1. Do people experiencing homelessness use emergency medical services at a high rate?
In the previous chapter, on Primary Care & Nursing, we examined the inequities that people who experience homelessness face in accessing health care. Research has consistently shown that most people who experience homelessness do not have a primary care provider, such as a Physician or Nurse Practitioner. We also saw in the previous chapter that many people who experience homelessness have chronic health conditions and that these conditions emerge at a premature age. Given this information, we begin this chapter on Emergency Medicine by considering whether people experiencing homelessness may perhaps turn to medical services, such as hospital emergency departments, as a foreseeable outcome. Before you continue through the material, we invite you to consider this question and record your thoughts in the space below. You may write as little or as much as you would like.
How to complete this activity and save your work: Type your response to the question in the box below. When you are done answering the question navigate to the ‘Export’ page to download and save your response. If you prefer to work in a Word document offline you can skip right to the Export section and download a Word document with this question there.
By now you likely know that the premise of this book is to ask simple questions that actually have rather complex answers. However, you may be wondering why we asked such a simple question to begin this chapter. Do people experiencing homelessness use emergency medical services at a high rate? This seems like a yes or no answer, so how can we write an entire section about it? Each of the researchers we posed this question to answered with a yes, and then followed it with a “but.” Yes, people who experience homelessness do use emergency medical services at a high rate, but… It is what comes after the “but” that makes this a seemingly simple question with a rather complex answer.
We begin with a video of Dr. Cheryl Forchuk that was recorded while she was onsite at a hospital during the COVID-19 pandemic in the summer of 2021. Dr. Forchuk’s research has shown a connection between homelessness and hospitalization for COVID-19. Notably, participants in her team’s study who had a recent history of homelessness were more likely to be tested for COVID-19 and to have the test return positive (Richard et al., 2021). Further, participants of the study with a recent history of homelessness were found to be 20 times more likely to be admitted to hospital for COVID-19, over 10 times more likely to require intensive care, and over 5 times more likely to die within 21 days of their first positive test result (Richard et al., 2021). In the video below, Dr. Forchuk explains further.
 When the videos in this ebook are almost done playing, the message “Stop the video now” will appear in the top left corner. This is a reminder for those who have turned on the Autoplay setting to manually pause the video when the speakers are done to avoid having it autoplay through to the next video. This message will appear in all researcher videos throughout the ebook.
When the videos in this ebook are almost done playing, the message “Stop the video now” will appear in the top left corner. This is a reminder for those who have turned on the Autoplay setting to manually pause the video when the speakers are done to avoid having it autoplay through to the next video. This message will appear in all researcher videos throughout the ebook.
Note: Viewers may still need to use their discretion in stopping other YouTube content such as ads.
Dr. Cheryl Forchuk: Do people who experience homelessness use emergency medical services at a high rate?
In this video, filmed at a hospital during the COVID-19 pandemic, Dr. Cheryl Forchuk explains that the literature shows people who experience homelessness are more likely to use emergency medical services but that the figures vary by study. She notes that when individuals experiencing homelessness go to the hospital, they have higher rates of admission, longer stays, and increased rates of readmission compared to housed patients. This video is 0:39 in length and has closed captions available in English.
Key Takeaways – Dr. Cheryl Forchuk: Do people who experience homelessness use emergency medical services at a high rate?
- The literature shows that people who experience homelessness tend to use emergency medical services more than housed individuals, but the estimated rates vary by study.
- People who experience homelessness are also more likely to be admitted to hospital and have longer stays than housed patients.
- Patients who are discharged into homelessness (i.e. to a shelter, the street, or another insecure housing situation) are more likely to be readmitted to hospital.
