9.8 How much do I change oxygenation settings by?
Acute Respiratory Distress Syndrome (ARDS) poses the most extreme oxygenation challenge in the domain of mechanical ventilation. An extensive body of literature on oxygenation support during ventilation predominantly centers around addressing the complexities of ARDS. This critical condition demands special attention and strategic management to optimize oxygenation and improve patient outcomes. As such, the focus on ARDS in ventilation literature reflects the significance of this condition and the ongoing efforts to enhance therapeutic approaches.
Let’s first review ventilation settings that affect oxygenation, mainly FiO2 and PEEP.
Adjustments of FiO2 to Improve Oxygenation
Depending on the cause of hypoxia, it may take some time for a patient to respond to oxygen therapy. For example in hypoxemia caused by circulatory problems or anemia, supplemental oxygen may be necessary until the underlying cause is resolved.
In the realm of oxygenation assessment, a plethora of parameters exists, each influenced by the specific clinical site protocols and patient oxygenation requirements. The table below lists common parameters useful in assessing oxygenation status. However, across all practice settings, a rapid and universally embraced bedside evaluation of oxygenation status can be conducted employing the following key parameters: PaO2, SpO2 and P/F ratio (the ratio of PaO2 to FiO2).
|
Commonly Used Oxygenation Indices |
||
|---|---|---|
| Arterial partial pressure of O2 | PaO2 | [latex]\small{\text{80 - 100 mmHg}}[/latex] |
| Arterial oxygen saturation | SaO2 | [latex]\small{\text{>}92\%}[/latex] |
| PaO2/FiO2 | P/F | [latex]\small{\text{380 - 475 (when PaO}_2\text{ is normal and FiO}_2\text{ is 0.21)}}[/latex] |
| Alveolar partial pressure of oxygen | PAO2 | [latex]\small{\text{100 - 673 mmHg (when FiO}_2\text{ is 0.21 to 1.0)}}[/latex] |
| Alveolar-arterial oxygen tension gradient | P(A-a)O2 | [latex]\small{\text{5 - 10 mmHg on FiO}_2\;0.21\\\text{30 - 60 mmHg on FiO}_2\;1.0}[/latex] |
| Mixed venous partial pressure of O2 | PvO2 | [latex]\small{40\text{ mmHg}}[/latex] |
| Saturation of mixed venous O2 | SvO2 | [latex]\small{75\%}[/latex] |
Similar to adjusting ventilation parameters, arterial blood gases are initially used to determine presence and level of hypoxia, based on PaO2 and SaO2. When the patient’s cardiovascular status is relatively stable, there is a linear relationship between FiO2 and PaO2. This relationship can be used as a guideline to determine necessary FiO2 adjustment based on the following equation:
[latex]\begin{align*}\frac{\text{Known PaO}_2}{\text{Known FiO}_2}&=\frac{\text{Desired PaO}_2}{\text{Desired FiO}_2}\\&\\\text{Desired FiO}_2&=\frac{\text{Known FiO}_2\times\text{Desired PaO}_2}{\text{Known PaO}_2}\end{align*}[/latex]
This method offers a simplified approach for determining FiO2 when the patient’s condition is stable. Nonetheless, it’s essential to acknowledge that oxygenation is frequently a complex and challenging process often requiring multiple adjustments, typically in increments of [latex]10\%\text{ - }20\%[/latex], to achieve the desired outcome. Additionally, identifying the root cause of hypoxia is crucial in effectively managing oxygenation issues.
The harmful effects of prolonged FiO2 levels exceeding [latex]0.60[/latex] are widely recognized, as they can lead to oxygen toxicity. Therefore, whenever a patient’s oxygen requirements surpass this threshold, or even as a preventive measure, it is crucial to consider adjusting Positive End-Expiratory Pressure (PEEP). By exploring PEEP adjustments, we can effectively manage and optimize oxygenation while minimizing the risk of oxygen-related complications.
Adjustment of PEEP to Improve Oxygenation – Optimal PEEP
Optimal PEEP is defined as the level at which the majority of alveoli remain inflated at the end of expiration. This critical point represents the PEEP setting that provides the maximum beneficial effects, including increased Functional Residual Capacity (FRC), enhanced alveolar recruitment, and optimal static compliance. At this specific PEEP level, the respiratory system achieves its best performance and efficiency ensuring improved lung function and oxygenation.
A number of different methods are currently used in practice, depending on the clinical site protocol and resources, you may encounter all or some of the following during your clinical placement:
- Incremental or Decremental PEEP studies
- Esophageal pressure monitoring
- Pressure Volume Curves
- PEEP – FiO2 tables
Regardless of the method used, setting optimal PEEP is often challenging and it should be set based on individual patient lung condition and disease process.
Incremental or Decremental PEEP Studies
During a PEEP study, it is essential to exercise caution as the end-expiratory pressure is incrementally increased. Diligent monitoring of the patient’s hemodynamic status becomes imperative to prevent potential cardiovascular compromise that may arise from elevated pressures in the lungs. At a minimum, continuous monitoring of the patient’s blood pressure is warranted, as a PEEP study may lead to a reduction in cardiac output with subsequent drop in blood pressure.
In addition to careful attention to hemodynamics, comprehensive monitoring of the patient’s ventilatory status is equally important. Monitoring parameters such as peak inspiratory pressure, plateau pressure, tidal volume, and arterial blood gases allows for a thorough assessment of the patient’s response to the PEEP study. Other oxygenation and cardiovascular indices can be monitored, when resources are available.
To perform an incremental PEEP study, PEEP is increased in [latex]2\text{ cmH}_2\text{O}[/latex] increments every 15 minutes, while estimating static compliance and monitoring selected ventilation and hemodynamic parameters to assess the adequacy of oxygenation and the function of the cardiovascular system.
To perform a decremental PEEP study, as the name suggests, we start with a higher PEEP obtained with a lung recruitment maneuver. From there, PEEP is reduced to [latex]25\text{ cmH}_2\text{O}[/latex] and then decreased in increments of [latex]2\text{ cmH}_2\text{O}[/latex].
A decrease in compliance or oxygen saturation at a certain level of PEEP implies decruitment and that PEEP should be increased to the previous level.
Esophageal Pressure Monitoring to set Optimal PEEP
Esophageal manometry allows measurement of esophageal pressure which indirectly reflects pleural pressure. You will remember from previous chapters that the pressure responsible for alveolar inflation is the transpulmonary pressure [latex](P_{alv}-P_{pl})[/latex]. The most common way to measure Pes is using an air‑filled balloon integrated into an esophageal catheter that is placed in the esophagus. Knowing pleural pressure, we can set PEEP accordingly to achieve a transpulmonary pressure of zero. Watch this video for a demonstration of using transpulmonary pressure to set optimal PEEP.
Pressure Volume Curves (Loops) to set Optimal PEEP
Ventilators equipped with this feature perform a respiratory mechanics maneuver by delivering a quasi-static PV (pressure/volume) curve at a low flow rate, typically less than [latex]6\text{ Lpm}[/latex]. As we previously learned, the components of a PV curve can help us improve ventilation. It allows for determination of the lower and upper inflection points. When this method is employed, PEEP is set [latex]2\text{ cmH}_2\text{O}[/latex] above the lower inflection point. Many clinicians recommend that PEEP be set on the exhalation limb of the PV loop, as more volume is present in the alveoli during exhalation for a certain pressure compared to the inspiratory limb. What stays open during exhalation will be easier to inflate during the next inhalation, requiring less driving pressure. Research is continuously being done to determine best practices on setting optimal PEEP.
