Treating the Cause
Treating the Cause
Assessment
The assessment of venous leg ulcers requires a comprehensive history and physical examination to elucidate symptoms and signs for both venous and arterial disease. It is recognized that arterial disease co-exists in about 25% of cases (O’Donnell, 2014). Evaluation of the arterial system is important to assess the healing potential as well as the type and strength of safe compression application. The pathophysiology of venous leg ulcers is associated with sustained venous hypertension due to chronic venous insufficiency (CVI). Return of fluids from the lower extremity occurs by movement from the superficial veins through the perforators to the deep venous system and back to the right side of the heart.
This chapter concentrates on the venous system, however there is additional evidence for the contribution of the lymphatic system to manage fluid in the lower extremity (Woodcock, 2012). Damage to the lymphatic system can contribute to venous disease and vise versa. Congestion in the venous system can result from 3 main mechanisms:
- 1) Failure of the calf muscle pump: Meulendijks et al. (2018) have identified the calf muscle dysfunction as a strong predictor of VLU severity and impaired healing. Any process that prevents heel-toe walking pattern will be a risk for venous congestion. Some examples include joint issues in the extremity, shuffling gait or disease processes including muscular or neurological diseases (e.g., Parkinson’s disease).
- 2) Valvular disease: Valves in the veins can become inefficient because of continuous downward pressure on the system or genetic weakness. Examples include obesity (higher body mass index), multiple pregnancies or even employment that requires long hours of sitting or standing.
- 3) Obstruction: The major cause of venous obstruction is a history of a deep vein thrombosis causing damage to the deep venous system. With deep vein thrombosis and surface compression, there may be an intolerable increase in pain because the surface veins are compressed and cannot support adequate venous return to the heart.
Risk factors for arterial disease should be evaluated in the history and physical examination as listed in Table 1. These are similar to coronary artery disease, with smoking, diabetes and advanced age being the most common.
Table 1 Components of a History and Physical Examination
| History | Risk factors for venous disease- may include genetic factors, obesity, standing occupations, smoking Co-morbid conditions: (diabetes mellitus, connective tissue diseases, inflammatory conditions), arterial risk factors History of previous or with current venous ulcer(s)- use Clinical-Etiology-Anatomy-Pathophysiology (CEAP) classification Symptoms of venous congestion (edema below the knee) |
|---|---|
| Bedside examination | Blood pressure (BP) Lower leg examination and ulcer characteristics Palpate for pulses at the femoral, popliteal, dorsal pedis and posterior tibialis Ankle Brachial Pressure Index (ABPI) or Audible Handheld Doppler (AHHD) Gait assessment including walking aids, footwear, physical activity and ankle joint range of motion |
| Laboratory | Blood glucose level, HbA1c If indicated: complete blood count, kidney (creatinine), liver function, additional co-morbid issues Thrombophilia screen if deep vein thrombosis (DVT) history unexplained, young age, family history -Factor V/ Prothrombin Gene mutations, Antiphospholipid Antibody, Deficiencies – Anti prothrombin, Protein C/S (Merriman, Greaves, 2006) |
| Vascular laboratory | ABPI and more extensive arterial studies if indicated Venous Duplex Doppler (often indicated when ABPI is below 0.70) |
| Allergies/Sensitivities | Oral Medications – especially those that can impair healing Topical agents – avoid common sensitizers |
| Self-care abilities / Psychosocial issues | Activities of daily living – meals, shopping, financial stability Continence status – incontinence issues Patient concerns – support system: circle of care, pain |
| Nutrition | Weight- BMI:
<18.5 Underweight Validated Canadian Nutrition Screening Tool (Yes x 2 – Registered Dietitian consult for further assessment) |
| Medications | Immuno-suppressants/ oral steroids over 20 mg Assess drug interactions: if adding drugs (antibiotics/ other drugs-agents) Venous disease: lower leg edema, at rest, with ambulation (R/O claudication with arterial disease) |
| Pain | Procedure-related to wound (e.g., dressing change, debridement, infection) Related to lower leg edema, compression bandages or local wound dressings |
Table 1 Modified from & reproduced with permission: Best Practice Recommendations for the Treatment & Management of Venous Leg Ulcers. 2019. Wound Care Canada (Evans et al., 2019)
Symptoms related to venous congestion may include swelling, aching, throbbing, and cramping of the legs, particularly at the end of the day. Venous stasis causes a disruption of the epithelial barrier, commonly seen as contact irritant dermatitis that comprises about 80% of contact dermatitis. Allergic contact dermatitis with itchiness is also common. It is important to illicit all topical agents that are being applied to the leg as many contain sensitizers and allergens (Sibbald et al., 2007). The difference between contact dermatitis and cellulitis is reviewed in Table 2.