Dr. Forchuk explains that people who experience homelessness do use emergency medical services at a high rate, but that the estimates vary across studies. Researchers use different methodologies for collecting data about homelessness and emergency department use, such as through surveys, interviews, and focus groups, that can produce different estimates. However, we can also learn a lot about homelessness and people’s access to medical services from administrative health records (Wiens, Rosella, Kurdyak, & Hwang, 2020). For instance, A review of administrative health data from emergency departments in Ontario between 2010 and 2017 identified 39,408 patients who were experiencing homelessness and also showed that the number of emergency department visits increased over the period of study (Strobel et al., 2021). These researchers found that the number of visits were at their highest annually in September and at their lowest each year in January, with hospital visits more highly concentrated in urban centres (Strobel et al., 2021). This study shows how administrative health data can help us learn more about the demographics and characteristics of people experiencing homelessness, by serving as both point-in-time and longitudinal sources of information (Strobel et al., 2021). We invite you to learn more about this study and its findings in this section’s featured reading below.
Featured Reading:
Strobel, S., Burcul, I., Dai, J. H., Ma, Z., Jamani, S., & Hossain, R. (2021). Characterizing people experiencing homelessness and trends in homelessness using population-level emergency department visit data in Ontario, Canada. Ottawa: Statistics Canada, Health Reports.
Administrative health data, as well as self-reports, are important sources of information for understanding the reasons some people who experience homelessness use emergency medical services at a higher rate. We say “some people” because it must be noted not every person who experiences homeless uses hospitals at a high rate. Rather, what our own research shows is that there is a small percentage who use hospitals on a frequent basis. We conducted surveys, interviews, and hospital record reviews for 52 people experiencing homelessness or housing insecurity in a small semi-rural town in Ontario. This review showed that in the preceding year over half (54%) had visited the hospital. These 28 individuals collectively went to the hospital 76 times, for medical (79%), mental health (17%) and dental (4%) reasons. While 28 of the 52 participants had been to the hospital in the preceding year, 6 were found to be frequent users and another 2 were highly frequent users, accounting for 15 and 28 of the total hospital visits respectively. Collectively these 8 individuals, who accounted for 15% of the sample, produced 75% of the hospital visits for people in this study in 2018 (Gilmer & Buccieri, 2020).
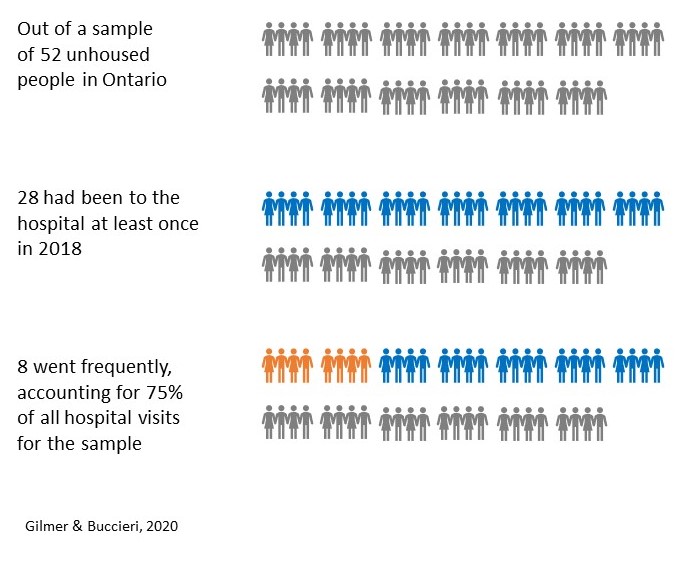
It is clear from this data that not every person who experiences homelessness uses hospital services but that, of those who do, a minority use it frequently. In the next video Dr. Stephen Hwang, St. Michael’s Hospital Chair in Homelessness, Housing and Health, explains in the next video why it is important we consider the reasons that people go to the hospital and not confuse high use with unnecessary use.
Dr. Stephen Hwang: Do people who experience homelessness use emergency medical services at a high rate?
In this video, Dr. Stephen Hwang explains that on average people who experience homelessness use the hospital and emergency health services at higher rates, but that it is important not to overgeneralize. He notes there is heterogeneity, as some people are very high users while others are not. Framing the issue more holistically, Dr. Hwang encourages us not to confuse high usage with unnecessary usage, but rather to notice that people experiencing homelessness who seek frequent emergency care often do so because of high rates of illness. He concludes that rather than trying to reduce emergency medical care usage, we should focus instead on improving access to primary care. This video is 3:54 in length and has closed captions available in English.
