds – conservative surgical |
|
| Document and re-evaluate at regular intervals |
|
| ©WoundPedia 2021. | |

