5.5 Volume Control Ventilation
We have overviewed the two branches of control ventilation: pressure and volume. Now lets dive into the two types of control modes a little deeper. Volume Control (ACVC, VCV, CMV-VC) is usually a more straightforward and easy-to-understand mode for anyone new to the world of mechanical ventilation. The clinician sets how big (tidal volume) a breath and how often the breath is delivered. As the name suggests, the volume of breath delivered is exactly the same every single time; it is constant and does not vary. The ventilator will deliver whatever pressure is needed to achieve the tidal volume in the set time that each breath must be delivered in. Volume is the control variable here. Once the set volume is delivered, the ventilator will either cycle into exhalation, or hold an inspiratory pause, as set by the clinician. In the later case, the ventilator will time cycle into exhalation at the end of the inspiratory pause (inspiratory hold).
We learned that flow is an expression of volume over time. Flow remains constant until the volume is delivered. Thus the flow curve does not change if the volume is the controlled variable, and there is a set respiratory cycle time. Usually, in volume control the set time is controlled by a flowrate, but some ventilators will let you set an inspiratory time instead.
The clinician sets on the ventilator the amount of air to be pushed into the lungs and the number of times the lungs will inflate per minute (tidal volume and respiratory rate). Also set is the max flow rate of the air being delivered—think of it as the “speed” of the air being pushed into the lungs. With constant volume, the Inspiratory time will change as a byproduct of the max flow rate you set on the ventilator. The higher the flow rate, the shorter the inspiratory time of the breath to deliver the set volume.
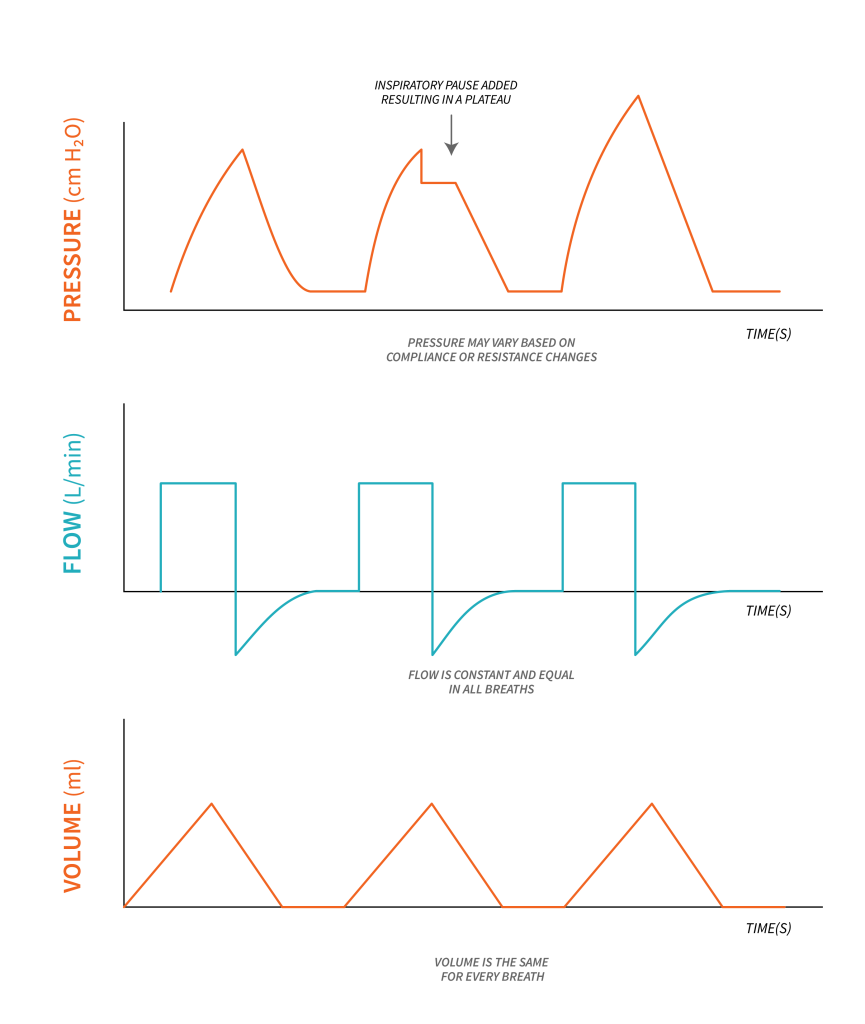
One parameter that you do not set in volume control is pressure—specifically peak pressures or distending pressures (pressure control or inspiratory pressure). Remember that ventilators deal with the application of positive pressure to fragile alveoli in the lungs. If not done carefully, the alveoli will act like any balloon. Balloons, if overinflated, will pop. Alveoli, if inflated too much, will become overdistended and can be irrevocably damaged. Have a look at the graphic above, pressure increased on the third breath due to a change in either compliance or resistance in order to deliver the set tidal volume.
