39 2.1: How Immunotherapy Fights Cancer
The Nobel prize for physiology or medicine in the year 2018 went to a remarkable pair of scientists, Tasuku Honjo and James Allison, for their discovery of inhibiting negative immune regulation using T cell targeted therapy. This represented a breakthrough in a new age of cancer therapy, one that targeted and manipulated our own immune system to enhance an anti-tumor response. How was this done? And what concepts is it based upon? This chapter will elucidate the fascinating and new field of cancer immunotherapy.
Figure 2: In 2013, cancer immunology was the topic of the highly respected Science Immunology Journal. Obtained from: https://www.immunology.org/science-cover-calling-cancer-immunotherapy-breakthrough-the-year-2013.
As you know from the previous chapter, cancer is a series of passenger mutations and driver mutations which facilitate pathological clonal expansion. Our normal immune system when we do not have cancer can seek out and kill cells which are aberrant or irregular. This was established by Frank McFarlane Burnet and it is called the immune surveillance hypothesis. Then why does cancer evade this endogenous system? The answer is that biochemical changes that occur in cancerous cells as they acquire driver mutations changes the recognition of these cells by other cells. Anti-cancer cells such as T cells, natural killer cells, and dendritic cells rely on surface markers and molecular signals to establish that a cell is cancerous. For example, downregulation of the antigen presenting molecular MHC-1 on our cells signals to natural killer cells that a cell could be cancerous. However, the process of cancer evolution by natural selection can blindly force cancer cells to survive which do not have the properties recognized by our immune system.
Tumor cells evolve to evade recognition by the immune system in a process called immunoediting. They downregulate those ligands and molecules that our anti-cancer cells recognize, and they increase the likelihood of our progenitor immune cells becoming pro-cancerous regulatory cells. This occurs by two mechanisms.
- Immune exhaustion: anti-cancer immune cells in an inflammatory environment lose effectiveness and upregulate markers which indicate exhaustion
- Immune suppression: immune cells acquire properties through differentiation and molecular signalling which contributed to tumor promotion
Therefore, there is a balancing act in cancer treatment and our body’s defense against cancer. The anti-cancer immune response needs to be promoted while the regulatory pro-cancer response needs to be repressed.
An anticancer response can be amplified by either upregulating or enhancing the effectiveness of anti-tumor ligands on immune cells or decreasing the effectiveness of negative regulatory molecules on pro-cancerous immune cells. This is called checkpoint blockade therapy, and it is the remarkable ability to negatively regulate the suppressive ligands of the immune system that won Dr. Honjo and Dr. Allison their Nobel prize.
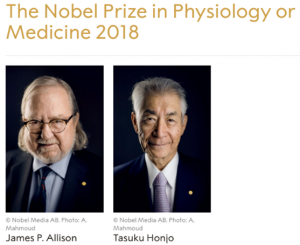
Figure 3: Winners of the 2018 Nobel Prize Professor Allison and Professor Honjo. Obtained from:https://www.nature.com/articles/d41586-018-06751-0.
But what are these molecules and how do we discover them? What tools do we have to specifically target them? What does targeting them accomplish? This will be discussed in the next chapter.
Test your knowledge:
