7.2 Stress
In this section:
Stress and Stressors
Emotions matter because they influence our behavior. And there is no emotional experience that has a affect more powerful influence on us than stress.
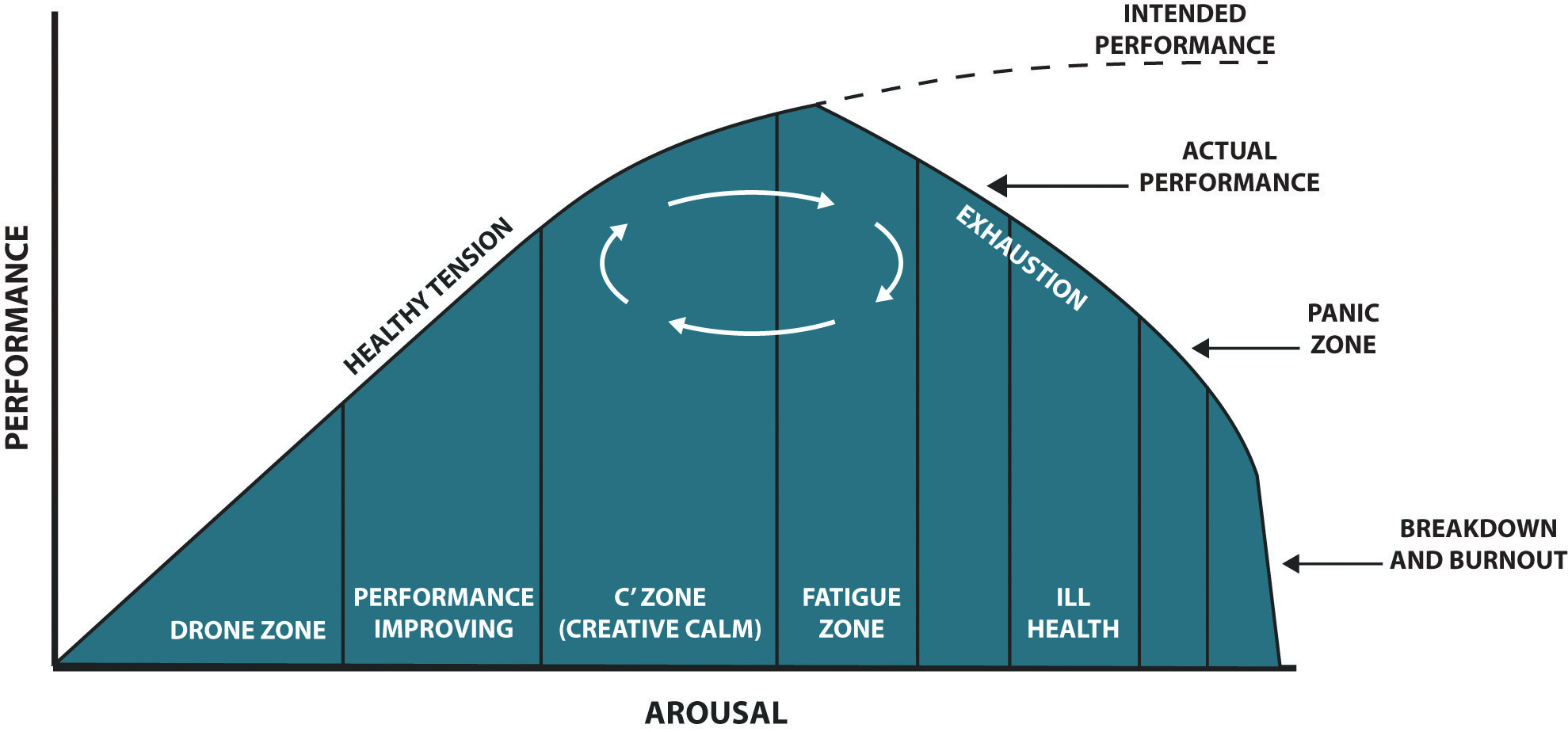
Stress is a function of the objective environment but also of individuals’ subjective interpretation of events and their consequences. Both body and mind are involved the process. It is important for both firms and individuals to take preventive measures before the cumulative effects of stress manifest themselves in ways that cost both the individual and the company. Stress can have a positive effect, making us more alert or more prepared to take on an important challenge. Stress can also have a negative effect, causing a range of physical and mental ailments.
