Introduction
Margo McCaffery summarized her view of pain as “It’s whatever the experiencing person says it is, existing whenever and wherever the person says it does” (McCaffery, 1968). Pain is often neglected because no simple diagnostic test exists to measure it.
Wound-related pain is an important component of patient-centered concerns that is often undervalued by healthcare professionals. When patients are asked to identify their priorities for a healthcare visit, they often reported pain management as their number one priority. In the late 90s, the European Wound Management Association (EWMA) drove a change in the management of wound related pain with its pivotal position document (Moffatt et al, 2002). This document recognized and focused on chronic wound pain and its influence on patients’ quality of life. It stated that one of the failures of modern medicine is the inadequate assessment and treatment of pain.
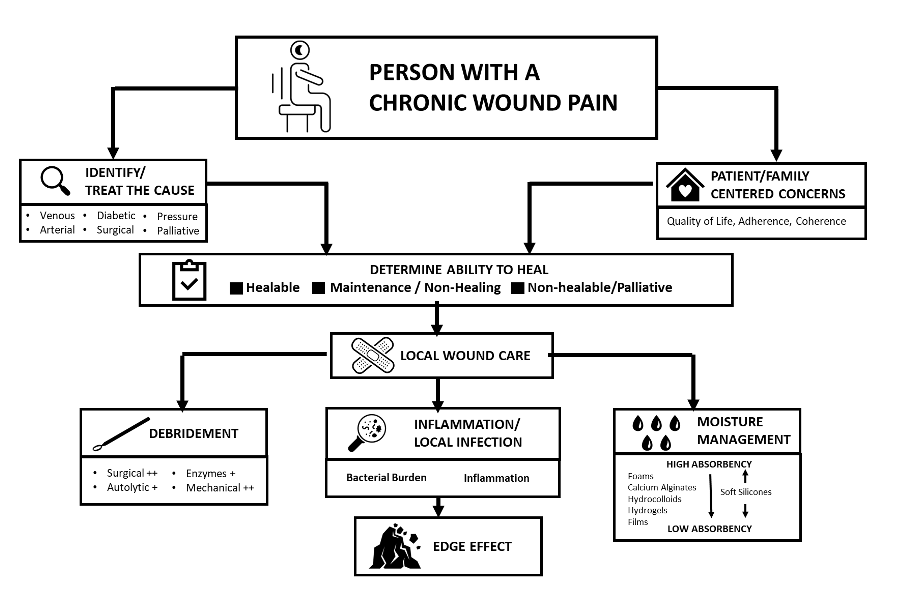
In the several decades since the publication of this document, the management of wound pain has been integrated into the wound bed paradigm originally discussed in Sibbald et al (2000, 2003, 2006, 2011, 2015 and 2021). The three main pain components are (Figure 1)
- Treating the cause involves the correct diagnosis of the wound pain.
- Patient-centered concerns must focus on what the patient sees as the primary reasons and resolutions for the pain.
- Local wound care needs to revolve around the three pillars of practice: debridement, bacterial balance, and moisture management, including the impact of pain.
Figure 1 – Chronic Wound Pain Paradigm (Adapted from, Reddy et al, 2003 and Sibbald et al, 2021)
The Mechanism of Pain
The process of pain involves a stimulus, detection of the stimulus by receptors, transmission of the stimulus via nerves, and interpretation of the stimulus in the brain. Pain can be described through two main types, nociceptive and neuropathic.
Nociceptive pain is an inflammatory response to direct tissue damage with an identified trigger or stimulus. Usually, relatively acute, nociceptive pain resolves when the tissue damage stops and resulting inflammation subsides (Wulf and Baron, 2002).
Neuropathic pain is independent of acute stimuli or triggers. Often, it is described as spontaneous with burning, tingling or stinging and when more severe, as stabbing or shooting.
Trauma to the peripheral nerves (e.g., amputation and phantom limb pain) is often associated with abnormal sensory function and a relative increase in patients’ response to pain (Colloca et al, 2017).
The term ‘chronic pain’ has been overused and has an unfortunate inference as a negative term often associated with drug misuse. The term ‘persistent pain’ may encourage a more positive attitude by patients and health professionals (AGS Panel, 2002).
Some Negative Outcomes of Unrelieved Pain
- Uncontrolled pain can cause stress and activation of the sympathetic nervous system. This can result in endocrine system releasing excessive hormones, inflammatory process activation, tachycardia, increased respiration rate and eventually weight loss (Wells, Pasero, McCaffery, 2008). Involuntary movements prepare the body for fight or flight.
- Sub-optimally managed pain is harmful for patients with metastatic cancers by reducing natural cells needed to prevent further tumor growth and spread (Wells, Pasero, McCaffery, 2008.
- Unrelieved acute pain may increase likelihood of chronic pain in future. One example is when acute pain from shingles is not managed aggressively and early, there is increased risk for ongoing post herpetic neuralgia (a painful chronic condition following shingles).
- Sub-optimally managed pain can lead to mistrust between the patient and care provider resulting in decreased patient satisfaction and delayed recoveries. This can lead to depression, anxiety and unscheduled emergency visits, all translating to largely preventable costs to the healthcare system.
There are many barriers to effective pain management from both the clinician and patient’s side. Fear of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) or negative attitudes and misconceptions toward opioid use may adversely overshadow both patient and clinician perspectives. The lack of pain assessment education and treatment is also a common factor for appropriate clinical use of both product classes. From the patient’s perspective, there may be a history of opioid tolerance or overuse that can negatively impact optimal pain management. These are a few of the complex challenges. There is a need to overcome pain related barriers and myths.
Wound Associated Pain
Tissue injury associated pain signals have an essential function and are clinically important symptoms (Khammissa et al, 2020; Bechert and Abraham, 2009). For example, local pain as a symptom or any increase in pain without another etiology is a key predictor of wound infection. It is one of the four cardinal indicators for inflammation (Gardner et al, 2001; Cutting et al, 2013). Pain or the fear of pain can also influence the healing process by interfering with the immune response (Matsuzaki and Upton, 2013). Unresolved pain is often associated with delayed wound closure (Stechmiller et al, 2019). Krasner proposed a conceptual model for wound pain (Table 1).
|
Table 1 – Krasner Model for Chronic Wound Pain (Modified from Krasner, 1995; Krasner, 2001) |
|
The clinical acceptance of wound-related pain is the first component but of equal importance is an understanding of the mechanism of pain, its impact clinically (Table 2) and its management from a patient’s perspective (Bechert and Abraham, 2009).
|
Table 2 – Important Facts Regarding Management of Wound Related Pain (Modified from Purcell et al, 2020). |
|
Professionals often define and assess a patient’s wound pain based on their clinical assumptions (Woo et al, 2008; Woo and Sibbald, 2009).