Key Takeaways – Dr. Stephen Hwang: Do people who experience homelessness use emergency medical services at a high rate?
- On average people who experience homelessness use the emergency department and hospital at higher rates – but we have to realize there is heterogeneity in that usage.
- There are a small number of people who are high users of emergency health care, but there are also a significant number of people who are unhoused and do not use emergency services more than average.
- It is important not to generalize.
- We should not confuse high usage with unnecessary usage.
- Some people who experience homelessness use emergency services and the hospital at high rates because they have high levels of illness and more need for care.
- When you take a holistic approach and ask, “Why is the person here at the hospital and does it make sense?” it often does make sense given their health status.
- Our goal should not be to reduce emergency department visits, but rather to provide better primary care to improve people’s health.
When people have high rates of chronic illness and low rates of primary care access, it is not surprising they will seek out alternative health care services, such as through a hospital’s emergency department. We said at the beginning of this section that we know as a whole people who experience homelessness use emergency medical services at higher rates, and that it is the “but” that follows we are interested in learning more about. Dr. Hwang tells us the rates are higher, but that we need to recognize people are there for legitimate medical reasons that are not being well-served through mainstream primary care services.
The link between hospital use and primary care issues is well founded in the literature. Our own research, for instance, again shows that amongst the 52 participants only 28% had a primary care provider in the city where they lived, and those who went to the hospital primarily did so for medical issues, pain, mental health support, overdose or drug-related complications, and dental care (Gilmer & Buccieri, 2020). Moderate to severe chronic pain is a common reason why people who experience homelessness seek medical treatment and is more common among people who also have major depressive disorder, post-traumatic stress disorder, and report suicidality among other conditions (Vogel et al., 2017).
It is also common that patients experiencing homelessness seek care at hospitals because they have complex health care issues that require specialized services. Research conducted at The Ottawa Hospital emergency department over a two-year period showed that during this time, 129 surgical referrals were made for 97 adults experiencing homelessness who visited the emergency department (Zuccaro, Champion, Bennett, & Ying, 2018). Of these referred patients, only 36% had a primary care physician and the majority were given surgical referrals due to traumatic injury (64%), with orthopedic surgery being the most commonly consulted service (Zuccaro et al., 2018). Another study of surgical outcomes for ankle fractures conducted in Ontario showed that, although complications are rare, patients who are marginalized are at significantly increased risk of infection and amputation following the procedure (Wolfstadt, Pincus, Kreder, & Wasserstein, 2019). What these studies collectively tell us, is that people who experience homelessness tend to use emergency medical services at a higher rate than those who are housed, but their records indicate they require specialized referrals and have higher risk of post-operative complications. In the video that follows, Dr. Naomi Thulien speaks about the benefit of hospitals offering centralized access to specialized services for these patients with complex medical and social needs.
Dr. Naomi Thulien: Do people who experience homelessness use emergency medical services at a high rate?
In this video, Dr. Naomi Thulien argues that people who experience homelessness do use emergency medical services at a higher rate, but it is in part because they offer centralized services. She notes that relationship building is a particularly important part of health care for this population and that this has been challenging during COVID-19. Dr. Thulien concludes that there is no one-size-fits-all approach for health care but that people who experience homelessness benefit from socially inclusive services. This video is 4:06 in length and has closed captions available in English.
Key Takeaways – Dr. Naomi Thulien: Do people who experience homelessness use emergency medical services at a high rate?
- People who experience homelessness use emergency services at high rates, but it is in part because it centralizes the care services they need in one location and they do not have to wait to be seen by specialists, or to have tests done.
- Relationships are important in health care provision for people experiencing homelessness.
- Virtual health care has provided an alternative to in-person care during the COVID-19 pandemic, but it is challenging unless a relationship already exists between patient and practitioner.