Eustress is a term that signifies beneficial stress, either psychological, physical. The term was coined by using the Greek prefix “eu”, meaning “good”, and stress, literally meaning “good stress”. Eustress was originally explored in a stress model by Richard Lazarus. It is the positive cognitive response to stress that is healthy, or gives one a feeling of fulfilment or other positive feelings (Nelson et al., 2004; Lazarus, 1966).
Under stress, individuals are unable to respond to environmental stimuli without undue psychological and/or physiological damage, such as chronic fatigue, tension, or high blood pressure. This damage resulting from experienced stress is usually referred to as strain.
Stressors
We all experience stress at some point in our lives. Situations causing stress are known as stressors. There are four types of stressors:
- Acute stressors are time-specific events of high intensity and short duration that occur infrequently, such as a performance review, a car accident, or unexpected encounter.
- Episodic (or daily) stressors may be similar to acute stressors but occur more frequently, have a longer duration, and may be of lower intensity. Making repeated requests of a worker to work overtime is an example of an episodic stressor.
- Chronic stressors are stressors that persist over a sustained period of time, and include job insecurity, work overload, or lack of control.
- Catastrophic stressors are a subset of acute stressors but differ in their intensity, threatening life, safety, or property. Robbery and physical assault are examples of catastrophic stressors.
Thomas Holmes and Richard Rahe (1967) developed a measure of some everyday life events that might lead to stress. Rahe and his colleagues (1970) asked 2,500 members of the military to complete the rating scale and then assessed the health records of the soldiers over the following 6 months. The results were clear: The higher the scale score, the more likely the soldier was to end up in the hospital. Although some of the items on the Holmes and Rahe scale are major, even minor stressors add to the total score. Our everyday interactions with the environment that are essentially negative, known as daily stressors or hassles, can also create stress, as well as poorer health outcomes (Hutchinson & Williams, 2007). Events that may seem rather trivial altogether, such as having an argument with a friend or getting cut off by another car in rush-hour traffic, can produce stress (Fiksenbaum et al., 2006). Glaser (1985) found that medical students who were tested during, rather than several weeks before, their school examination periods showed lower immune system functioning. Other research has found that even more minor stressors, such as having to do math problems during an experimental session, can compromise the immune system (Cacioppo et al., 1998).
Self-assessment
See Appendix B: Self-Assessments
Place a check mark next to each event you experienced within the past year. Then add the scores associated with the various events to derive your total life stress score.
Responses to Stress
Not all people experience and respond to stress in the same way, and these differences can be important. The cardiologists Meyer Friedman and R. H. Rosenman (1974) were among the first to study the link between stress and heart disease. In their research, they noticed that even though the partners in married couples often had similar lifestyles, diet, and exercise patterns, the husbands nevertheless generally had more heart disease than did the wives. As they tried to explain the difference, they focused on the personality characteristics of the partners, finding that the husbands were more likely than the wives to respond to stressors with negative emotions and hostility.
Recent research has shown that the strongest predictor of a physiological stress response from daily hassles is the amount of negative emotion that they evoke. People who experience strong negative emotions as a result of everyday hassles and who respond to stress with hostility experience more negative health outcomes than do those who react in a less negative way (McIntyre et al., 2008; Suls & Bunde, 2005). Williams and his colleagues (2001) found that people who scored high on measures of anger were three times more likely to suffer from heart attacks in comparison with those who scored lower on anger.
On average, men are more likely than are women to respond to stress by activating the fight-or-flight response, which is an emotional and behavioral reaction to stress that increases the readiness for action. The arousal that men experience when they are stressed leads them to either go on the attack, in an aggressive or revenging way, or else retreat as quickly as they can to safety from the stressor. The fight-or-flight response allows men to control the source of the stress if they think they can do so, or if that is not possible, it allows them to save face by leaving the situation. The fight-or-flight response is triggered in men by the activation of the HPA axis.
Women, on the other hand, are less likely to take a fight-or-flight response to stress. Rather, they are more likely to take a tend-and-befriend response (Taylor et al., 2000). The tend-and-befriend response is a behavioral reaction to stress that involves activities designed to create social networks that provide protection from threats. This approach is also self-protective because it allows the individual to talk to others about her concerns as well as to exchange resources, such as child care. The tend-and-befriend response is triggered in women by the release of the hormone oxytocin, which promotes affiliation. Overall, the tend-and-befriend response is healthier than the flight-or-flight response because it does not produce the elevated levels of arousal related to the HPA, including the negative results that accompany increased levels of cortisol. This may help explain why women, on average, have less heart disease and live longer than men.
The experience of long-term stress—and its potential negative impact on our physical and mental health—represents one example of the powerful influence of the social situation in our everyday lives. These findings represent social psychological principles in action: Our affect, cognition, and behavior are influenced in profound ways by the events that occur to us, and particularly by the people around us.
Stress and the Immune System
We experience stress when we find ourselves in situations where we are not sure how to respond or whether we are going to be able to adequately cope. Extreme social situations, such as being the victim of a terrorist attack, a natural disaster, or a violent crime, may produce an extreme form of stress known as post-traumatic stress disorder (PTSD),a medical syndrome that includes symptoms of anxiety, sleeplessness, nightmares, and social withdrawal.
Stress is accompanied by increases in arousal. When we experience stress, our heart rate, breathing, and blood pressure increase, and our body begins to secrete adrenaline and other hormones. Perspiration increases to cool down the body. In addition, sugar is released to provide energy, and the pupils dilate to improve our vision. At the same time, the less immediately essential body activities controlled by the parasympathetic nervous system (PNS), including digestion, are reduced in order to divert more energy to allow the body to react to the threat.
The experience of stress likely had positive aspects for human beings in an evolutionary sense. When we are attacked, afraid, or concerned about our welfare, the body signals us that we need to react, and the stress response is one of those signals. But problems begin when a threat continues over time. When it is extreme or prolonged, stress can create substantial negative mental and physical effects. In fact, when stress occurs for too long, it can lead to exhaustion and even death.
General Adaptation Syndrome
The physiologist Hans Seyle (1907–1982) studied stress by examining how rats responded to being exposed to stressors such as extreme cold, infection, shock, and excessive exercise. Seyle found that regardless of the source of the stress, the rats experienced the same series of physiological changes as they suffered the prolonged stress. Seyle created the term general adaptation syndrome to refer to the three distinct phases of physiological change that occur in response to long-term stress: alarm, resistance, and exhaustion. These phases are explained in Figure 7.7 below.