Table 2. Dermatitis versus Cellulitis in the lower leg: Reproduced with permission: Wound Care Canada
| Presentation |
Stasis Dermatitis with erosions
|
Cellulitis with Ulcer
|
| Symptoms / General Signs | Afebrile Itching, discomfort most common Varicose veins/ Potential deep vein thrombosis May be unilateral or bilateral |
May have fever Painful Relevant history of venous disease, ulcer Most often unilateral |
| Specific Signs | Normal temperature Erythema, inflammation Itch but may be tender Vesicles and crusting Lesions on other body parts (e.g., other leg, arms, trunk) If blisters, or pain along with deep inflammation consider secondary infection |
NERDS and STONEES tool (Woo, Sibbald, 2009) – Any 3 of the following 7 criteria for infected ulcers: *Size of ulcer has increased *Temperature: Elevated (3°F or greater than mirror image) *Os- Latin for Bone probing or exposed bone *New areas of breakdown *Erythema, Edema (Cellulitis) *Exudate increased *Smell – often gm-ve/ Anaerobes |
| Portals of Entry | Stasis dermatitis with loss of the epidermal barrier (erosion, ulcer) allows allergens to penetrate | Usually unknown; break in skin, ulcers, trauma, tinea pedis (foot fungus), intertrigo implicated (between toes). |
| Laboratory | Often nothing is seen | May have elevated WBC count especially neutrophils Skin swabs – Staphylococcus aureus or Streptococcus most often identified |
Table 2. Dermatitis versus Cellulitis in the lower leg: Reproduced with permission: Wound Care Canada
Pain related to venous ulceration is common and is reported in over 60% of patients (Hofman et al., 1997). Claudication and rest pain are symptoms of arterial insufficiency. Claudication is a reproducible pain that occurs in the lower extremity after walking a defined distance and is relieved by rest. Rest pain is most common at night or when in a recumbent position with the leg elevated that is relieved by hanging the leg in a gravity-aided dependent position or by walking. This level of pain would require an urgent vascular surgery consult. Characteristics and location of ulcerations may also give clues to the presence of arterial compromise. Distal punched out ulcers are more characteristic of arterial compromise (Evans et al., 2019).
Physical Findings
Characteristic changes associated with venous insufficiency are illustrated in Table 3. Changes characteristic of arterial disease could include cool extremity, muscle atrophy, dependent rubour and distally located ulcers with a punched-out appearance. Decreased hair growth and nail changes (thickening, loss of lustre) may be less reliable. The physical finding of edema in the lower extremity could also be related to more systemic disease including congestive heart failure, liver, renal and gastrointestinal issues causing fluid overload, especially if the edema is bilateral and extends above the knee. This of course can co-exist with localized lower leg venous disease complicating the management of our patents. With edema it is also important to consider and rule out an acute deep vein thrombosis or a ruptured Baker’s cyst.
