3 1.3 Overview of Triple Therapy
A relatively new treatment strategy for improving lung function in patients with asthma and COPD is triple therapy, which derives its name from the combination of three classes of drugs: inhaled corticosteroids (ICS), long-acting β2 agonists (LABA), and long-acting muscarinic antagonists (LAMA). The three drugs are taken through inhalers, with recent iterations of triple therapy including all three in the same inhaler for increased convenience. As mentioned previously, the use of these drugs individually and in pairs are mainstays of both asthma and COPD treatment, but interest in combining all three has developed because of their distinct but complementary modes of action.
Inhaled Corticosteroids (ICS)
Inhaled corticosteroids (ICS) have proven to be the most effective drugs for treating asthma-associated airway inflammation. As such, they are often the first choice for treatment of asthmatic symptoms. Conversely, ICS have shown poor effectiveness for the treatment of COPD.
At the cellular level, ICS reduce inflammatory cell quantities within airways, including T lymphocytes, eosinophils, dendritic cells, and mast cells. This is accomplished by suppressing the expression of several genes encoding molecules involved in inflammation that are activated in asthmatic airway epithelial cells, such as cytokines, chemokines, adhesion molecules, receptors and enzymes that promote inflammatory cell recruitment.
Corticosteroids alter gene expression by forming complexes with cytoplasmic glucocorticoid receptors (GR), which are then translocated to the nucleus. Once in the nucleus, the complex can affect transcription in several ways. It can bind directly to glucocorticoid response elements (GRE) within gene promoter regions and act as a transcription factor to activate anti-inflammatory genes or repress pro-inflammatory genes. It can also bind and interfere with histone acetyltransferases like the CREB-binding protein (CBP), which normally open up chromatin to allow access to genes for transcription. This, combined with the complex’s ability to recruit histone deacetylases such as histone deacetylase 2 (HDAC2), allows for the repression of inflammatory genes through heterochromatin formation. One of the reasons why corticosteroids do not work as well for COPD is because HDAC2 expression and activity are inhibited, negating their gene suppressive effects.
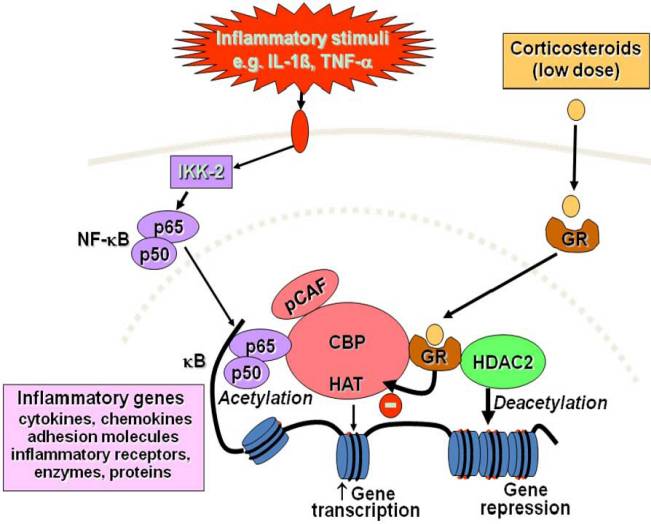
Figure 4. Diagram showing the intracellular effects of ICS. Complexes of ICS with the glucocorticoid receptor (GR) can interfere with histone acetylases such as CREB-binding protein (CBP) and recruit histone deacetylase 2 (HDAC2) to inhibit transcription of inflammatory genes (Figure from Barnes 2010).
Definitions
Histone acetyltransferases / deacetylases: enzymes that add / remove acetyl groups (O=C-CH3) from histones, respectively. DNA is wrapped around histones to form chromatin, and histone acetylation and de-acetylation modulate the accessibility of chromatin to RNA polymerase and transcription factors, which facilitate gene transcription. In general, acetylating histones opens up chromatin structure to promote gene transcription, while deacetylating histones keeps DNA inaccessible, repressing transcription.
Bronchodilators
LAMAs and LABAs are both classified as bronchodilators: medications that relax and dilate the airways. Due to their distinct and complementary modes of action, both LAMAs and LABAs are mainstays of asthma and COPD treatment, and are used to treat patients at all stages of both diseases.
Long-acting muscarinic antagonists (LAMA)
LAMAs affect the parasympathetic nervous system’s control of tone in airway smooth muscle cells, which mediates the constriction and dilation of bronchi. The primary neurotransmitter of the parasympathetic nervous system is acetylcholine (Ach), which binds to muscarinic receptors, the most relevant of which are M3 receptors, found on airway smooth muscle, airway epithelial cells, and mucous glands. The therapeutic effects of LAMAs result from their antagonistic interaction with muscarinic receptors.
In smooth muscle cells, Ach released from parasympathetic neurons binds to muscarinic receptors, causing a signal transduction cascade that results in the contraction of airway smooth muscle cells due to Ca2+ efflux from the sarcoplasmic reticulum. Ach also binds to muscarinic receptors on airway mucous glands and goblet cells, stimulating the secretion of mucus into airways. The resulting bronchoconstriction and mucus hypersecretion combine to obstruct the airways. By blocking acetylcholine’s interaction with these receptors, LAMAs alleviate the effects of COPD and asthma by promoting smooth muscle cell relaxation, bronchodilation, and reduced mucus secretion.
