Chapter 11: Skin Tears
- Author:
Kimberly LeBlanc PhD, RN, NSWOC, WOCC(C), FCAN
Samantha Wiesenfeld (Student Nurse)
Learning Objectives
- To review Skin Tear risk factors
- To identify appropriate Skin Tear intervention and treatment strategies for at-risk patients
- To define the ISTAP Skin Tear classification system including Types 1, 2 and 3
The International Skin Tear Advisory Panel (ISTAP) defines Skin Tears (STs) as “a traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer)” (LeBlanc et al., 2018).
Skin Tears are considered the most prevalent wound etiology found in the Long-term Care (LTC) setting (Carville et al., 2014). The prevalence of STs in the LTC population are reported between 3.9% and 26.0% (Chang et al., 2016; Koyano et al., 2016; LeBlanc, Christensen, et al., 2013; Skiveren et al., 2017; Woo et al., 2017). The ST incidence within the LTC population has been reported to be between 2.2% and 16.0% (Payne & Martin, 1990; Sanada et al., 2015). If improperly identified and managed, they can become chronic and complex wounds, leading to individual pain, suffering, and increased costs to the healthcare system (LeBlanc & Baranoski, 2011).
Skin Tear Risk Factors
Figure 1: Skin Tear Risk Framework © LeBlanc 2017 (used with permission)
| General Health -Chronic/Critical Diseases – Aggressive Behaviour – Mobility – Dependence for Activities of DailyLiving (including functional mobility) – History of fallsSkin – History of previous skin tears – Skin changes Associated with Aging (skin Atrophy, Ecchymosis, Senile Purpura, Hematoma, Stellate Pseudo Scar) – Photo-damage |
> | Mechanical Skin Trauma – Shear, Friction and/or Blunt Force TraumaIndividual / Care-giver / Healthcare Professional – Knowledge of Skin Tear Prevention Strategies – Attitude – Practice or Approach of providing CarePhysical EnvironmentHealthcare Setting – Skin Tear Audit Programs – Support for skin tear Reduction Programs – Interprofessional Approach to Care |
> |
Skin Tear |
STs are frequently seen in the extremes of age, the critically and chronically ill, and those who require assistance with activities of daily living (ADLs) (LeBlanc & Baranoski, 2011; LeBlanc et al., 2018; Rayner et al., 2015). Furthermore, a history of falls, decreased levels of mobility, agitated behaviour and non-responsiveness are reported to be additional risk factors for ST development (LeBlanc et al., 2020; Strazzieri-Pulido et al., 2015).
In addition to the above-mentioned risk factors, it has been reported that the greatest predictor of ST development is having a history of previous skin tears (LeBlanc et al., 2020, 2021). LeBlanc, Woo, VanDenKerkhof and Woodbury (2021) concluded that other skin related issues such as skin changes associated with aging (skin atrophy, ecchymosis, senile purpura, and stellate pseudo scar), hematomas, and photo-damage present as risk factors for ST development (LeBlanc et al., 2020, 2021).
LeBlanc, Woo, VanDenKerkhof and Woodbury (2021) (Figure 1), maintain that the above-mentioned risk factors will not independently result in ST development. STs will develop from meditating factors that include exposure to:
- medical adhesives or other forms of mechanical skin trauma
- dismissive healthcare professional or caregiver attitudes towards ST prevention
- a physical environment which heightens the risk for STs
- lack of healthcare setting commitment to the prevention of skin tears.
Skin Tear Prevention
ISTAP maintains that the best method for managing STs is to develop a targeted prevention program (LeBlanc & Baranoski, 2011; LeBlanc et al., 2018) (Table 1). A 2014 study performed by Carville et al. (2014), reported that simply applying moisturizer / emollient once or twice a day can reduce skin tear incidence by up to 50% (Carville et al., 2014). Skin changes that occur due to aging can contribute to disruptions in the normal functioning skin barrier; ultimately resulting in the skin being more susceptible to ST development (Carville et al., 2014). Moisturizers can provide added protection against ST development by aiding in skin hydration.
