Evolution of Dimensional Measurements versus Healing Trajectories
Clinicians and researchers have been measuring wounds in different ways for years, if not decades. More recently, technology has played a significant part in the evolution of the way in which we not only describe wounds but measure and document them (Wang et al, 2017; Queen, 2019). This technological evolution has taken the science of measurement beyond simple, single point dimensional measurements to the more dynamic measurement of wound healing trajectory (Feldman 2018). This is a better measure of success of any clinical approach including the assessment of therapies and treatment approaches (Bharara et al, 2010; McQuilling et al, 2021).
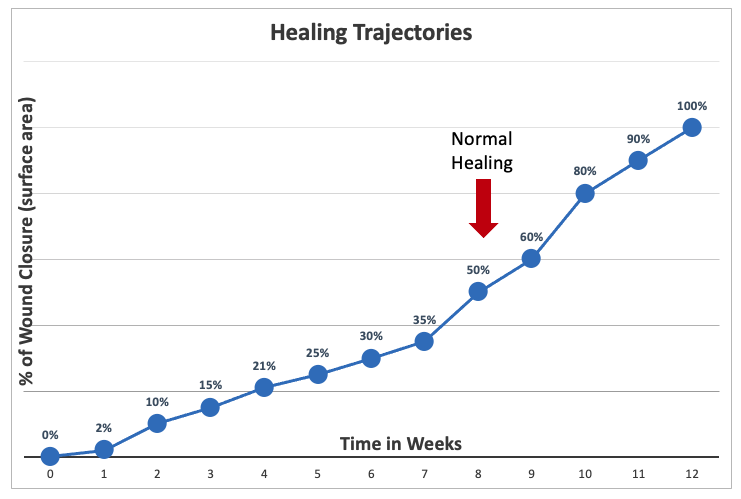
Tracking the healing process of open wounds follows an exponential curve. Wound-healing trajectories (percentage of wound closure versus time) have been used to describe chronic wound healing (Payne, et al 2011). Although wound healing trajectories were initially intended for acute wounds, they can also be used to evaluate the healing of chronic and complex wounds, including diabetic foot ulcers, pressure injuries and venous leg ulcers (European Wound Management Association, 2008; Phillips et al, 2000; Sheehan et al, 2003; Cardinal et al, 2009; Prince and Dodds, 2006).
Figure 1 – Healing Trajectories (Norris and Chapman-Jones, 2015)
One potential inconsistency is actually measuring the wound size. Even when using digital photography, non-invasive measurements of wound area are subject to errors especially when defining the wound edge. This is most common when different operators are responsible for obtaining and analyzing the images (Wang et al, 2017). This is even more apparent when clinicians use a paper ruler. Furthermore, such methods only measure the area of the wound and provide no information about changes occurring in the wound depth (volume vs area).