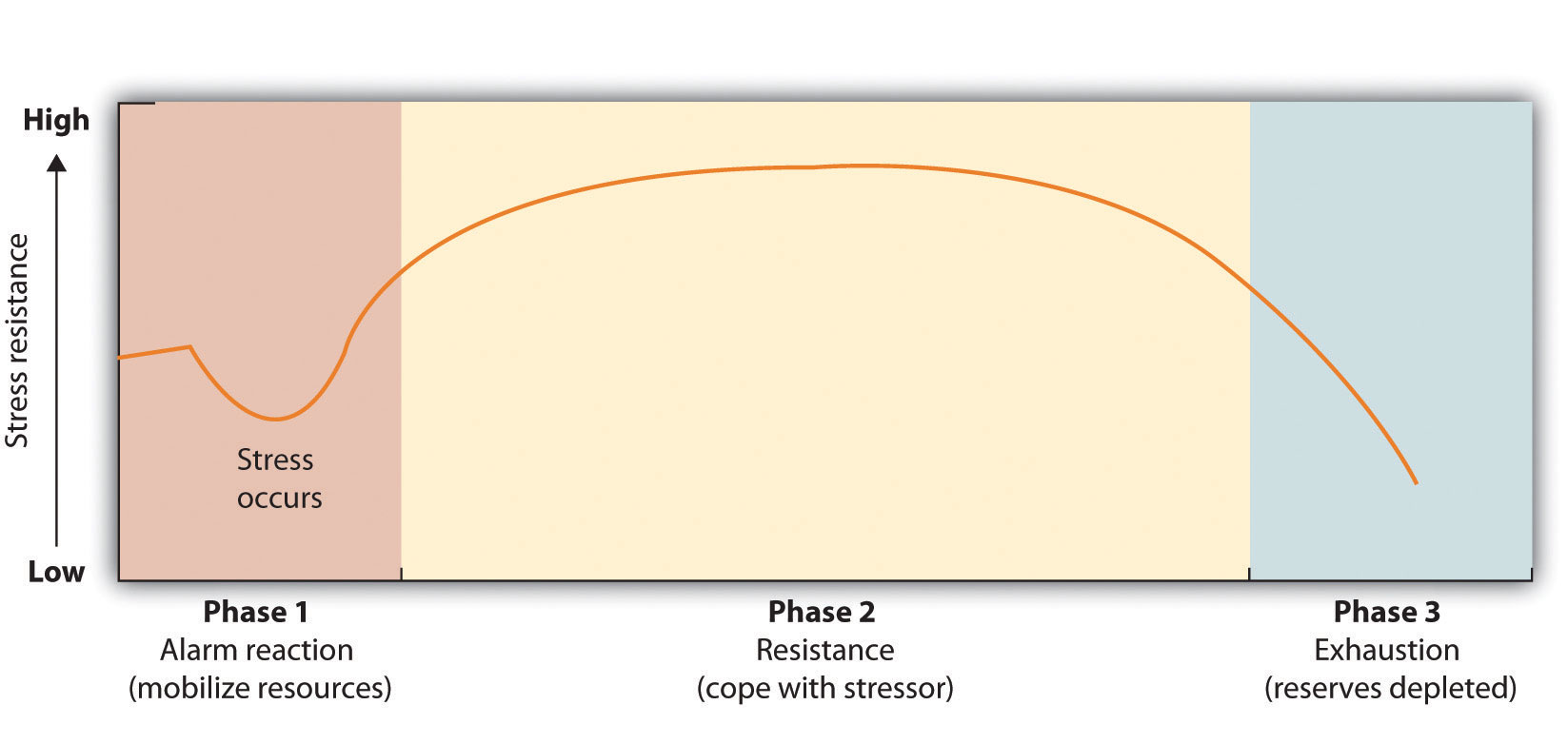
Stage one:
- General alarm reaction. The first reaction to stress The body releases stress hormones, including cortisol
Stage two:
- Resistance. After a period of chronic stress the body adapts to the ongoing threat and tries to its normal function. Glucose levels increase to sustain energy, and blood pressure increases.
Stage three:
- Exhaustion. In this stage, the body has run out of its reserves of energy and immunity. Blood sugar levels decrease, leading to decreased stress tolerance, progressive mental and physical exhaustion, illness, and collapse. The body’s organs being to fail, and eventually illness or death occurs.
The experience of stress creates both an increase in general arousal in the sympathetic nervous system (SNS) and another, even more complex, system of physiological changes through the HPA axis. The HPA axis is a physiological response to stress involving interactions among the hypothalamus, the pituitary gland, and the adrenal glands. The HPA response begins when the hypothalamus secretes hormones that direct the pituitary gland to release the hormone ACTH. The ACTH then directs the adrenal glands to secrete more hormones, including epinephrine, norepinephrine, and cortisol, a stress hormone that releases sugars into the blood to help prepare the body to respond to threat (Rodrigues et al., 2009).
Cortisol is frequently referred to as the “stress hormone,” and it is commonly measured by researchers in order to assess the activation of the HPA axis in response to stress. Cortisol is measured by taking a sample of saliva, which is then analyzed to determine cortisol levels. Cortisol increases when people are stressed, for instance, when they are in dancing competitions (Edelstein et al., 2010), when they are experiencing public shame (Rohleder et al., 2008), and (I’m sure you won’t be surprised) when taking school exams (Preuss et al., 2010).
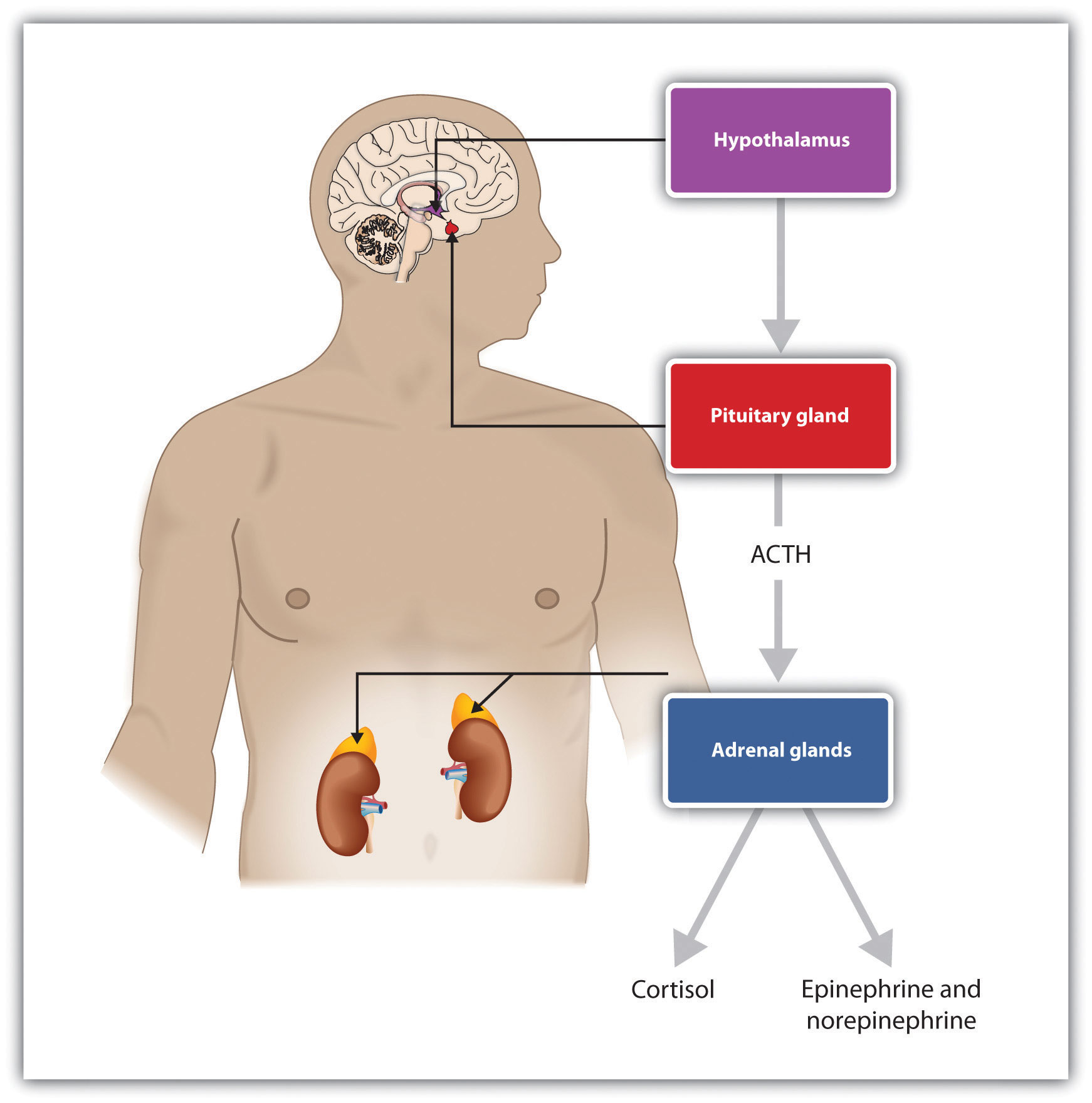
The experience of prolonged stress has a direct negative influence on our physical health because at the same time that stress increases activity in the SNS, it also suppresses important activity in the PNS. When stress is long-term, the HPA axis remains active and the adrenals continue to produce cortisol. This increased cortisol production exhausts the stress mechanism, leading to fatigue and depression.