- In the homelessness sector there is no one-size-fits-all approach for health care but having a connection with the health care provider is important to promote a sense of social inclusion.
The notion that there is no-size-fits-all approach for supporting people experiencing homelessness is a common theme that runs through this book. We have seen that some people who experience homelessness use emergency medical services at a high rate, while others do not use it at all.
What do you think?
Can we predict which individuals experiencing homelessness will be high users of emergency medical services based on shared characteristics? Are there factors that you think might lead some people to use emergency departments more than others?
Gabet, Grenier, Cao, and Fleury (2019) set out to answer this question by recruiting 270 individuals from shelters, temporary housing, and permanent housing in Montreal. They interviewed participants at baseline (i.e. entry into the study), and again 12 months later to see whether there were commonalities between those who used emergency departments during that time and those who did not. They found that having a substance use disorder and low perceived physical health were both need-factors that related to higher emergency department use. Interestingly, emergency department use was not associated with the different types of housing (Gabet et al., 2019).
In another study, researchers in Vancouver sought to identify factors associated with hospitalization for people experiencing homelessness or housing vulnerability (Gadermann et al., 2020). They found that hospitalization was predicted by being female and/or transgender, the level of perceived social support, self-reported mental health, and having three or more chronic health conditions, whereas having a higher education was associated with lower rates of hospitalization (Gadermann et al., 2020).
What do you think?
 In the study conducted by Gabet et al., (2019) researchers did not find a connection between housing type and hospitalization rates. However, the study conducted by Gadermann et al., (2020) showed that residential moves are associated with higher risk of hospitalization. Why do you think the type of housing may be less important than the number of places a person has lived, as a risk factor for subsequent hospital usage? What might the risk associated with residential instability tell us about having secure housing as a key social determinant of health?
In the study conducted by Gabet et al., (2019) researchers did not find a connection between housing type and hospitalization rates. However, the study conducted by Gadermann et al., (2020) showed that residential moves are associated with higher risk of hospitalization. Why do you think the type of housing may be less important than the number of places a person has lived, as a risk factor for subsequent hospital usage? What might the risk associated with residential instability tell us about having secure housing as a key social determinant of health?
We encourage you to consider these questions as you watch the next video of Dr. Naomi Nichols, who is a Tier II Canada Research Chair in Community-Partnered Social Justice Research at Trent University. She reflects upon youth and how – while we may often say homelessness leads to poor health – we must also recognize the ways constantly having to work to obtain health care can be destabilizing to one’s housing. Here, Dr. Nichols explains further.
Dr. Naomi Nichols: The impact of uncoordinated medical services on youth
In this video, Dr. Naomi Nichols reflects on research her team has conducted in Quebec, on how public sector institutions operate in relation to youth homelessness. She notes that in many ways these institutions are not preventing homelessness, but actively contributing to young people’s housing instability. She argues that the health care system is one example, where young people do relentless and unremitting work seeking access to care, which can have a destabilizing effect on their lives. While we often hear that homelessness leads to poor health, Dr. Nichols argues that it is more complex in that a lack of access to timely and sufficient health care can also be a driver of homelessness. In the absence of this care, young people may turn to emergency rooms, where even despite multiple visits they receive only treatment but not ongoing coordination of care. This video is 3:24 in length and has closed captions available in English.
Key Takeaways – Dr. Naomi Nichols: The impact of uncoordinated medical services on youth
- In many ways, public sector institutions are not only preventing young people from becoming homeless, but actively contributing to their housing instability.
- The health care system is one example where our interventions undermine the health and housing of people experiencing homelessness.
- Research in Quebec indicates young people do relentless and unremitting work to seek access to mental health care and/or addictions treatments and are often unsuccessful for years.
- After young people are diagnosed, the treatments often are destabilizing in their lives, resulting in insecure housing.
- We often talk about homelessness causing poor health, but it is more complicated than that. A lack of access to timely and sufficient health care can be a driver of homelessness.