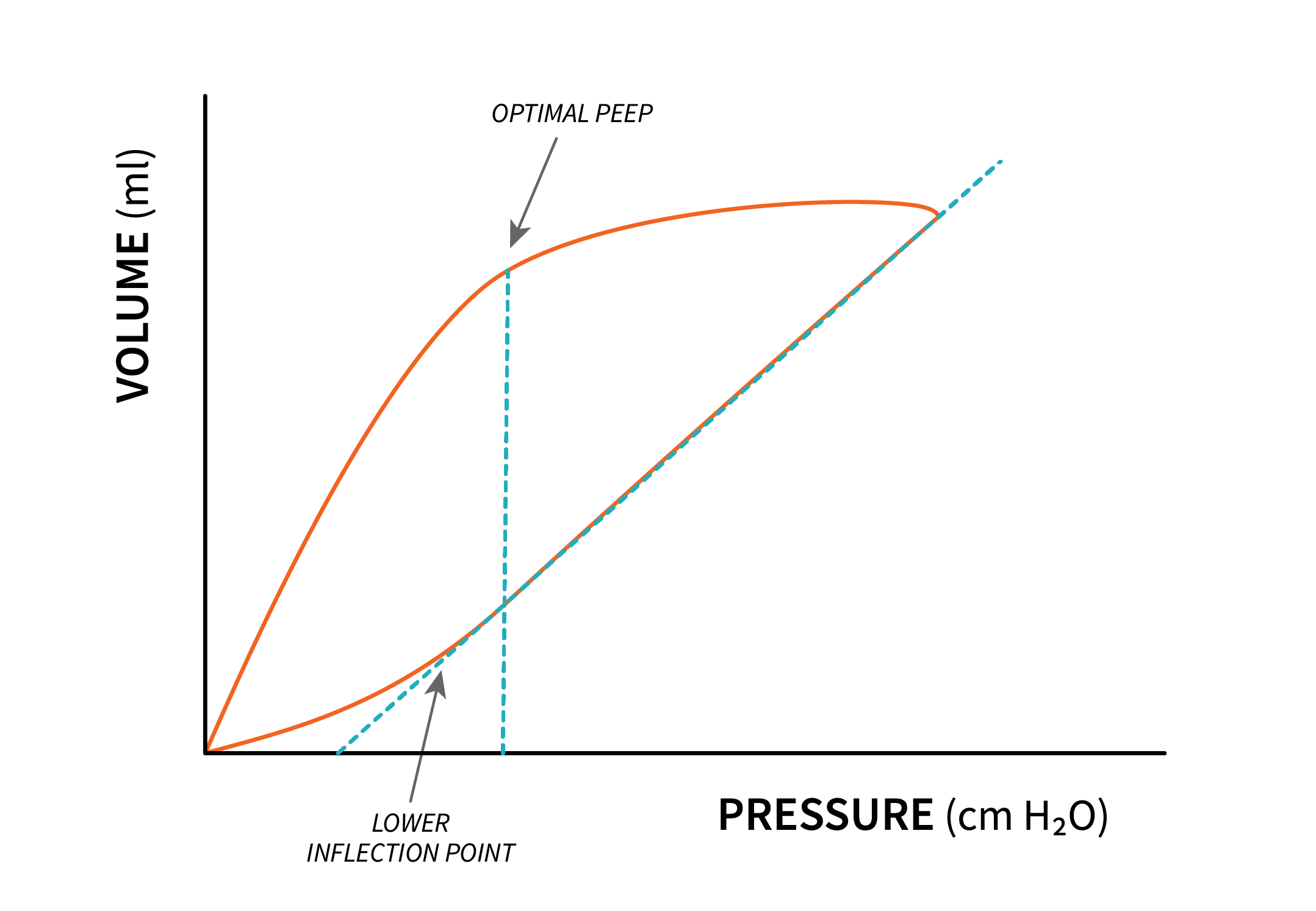
The shape of PV loops can also be used to determine if lungs are recruitable. For a lung to be deemed recruitable, presence of hysteresis and gain in volume is required. A large hysteresis indicates potential for recruitment, while a small or absence of hysteresis indicates the lung is not recruitable.
A lung recruitment maneuver (LRM) is another tool to improve oxygenation, and it involves an increase in pressure in the lung for a longer period of time than a normal respiratory cycle. Common approaches to LRM is [latex]30\text{ cmH}_2\text{O}[/latex] for [latex]30\text{ seconds}[/latex] or [latex]40\text{ cmH}_2\text{O}[/latex] for [latex]40\text{ seconds}[/latex]. Due to the risk of increasing intrathoracic levels, careful monitoring of patients during this procedure is required, and the maneuver should be aborted at the first sign of cardiovascular compromise.
Electrical impedance tomography (EIT) is available to titrate PEEP to achieve the greatest volume in the lung (seen as greatest area of air in the lung with EIT), however, this method may not be available in all institutions.
Finding Optimal PEEP Article
This article provides a concise summary of the history of research on finding optimal PEEP and the need for further research.
In search of the Holy Grail: identifying the best PEEP in ventilated patients