The HPA reactions to persistent stress lead to a weakening of the immune system, making us more susceptible to a variety of health problems, including colds and other diseases (Cohen & Herbert, 1996; Faulkner & Smith, 2009; Miller et al., 2009; Uchino et al., 2007). Stress also damages our DNA, making us less likely to be able to repair wounds and respond to the genetic mutations that cause disease (Epel et al., 2006). As a result, wounds heal more slowly when we are under stress, and we are more likely to get cancer (Kiecolt-Glaser et al., 2002; Wells, 2006).
Sheldon Cohen and colleagues (1998) demonstrated experimentally that repeated exposure to threats and stress can increase susceptibility to the common cold virus, revealing the causal link between psychological stress and actual susceptibility to disease. To begin, the researchers had adult volunteers fill out several questionnaires about the stressful experiences in their lives. Then the researchers administered nose drops into each participant’s nose. The control group (the lucky ones!) received a placebo saline solution; the experimental group received a solution containing a cold virus. Over the next week, the participants were examined daily by a nurse. None of the control group participants got a cold. But of those exposed to the cold virus, 82% did get a cold. Furthermore, within this condition, those participants who reported enduring long-term stressors—particularly those who felt that they were underemployed or who had enduring interpersonal difficulties with family or friends—were significantly more likely to catch colds than those who had only short-term stress.
As previously mentioned, chronic stress is also a major contributor to heart disease. Although heart disease is caused in part by genetic factors, as well as by high blood pressure, high cholesterol, and cigarette smoking, it is also caused by stress (Krantz & McCeney, 2002). Long-term stress creates two opposite effects on the coronary system. Stress increases cardiac output (i.e., the heart pumps more blood) at the same time that it reduces the ability of the blood vessels to conduct blood through the arteries, as the increase in levels of cortisol leads to a buildup of plaque on artery walls (Dekker et al., 2008). The combination of increased blood flow and arterial constriction leads to increased blood pressure (hypertension), which can damage the heart muscle, leading to heart attack and death.