Definitions
muscle tone: refers to the passive contraction of muscle cells at rest. Modulating the tone of airway smooth muscle cells leads to bronchoconstriction and bronchodilation.
sarcoplasmic reticulum: an organelle similar to the endoplasmic reticulum, found in muscle cells. Its primary function is to store calcium ions (Ca2+). The release and uptake of calcium ions from the sarcoplasmic reticulum are essential for muscle contraction.
Besides neurons, Ach is also released from inflammatory and epithelial cells, where they act as autocrine or paracrine effectors to induce immune cell proliferation and chemotactic cytokine release, leading to the migration of neutrophils and eosinophils. These inflammatory effects are mediated by muscarinic receptors; thus they can be inhibited with LAMAs to treat airway inflammation and obstruction.
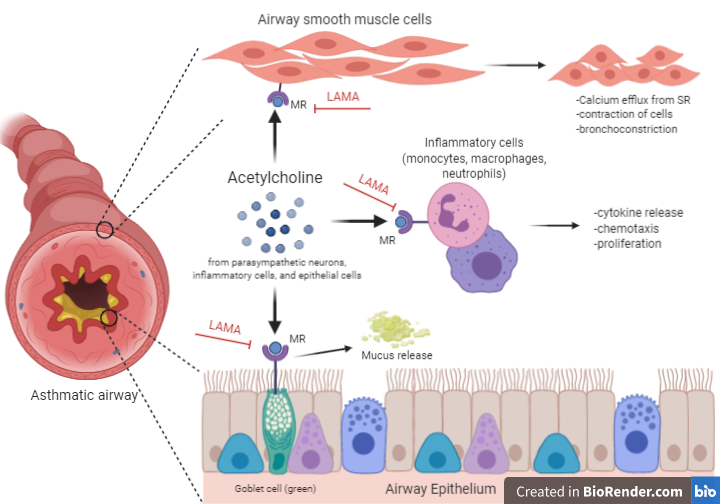
Figure 5. A summary of the various effects of acetylcholine binding to muscarinic receptors (MR), including mucous secretion from goblet cells, bronchoconstriction from airway smooth muscle cell contraction, and proliferation and chemotaxis of immune cells. LAMAs can inhibit these processes by binding to MRs and preventing acetylcholine binding (Created with BioRender.com).
Long-acting β2 agonists (LABA)
Instead of acting on the parasympathetic nervous system, the mechanism of action of LABA drugs involves the sympathetic nervous system. As their name suggests, LABAs are compounds that act as agonists for β2 adrenergic receptors found on airway smooth muscle cells.
β2 adrenergic receptors normally bind to epinephrine (adrenaline) and are coupled to G-proteins that mediate their downstream effects. It is thought that when the receptor is stimulated, the G protein’s stimulatory subunit activates cyclic AMP production through adenylate cyclase. This leads to smooth muscle relaxation both through sequestration of Ca2+ ions into the sarcoplasmic reticulum, and through the activation of protein kinase A, which modulates various proteins that regulate muscle tone. β2 agonists, therefore, stimulate bronchodilation by binding to these β2 receptors. Studies are still being performed to determine whether the effects of β2 receptor activation are mediated through the cAMP signal cascade or some other independent mechanism.
References
Inhaled Corticosteroids
Barnes, Peter J. “Inhaled Corticosteroids.” Pharmaceuticals (Basel, Switzerland), vol. 3, no. 3, Mar. 2010, pp. 514–40. PubMed, doi:10.3390/ph3030514.
Hossny, Elham, et al. “The Use of Inhaled Corticosteroids in Pediatric Asthma: Update.” World Allergy Organization Journal, vol. 9, 2016, p. 26. DOI.org (Crossref), doi:10.1186/s40413-016-0117-0.
Bronchodilators
Alagha, Khuder, et al. “Long-Acting Muscarinic Receptor Antagonists for the Treatment of Chronic Airway Diseases.” Therapeutic Advances in Chronic Disease, vol. 5, no. 2, Mar. 2014, pp. 85–98. PubMed, doi:10.1177/2040622313518227.
Kistemaker, Loes E. M., et al. “Regulation of Airway Inflammation and Remodeling by Muscarinic Receptors: Perspectives on Anticholinergic Therapy in Asthma and COPD.” Life Sciences, vol. 91, no. 21–22, Nov. 2012, pp. 1126–33. PubMed, doi:10.1016/j.lfs.2012.02.021.
Matera, M. G., et al. “Pharmacology and Therapeutics of Bronchodilators Revisited.” Pharmacological Reviews, edited by Eric L. Barker, vol. 72, no. 1, Jan. 2020, pp. 218–52. DOI.org (Crossref), doi:10.1124/pr.119.018150.
Tashkin, Donald P., and Leonardo M. Fabbri. “Long-Acting Beta-Agonists in the Management of Chronic Obstructive Pulmonary Disease: Current and Future Agents.” Respiratory Research, vol. 11, no. 1, Dec. 2010, p. 149. DOI.org (Crossref), doi:10.1186/1465-9921-11-149.
Figure 5: “Diagram showing the various effects of acetylcholine…” created using Biorender.com