- Timely access to quality health care can be particularly challenging for young people, who may not have advocates to help them navigate the health care system.
- Canada does not have enough mental health services that are publicly funded and sufficient for the number of mental health issues that people are experiencing.
- In the absence of adequate primary and mental health care, people are relying on emergency rooms. There is a fundamental lack of capacity to address anything beyond keeping people alive.
- A young person who returns to the emergency room multiple times, such as overdose or suicide attempts, receives immediate care but no long-term coordination or support.
Researchers leading the “At-Risk Youth Study” in Vancouver also examined hospitalization and homelessness with a focus on the experiences of young people (Chang et al., 2018). They found that of the 1,216 study participants, 31% reported having been hospitalized within 6 months prior to being surveyed and that the reasons were primarily for mental illness, physical trauma, and drug-related issues (Chang et al., 2018). This study again shows that not every person who experiences homelessness uses hospital services at a high rate but that when people do, it is for legitimate medical reasons that often have been left untreated to the point where they have reached a crisis level situation.
We have seen throughout the chapter on Primary Care & Nursing that people who experience homelessness often have chronic health conditions and that they may be faced with premature aging. Those who seek emergency medical services do not do so frivolously, but because they lack equitable access to primary care. That raises an interesting question then – if studies consistently show a large percentage of people experiencing homelessness do not go to the hospital, is it because they do not need medical care? Recall for instance our study which showed that 46% of participants had not been to the hospital in the preceding year (Gilmer & Buccieri, 2020) and the At-Risk Youth Study which showed 69% of young people had not been to the hospital in the preceding 6 months (Chang et al., 2018). Is it the case that these individuals did not require medical care?
While it is possible that some were not in need of emergency care, or had primary care they could access, it is likely that at least some of these individuals needed medical care but avoided going to the hospital. When people who experience homelessness go to the hospital, they often report perceived stigma and discrimination against them. Purkey and MacKenzie (2019) have noted that some people have positive experiences in hospitals, but that many individuals who experience homelessness, particularly if using substances, feel the health care system is designed for middle-class populations and not accountable or flexible enough to meet their needs. Mainstream health care services may not always feel welcoming and inclusive to individuals with specialized needs. In the next video Dr. Alex Abramovich speaks about the use of emergency health care amongst LGBTQ2S+ people and notes that for transgender individuals, in particular, hospital care may be used only when no alternatives exist.
Dr. Alex Abramovich: Do people who experience homelessness use emergency medical services at a high rate?
In this video, Dr. Alex Abramovich discusses the complexity of emergency health care use amongst LGBTQ2S+ individuals. He notes that many people within this population have had negative encounters in health care settings and lack access to comfortable, safe, and affirming primary care. Research on LGBTQ2S+ health care can be challenging, as administrative health data generally records sex using binary categories. Dr. Abramovich notes that in research he is leading, the analysis of speciality clinic administrative data identified 2,000 transgender individuals. Although not focused on homelessness, this study did show alarmingly high rates of emergency department use amongst this group, for mental health and suicidality. Dr. Abramovich argues that many people within the LGBTQ2S+ population will avoid health care settings and seek hospital care only when a crisis arises. This video is 3:21 in length and has closed captions available in English.
Key Takeaways – Dr. Alex Abramovich: Do people who experience homelessness use emergency medical services at a high rate?
- LGBTQ2S+ people who are experiencing homelessness may not have access to primary health care in a place that is comfortable, safe, and affirming.
- LGBTQ2S+ individuals often avoid health care settings because of previous negative treatment and the impact it has on their mental health.
- LGBTQ2S+ individuals may go to the emergency room only when their health has become a crisis.
- Research on LGBTQ2S+ health care can be challenging because administrative health data does not often record sex in non-binary ways.
- A recent study that used administrative records from speciality clinics in Ontario identified 2000 transgender individuals. Although not focused on homelessness, researchers found the rates of emergency department visits for mental health and suicidality amongst this population to be alarmingly high.