Managing Stress
We all experience stress at one time or another. However, we can take action to assess and relieve the stress in our life. First, we do some self-analysis to determine the stressors in our life and how we handle it. This emotional intelligence skill (self-awareness) allows us to see what we need to improve upon. Then, we can apply self-management tools to help us manage the stress in our lives. The benefit of this identification and management is that it allows us to relate better to others both in our work life and personal life.
Look at your habits and emotions and really think about what is causing the stress. For example, Julie may be stressed about a project due on Friday, but the real stress may be because she procrastinated in starting the project, and now there isn’t enough time to complete it. Or perhaps Gene is stressed because his personality type causes him to put too many things on his to-do list, and he isn’t able to get them done. Accepting responsibility for the role we play in our own stresses can be the first step in maintaining a life with mostly positive stress!
Next, we can look at the way we currently deal with stress. For example, when Emily is feeling stressed, she smokes a pack of cigarettes and tends to have several glasses of wine at night. When she isn’t stressed, she doesn’t smoke and may limit herself to just one or two glasses of wine every few days. Some people smoke cannabis or use other drugs to cope with the stress of everyday life. These substances seemingly help for a period of time but prevent us from actually dealing with the stress—and doesn’t help us to gain skills in self-awareness. Understanding your current coping mechanisms for stress can help you determine what works to manage stress—and what doesn’t.
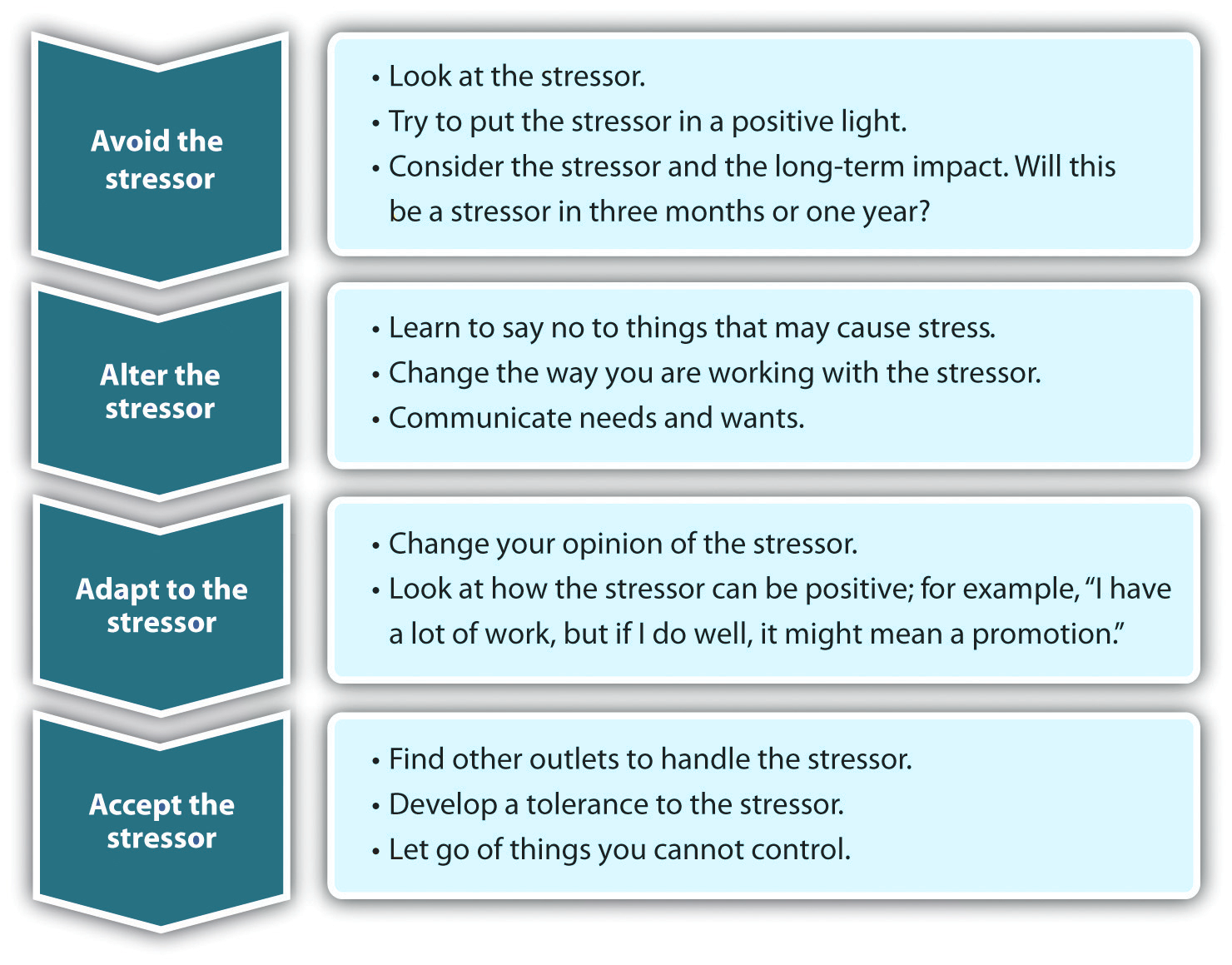
Once we do some self-analysis, we can use a method called the four As. The four As gives us four choices for dealing with a stressor:
Avoid the Stressor
We can try to avoid situations that stress us out. If watching certain television programs causes stress, stop watching them! Spend time with people who help you relax. We can also look at saying no more often if we do not have the time necessary to complete everything we are doing. As we have already learned, avoiding some problems and conflicts can be a temporary solution, but ultimately make the situation worse.