Table 3. Physical changes and presentation of symptoms related to venous disease
| Physical changes | Presentation | Comments |
|---|---|---|
| Edema |  |
– Observed as perceptible increase in volume of fluid in skin and subcutaneous tissue, characteristically indented with external finger pressure – Usually occurs first in ankle region where the long saphenous vein is most superficial and curved but may extend to leg and foot – Worsens with dependency and improves with leg elevation (Carmel & Bryant, 2016). |
| Stasis changes |  |
– Eczematous changes make the skin vulnerable with redness and scaling (stasis dermatitis) often associated with pruritus – Management involves the use of emollients, humectant moisturizers or topical corticosteroids if red & inflamed – Contact irritant dermatitis & allergies may occur with some topical agents |
| Hemosiderin Staining (Hemosiderosis) Hyperpigmentation |  |
– When vein valves fail & red blood cells are forced out of capillaries, they break down releasing hemosiderin pigment + melanin, results in gray-brown gaiter skin pigmentation (mod. from Carmel & Bryant, 2016) |
| Corona phlebectatica (starburst veins radiating below the malleoli above and onto the side of the foot) |  |
– Fan-shaped pattern of numerous small intradermal veins on medial or lateral malleoli – Often an early sign of advanced venous disease Also known as malleolar flare or ankle flare – “The corona phlebectatica (CP) abnormally visible cutaneous blood vessels at the ankle with 4 components: venous cups, telangiectasias – blue* & red, capillary stasis spots* *most important elements.”(Uhl et al., 2012) |
| Varicosities |  |
– Usually tortuous, but tubular saphenous veins with reflux may be classified as varicose veins (varix, varices, or varicosities) – Blue colour, swollen, twisted, superficial or deep – Common locations: ankle, back of the calf or medial aspect of the leg (Carmel & Bryant, 2016) |
| Acute Lipodermatosclerosis (LDS) |
 |
– Acute lipodermatosclerosis presents with an extremely painful (even to light touch) red to purple indurated warm area on the lower leg – Often misdiagnosed as cellulitis, phlebitis, panniculitis or acute morphea – Progression-months/years to chronic – More likely bilateral than cellulitis (3° Fahrenheit warmer than the mirror image on the other leg) – Acute lipodermatosclerosis often transitions to subacute or chronic changes (Miteva, 2010) |
| Chronic Lipodermatosclerosis (LDS) |
 |
– Localized chronic inflammation and fibrosis of dermal skin and subcutaneous tissues of lower leg, sometimes associated with scarring or contracture of Achilles tendon – LDS may be proceeded by diffuse inflammatory edema of the skin that may be painful; referred to as acute LDS – The chronic form is part of severe venous disease or C4 in the CEAP classification (Carmel & Bryant, 2016) |
| Inverted champagne bottle deformity | 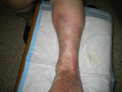 |
– This is a form of lipodermatosclerosis with subcutaneous fibrosis that leads to proximal leg swelling with skin tightening & narrowing band at the distal calf (gaiter area) |
| Atrophy blanche |  |
– Localized, often circular whitish & atrophic areas (hypopigmented) surrounded by dilated capillaries & may have hyperpigmentation. Often described as porcelain white scars – When vein valves fail & red blood cells are forced out of capillaries, they break down releasing hemosiderin pigment + melanin, results in gray-brown gaiter skin pigmentation (mod. from Carmel & Bryant, 2016) – Atrophy blanche is common, occurring in 1/3 of patients with venous disease but also may represent livedoid vasculopathy in 50% of cases, especially if the changes extend to the dorsal base of the toes (Alavi et al., 2014) – Associated with coagulation abnormalities in 50% – Atrophy blanche pain due to vascular occlusion (Alavi et al., 2014, Carmel & Bryant, 2016) |
| Venous ulcer |  |
– Full-thickness defect of the skin, most frequently in ankle or lower gaiter region, that fails to heal spontaneously and is sustained by CVD – Ulcers often have a granulation tissue base (firm pink) with serpiginous margins (irregular snake-like) and are less likely to have eschar, debris, or tendons in the base of the ulcer |
Reproduced with permission: Wound Care Canada