Table 1. Risk reduction program checklist (adapted from Leblanc and Baranoski, 2011)
| RISK FACTOR | ACTION |
|---|---|
| Skin |
|
| Mobility |
|
| General health |
|
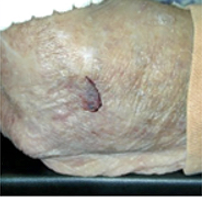
Classifying Skin Tears
The International Skin Tear Advisory Panel developed and validated the ISTAP Skin Tear Classification system (Figure 2) to establish common terminology and a standardized method for describing and documenting STs. This classification system should be used for the assessment and documentation of STs (LeBlanc, Baranoski, Holloway, Langemo., 2013).
IASTAP Skin tear Classification
| Type 1 | Type 2 | Type 3 | |
| NO SKIN LOSS | PARTIAL FLAP LOSS | TOTAL FLAP LOSS | |
 |
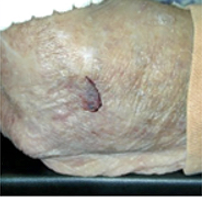 |
 |
 |
| Linear or Flap Tear which can be repositioned to cover the wound bed. | Partial Flap loss which cannot be repositioned to cover the wound bed. | Total Flap loss exposing entire wound deb. | |
Figure 2: ISTAP ST Classification System ©ISTAP 2013 used with permission
“A flap in skin tears is defined as a portion of the skin (epidermis/dermis) that is unintentionally separated (partially or fully) from its original place due to shear, friction, and/or blunt force. This concept is not to be confused with tissue that is intentionally detached from its place of origin for therapeutic use e.g. surgical skin grafting” (Van Tiggelen et al., 2020).
Skin Tear Assessment
Initial management of STs should include controlling bleeding, re-approximation of wound edges and classification according to the ISTAP ST classification system (Figure 3).
| SKIN TEARS | |||
| ↓ | |||
| Control Bleeding ASSESS | |||
| ↓ | |||
| CLEANSE | |||
| ↓ | |||
|
APPROXIMATE WOUND EDGES CLASSIFY (Measure and Document ) |
|||
| ↓ | |||
| GOALS OF TREATMENT | |||
|
|
|
|
| ↓ | |||
| TREATMENT OPTIONS IN ACCORDANCE WITH LOCAL WOUND CONDITIONS | |||
| TYPE 1: NO SKIN LOSS | Type 2: PARTIAL FLAP LOS | Type 3: TOTAL FLAP LOSS | |
 |
 |
 |
 |
Skin Tear Management
Skin tears are acute wounds which should have a wound healing trajectory of 14 to 21 days. Type 1 STs have the potential to be closed by primary intention, while type 2 and 3 STs will close by secondary intention. It is imperative that they are properly managed to prevent progression towards chronic and complex wounds (Figure 3) (LeBlanc, Baranoski, et al., 2013). Once the ST has been classified, the next steps include addressing patient concerns, treating the cause, initiating a ST prevention program, avoiding recurrent trauma, protecting the peri-wound skin, promoting moist wound healing, managing exudate, avoiding infection, and controlling pain (LeBlanc et al., 2018). ISTAP also recommends assessing for and controlling co-morbidities. This includes completing a lower leg assessment, if the ST is on the lower leg, and initiating compression therapy when indicated (LeBlanc et al., 2018). ISTAP further recommends that sutures, staples and skin closure strips should be avoided given the fragility of the ST peri-wound skin (LeBlanc et al., 2018).
Dressing selection should include products that will not add an increased risk for trauma, provide moist wound healing and manage pain (LeBlanc et al., 2018). LeBlanc and Woo (2021) conducted a pragmatic randomised controlled clinical study to evaluate the use of silicone dressings for the treatment of STs. They concluded that silicone dressings (silicone contact layers or silicone foam dressings) are a superior option for the treatment of STs. In their study, it was reported that STs healed almost two times faster with silicone dressings compared with conventional nonadherent dressings over the course of three weeks. Furthermore, the proportion of healed subjects was almost three times higher in the silicone treatment group.