Alter the Stressor
Another option in dealing with stress is to try to alter it, if you can’t avoid it. When changing a situation, you can be more assertive, manage time better, and communicate your own needs and wants better. For example, Karen can look at the things causing her stress, such as her home and school commitments; while she can’t change the workload, she can examine ways to avoid a heavy workload in the future. If Karen is stressed about the amount of homework she has and the fact that she needs to clean the house, asking for help from roommates, for example, can help alter the stressor. Often this involves the ability to communicate well.
Adapt to the Stressor
If you are unable to avoid or change the stressor, getting comfortable with the stressor is a way to handle it. Creating your own coping mechanisms for the stress and learning to handle it can be an effective way to handle the stress. For example, we can try looking at stressful situations in a positive light, consider how important the stressor is in the long run, and adjust our standards of perfectionism.
Accept the Stressor
Some stressors are unavoidable. We all have to go to work and manage our home life. So, learning to handle the things we cannot change by forgiving, developing tolerances, and letting going of those things we cannot control is also a way to deal with a stressor. For example, if your mother-in-law’s yearly visits and criticisms cause stress, obviously you are not able to avoid or alter the stress, but you can adapt to it and accept it. Since we cannot control another person, accepting the stressor and finding ways of dealing with it can help minimize some negative effects of the stress we may experience.
Now that we’ve explored the nature of stress, in general, let’s turn our attention to stress and stressors in the workplace.
Adapted Works
“Manage Your Stress” in Human Relations by Saylor Academy is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License without attribution as requested by the work’s original creator or licensor.
“Emotions, Stress, and Well-Being” in Principles of Social Psychology by University of Minnesota is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
References
Cacioppo, J. T., Berntson, G. G., Malarkey, W. B., Kiecolt-Glaser, J. K., Sheridan, J. F., Poehlmann, K. M., Burleson, M. H., Ernst, J. M., , Hawkley, L. C., & Glaser, R. (1998, May). Autonomic, neuroendocrine, and immune responses to psychological stress: The reactivity hypothesis. Annals of the New York Academy of Sciences: Neuroimmunomodulation: Molecular aspects, integrative systems, and clinical advances, 840, 664–673. DOI: 10.1111/j.1749-6632.1998.tb09605.x
Cohen, S., Frank, E., Doyle, W. J., Skoner, D. P., Rabin, B. S., & Gwaltney, J. M. Jr. (1998). Types of stressors that increase susceptibility to the common cold in adults. Health Psychology, 17, 214–23.
Cohen, S., & Herbert, T. B. (1996). Health psychology: Psychological factors and physical disease from the perspective of human psychoneuroimmunology. Annual Review of Psychology, 47, 113–142.
Dekker, M., Koper, J., van Aken, M., Pols, H., Hofman, A., de Jong, F.,…Tiemeier, H. (2008). Salivary cortisol is related to atherosclerosis of carotid arteries. Journal of Clinical Endocrinology and Metabolism, 93(10), 3741.
Diener, E., Suh, E. M., Lucas, R. E., & Smith, H. L. (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125(2), 276–302.
Edelstein, R. S., Yim, I. S., & Quas, J. A. (2010). Narcissism predicts heightened cortisol reactivity to a psychosocial stressor in men. Journal of Research in Personality, 44(5), 565–572.
Epel, E., Lin, J., Wilhelm, F., Wolkowitz, O., Cawthon, R., Adler, N.,…Blackburn, E. H. (2006). Cell aging in relation to stress arousal and cardiovascular disease risk factors. Psychoneuroendocrinology, 31(3), 277–287.
