Measurement
MEASURE
Wound measurement is often a good indicator of wound healing (Keast et al., 2004). Appropriate equipment such as a cotton tip applicator and measurement ruler should be used in the determination of wound measurements (Goldman & Salcido, 2002). Wound measurement (surface area in cm2) is calculated using the “longest length” on the surface in any direction, followed by the “widest width” that runs perpendicular (right angle) to the length (Sibbald et al., 2021). Depth is measured at the deepest portion of the wound (Keast et al., 2004) (Figure 3).
Figure 3– Wound Measurement
 |
|
When measuring a wound, consistency of documentation is crucial. There are 2 methods to measure a wound. 1. measuring the longest length and the widest width at a 90-degree angle to the longest length. 2. measuring using the head-to-toe measurement. Having a policy at your institution or place of employment will enable wound size to be more consistently and accurately documented. |
Wound measurement is obtained on the first assessment and should be reassessed at least weekly or as institutional policies require. Unlike chronic wounds, acute wounds follow a normal healing process, closing within 21 days (Keast & Orsted, 1998). In chronic wounds, wound size is expected to decrease by 20-40% within 4 weeks to ensure that wounds close by week 12 (Woo & Sibbald, 2009). Therefore, by measuring wounds at least on a weekly basis will help determine if wounds are progressing.
EXUDATE
Wound exudate may vary in amount and type. For example, a patient with a venous leg ulcer with edema, may have copious drainage while a patient with an intact eschar may have no exudate. Frequency of dressing changes, size of the products selected and wound characteristics are some examples that influence product selection for management of exudate (See Figure 3).
It is also important to describe the type of exudate on the wound surface as being serous (clear), serosanguineous (clear + bloody), sanguineous (bloody) or purulent (green or tan) (Keast et al., 2004). The type and volume of exudate should also be described. The most predominant feature of the exudate should be described first e.g. serosanguineous has more clear serum and small amounts of blood.
APPEARANCE
The appearance of the wound bed is a good indicator of the progression of wound closure. Other useful observations may include presence of bone (osteomyelitis), ligament, tendon or foreign body. There are four main tissue types of the wound bed (Figure 9.4):
- healthy granulation (pink, firm, moist)
- epithelialization (new, natural, thin protective layer, often a light purple colour)
- necrotic tissue (black or brown, firm or hard)
- slough (yellow, soft, wet, loose)
Wound appearance assessment is documented by percentages of tissue type observed relative to the entire wound bed size.
Table 2 – Four tissue types. Photos: Courtesy ©L.Goodman
 |
Granulation (light red to pink)
|
 |
Epithelization (light purple)
|
 |
Slough (yellow or grey)
|
 |
Necrotic (black or brown)
|
SUFFERING
The wound pain score, type of pain and characteristics should be captured as part of the documentation.
UNDERMINING
Undermining or tunneling may also be seen underneath the borders of a wound. Undermining covers large areas or quadrants, while tunnels are narrow caverns that burrow towards a single direction (Wound Ostomy & Continence Nurses Society, 2010) (See Figure 4 ).
To appropriately locate the position of a tunnel or undermined area, imagine the wound as a clock with the 12 o’clock edge pointing towards the head of the patient and 6 o’clock to the feet (Keast et al., 2004; Sibbald et al., 2021) (See Figure 4 ). Use a sterile cotton-tip applicator to gently probe and measure the extent of undermining and tunneling e.g. a tunnel is 3cm deep at 4 o’clock. Identifying such areas can help ensure that they are packed appropriately to facilitate healing and communicates where dressing material needs to be removed from.
Figure 4 – Areas of Undermining & Tunneling (Clock Method)
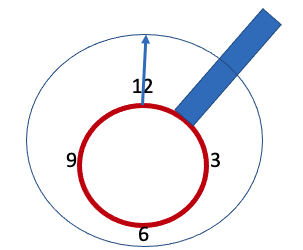 |
| Script : Measurement of undermining and tunneling is best accomplished by using the clock method for documentation. Using a sterile probe and document the measurements at 12 o’clock, 3 o’clock, 6 o’clock and 9 o’clock. It is important to document the anatomical location of the 12 o’clock measurement for consistency especially if the wound is on the foot.
|
It is important to obtain a wound measurement (including areas of undermining or tunneling) using a consistent method to ensure accuracy and reliability.
RE-EVALUATE
Comprehensive wound assessment and patient progress should be re-evaluated as necessary and according to institutional policies.
EDGE
Wound assessment goes beyond the surface of the wound and should also include an assessment of the wound edges and the periwound skin (4 cm beyond the wound). To support wound closure, wound edges should be like “the shore of a sandy beach” where the new epithelial tissue advances smoothly along the wound surface. Some wounds have a “cliff-like edge” or rolled edges (epibole), usually indicating chronicity because the epithelium falsely believes healing is complete. This type of wound edge inhibits epithelial tissue advancement resulting in delayed wound healing (Fletcher & Probst, 2020).
Maintaining a healthy periwound is a vital component of local wound care. Periwound skin should be assessed for:
- maceration (indicative of excessive moisture, white over hydrated skin)
- erythema (red, indurated)
- excoriation (linear erosion or ulcer)
- edema (swelling)
- thick callus (thickened epidermis)
- new areas of breakdown (possible sign of infection)
Early recognition and intervention are necessary to prevent overall wound deterioration but not treating the cause or trauma may also be responsible.
Infection
Wound infection results in impaired wound healing. The validated NERDS and STONEES tool may be used to assess and document potential superficial and deep and surrounding tissue infection.
Treatment
Documentation should also include local wound care plans and response to treatment. This process will help other clinicians to determine what preventative strategies, local dressings or cleansers were used and how it may have influenced the wound parameters being monitored.
| V – Vascular: ABPI confirms adequate arterial blood supply for healing I – Infection: NERDS and STONEES criteria (odour, pain, exudate) – consider topical antimicrobial treatment; possibly systemic antibiotic therapy based on other factors P – Pressure: High compression therapy indicated due to absence of arterial disease once pain is under control and patient tolerates S – Sharp surgical debridement: Depending on the wound bed appearance Other – Normal saline appropriate for cleansing |