For populations who require specialized care, such as LGBTQ2S+ persons and/or individuals experiencing homelessness, accessing emergency departments may indicate a lack of primary care options that have resulted in crisis level support needs. Despite the goal of universally accessible patient-centred care, mainstream health care services can be felt as stigmatizing and shaming for patients experiencing homelessness, which may lead them to avoid or abandon seeking treatments they need (Purkey & MacKenzie, 2019).
People who have concurrent disorders – mental illness and addictions issues – use emergency departments at comparatively higher rates than those without (Zhang et al., 2018) but they may not be well served by mainstream health care services, including primary and emergency sectors. Stigmatization against these and other marginalized patients is an issue across emergency response services, which can negatively affect their quality of care (Alunni-Menichini, Bertrand, Roy, & Brousselle, 2020). Zhang et al., (2018) have suggested that comprehensive programs, such as those that integrate mental health and addiction services with primary care and community-based outreach may better address these individual’s unmet health needs and improve their health outcomes.
Emergency response outreach is an approach that brings hospital personnel and other emergency workers directly into the community to meet individuals with complex needs where they are. The two videos below demonstrate examples of emergency outreach programs, such as through the Ottawa Hospital and Vancouver paramedic bike program. People who experience homelessness have higher rates of emergency department use and are frequent users of public ambulatory health services (Gentil, Grenier, Bamvita, & Fleury, 2020). A study of people who call EMS services, such as ambulance, frequently showed that they are often experiencing structural barriers like poverty and food insecurity at higher rates than the general population average (Agarwal et al., 2019). Bringing emergency response systems to the community may increase their accessibility and also has the potential to increase the time emergency health workers spend with these individuals. Research has shown that Canadian paramedic students report generally positive attitudes about working with people experiencing homelessness, but that their interest and confidence in treating this population decreases between pre- and post- placement in the field (Cochrane et al., 2019). As you watch the videos below, we encourage you to think about how programs such as these have an important role to play in bringing emergency medical services out into the community.
Emergency response is an important part of care for people experiencing homelessness, particularly if a person’s life is at risk (Alunni-Menichini et al., 2020). As we have seen in the previous videos, outreach is one way that emergency services can connect with marginalized patients and offer them specialized supports that they may not otherwise receive. However, while these programs are critically important, they do not negate the need to fix the problems in the mainstream health care system that make it discriminatory and inaccessible for some members of the community. Outreach is good, but we must also work to make hospitals and other health care settings more welcoming and inclusive spaces for treating the specialized needs of people experiencing homelessness.
We began this section by highlighting the simplicity of the question – do people experiencing homelessness use emergency medical services at a high rate? The responses and the research are clear that indeed homelessness often is associated with higher use of emergency medical services. However, the responses do not end there. We have seen throughout, the “but” that follows this answer. Yes, people who experience homelessness use emergency medical services at higher rates, but:
- the figures vary according to different research studies,
- it is often because they lack access to primary care,
- those who do use emergency services at high rates represent only a percentage of people experiencing homelessness,
- high rates of use should not be confused with unnecessary use,
- complex health conditions require access to multiple specialists,
- access to emergency medical services may be a last resort when a person reaches crisis levels of need.
Thus, while we began with a very simple question, we ended up with a rather complicated answer. We have seen throughout this section that when people who experience homelessness do use emergency medical services they often report feeling that the services are not designed for them. They may face discrimination and stigma, particularly if they are seeking care for mental illness, substance use issues, and/or transgender care. Emergency medical outreach services, such as those profiled in Ottawa and Vancouver, offer supports that are more accessible by meeting people where they are in the community. However, as we have stated repeatedly, people who experience homelessness do not have equitable access to health care. We must ensure that all health care systems – whether primary or emergency – are accessible and inviting for all patients who walk through the door.
Podcast: Do people who experience homelessness use emergency medical services at a high rate? (16:33)
Click the link below to listen to all of the researchers answer the question “Do people who experience homelessness use emergency medical services at a high rate?” in audio format on our podcast!