Faulkner, S., & Smith, A. (2009). A prospective diary study of the role of psychological stress and negative mood in the recurrence of herpes simplex virus (HSV1). Stress and Health: Journal of the International Society for the Investigation of Stress, 25(2), 179–187.
Fiksenbaum, L. M., Greenglass, E. R., & Eaton, J. (2006). Perceived social support, hassles, and coping among the elderly. Journal of Applied Gerontology, 25(1), 17–30.
Friedman, M., & Rosenman, R. H. (1974). Type A behavior and your heart. Knopf.
Glaser, R. (1985). Stress-related impairments in cellular immunity. Psychiatry Research, 16(3), 233–239.
Higgins, E. T., Bond, R. N., Klein, R., & Strauman, T. (1986). Self-discrepancies and emotional vulnerability: How magnitude, accessibility, and type of discrepancy influence affect. Journal of Personality and Social Psychology, 51(1), 5–15.
Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of Psychosomatic Research, 11, 213–218.
Hutchinson, J. G., & Williams, P. G. (2007). Neuroticism, daily hassles, and depressive symptoms: An examination of moderating and mediating effects. Personality and Individual Differences, 42(7), 1367–1378.
Kiecolt-Glaser, J. K., McGuire, L., Robles, T. F., & Glaser, R. (2002). Psychoneuroimmunology: Psychological influences on immune function and health. Journal of Consulting and Clinical Psychology, 70(3), 537–547.
Krantz, D. S., & McCeney, M. K. (2002). Effects of psychological and social factors on organic disease: A critical assessment of research on coronary heart disease. Annual Review of Psychology, 53, 341–369.
Lazarus, R. S. (1966). Psychological stress and the coping process. McGraw-Hill Book Co.
Lazarus, R. S. (2000) Toward better research on stress and coping. American Psychologist, 55, 665–673.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. Springer Publishing Company.
McIntyre, K., Korn, J., & Matsuo, H. (2008). Sweating the small stuff: How different types of hassles result in the experience of stress. Stress & Health: Journal of the International Society for the Investigation of Stress, 24(5), 383–392. doi:10.1002/smi.1190
Miller, G., Chen, E., & Cole, S. W. (2009). Health psychology: Developing biologically plausible models linking the social world and physical health. Annual Review of Psychology, 60, 501–524.
Nelson, D. L., Simmons, B. L., Perrewé, P. L., &; Ganster, D. C. (2004). Eustress: An elusive construct an engaging pursuit (1st ed.). Elsevier Jai.
Preuss, D., Schoofs, D., Schlotz, W., & Wolf, O. T. (2010). The stressed student: Influence of written examinations and oral presentations on salivary cortisol concentrations in university students. Stress: The International Journal on the Biology of Stress, 13(3), 221–229.
Rahe, R. H., Mahan, J., Arthur, R. J., & Gunderson, E. K. E. (1970). The epidemiology of illness in naval environments: I. Illness types, distribution, severities and relationships to life change. Military Medicine, 135, 443–452.
Rodrigues, S. M., LeDoux, J. E., & Sapolsky, R. M. (2009). The influence of stress hormones on fear circuitry. Annual Review of Neuroscience, 32, 289–313.
Rohleder, N., Chen, E., Wolf, J. M., & Miller, G. E. (2008). The psychobiology of trait shame in young women: Extending the social self-preservation theory. Health Psychology, 27(5), 523–532.
Strauman, T. J., & Higgins, E. T. (1988). Self-discrepancies as predictors of vulnerability to distinct syndromes of chronic emotional distress. Journal of Personality, 56(4), 685–707.
Suls, J., & Bunde, J. (2005). Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin, 131(2), 260–300.
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A. R., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411–429.
Uchino, B. N., Smith, T. W., Holt-Lunstad, J., Campo, R., & Reblin, M. (2007). Stress and illness. In J. T. Cacioppo, L. G. Tassinary, & G. G. Berntson (Eds.), Handbook of psychophysiology (3rd ed., pp. 608–632). Cambridge University Press.
Wells, W. (2006). How chronic stress exacerbates cancer. Journal of Cell Biology, 174(4), 476.
Williams, R. B. (2001). Hostility: Effects on health and the potential for successful behavioral approaches to prevention and treatment. In A. Baum, T. A. Revenson, & J. E. Singer (Eds.), Handbook of health psychology. Lawrence Erlbaum Associates.