Also take note on the above graphic that an inspiratory pause (inspiratory hold) can be added to the inspiratory time, resulting in a plateau on the pressure-time waveform. During this inspiratory pause, plateau pressure can be measured.
So how do you limit the pressure being experienced in the lungs when you are in volume control mode? You cannot directly set it—you set the volume instead. Pressure is monitored as a direct relationship based on the volumes and flows set. This means that you need to watch the pressure the ventilator is needing to inflate the lungs at the set volume and time you are asking it to achieve. If the pressure you are seeing in the lungs is too high, you may need to decrease the volume you are targeting or slow down the flowrate (increase the inspiratory time) to decrease the pressures experienced by the lungs.
Key Takeaways
- Pressure and volume have a linear relationship. If you decrease the volume, you are inflating the lungs too. This will decrease the pressure.
- Taking longer to inflate the lungs will allow you to “blow softer” or a lower pressure to achieve the same volume. Slowing the flow rate down or increasing the Inspiratory time will help with this.
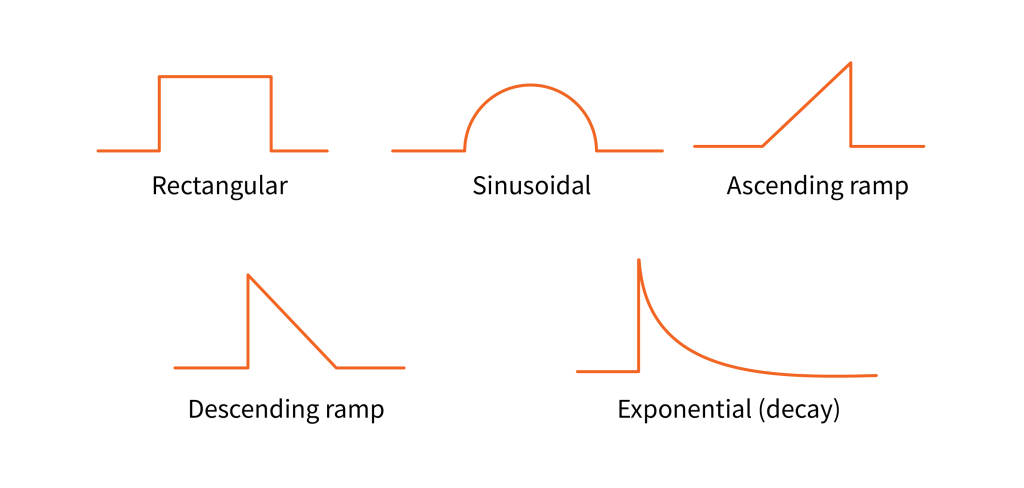
While in volume control ventilation, the flow available to the patient is limited, a ventilator can use different patterns to deliver the flow of air. Other than constant waveform (rectangular waveform), you may see the following patterns:
Test Your Knowledge
Consider volume control ventilation and what are the breath variables for this ventilation mode: Trigger, limit, cycle and baseline.
|
Summary of Basic Settings in A/C – VCV |
|
|---|---|
In A/C volume control, you will directly set:
|
In A/C volume control you will observe but not directly set:
|
Lung Compliance and Resistance
We have now reviewed and reinforced the relationship of volume and pressure, and we have also discussed that in volume control the achieved volume will always be delivered by the ventilator with whatever pressure is needed. The volume is constant unless the clinician decides to change it based on what they are noting in terms of the patient’s condition. But what if the lungs themselves start to change? We know that many illnesses and pathologies can change the status of the lungs: they can make the lungs stiffer (less compliant) or restrict the air’s ability to flow through the airways (increased resistance).
Let’s explore lung compliance and resistance a little further and how these factors impact volume control ventilation.
Lung compliance is a measurement of how easily the lungs can expand and stretch. More compliance would refer to lungs that stretch much easier than lungs with lower compliance. If lungs are less compliant, they will be harder to inflate and they will need higher pressures to overcome the rigidity of the lungs. Think about blowing up a regular balloon versus a tire. Both inflate and expand, but a tire is much more stiff and less compliant than a regular balloon so air must be delivered at high pressures, such as by an air compressor. In the same way, any lung condition that affects the stretch of the lungs will cause a lowering of compliance, and higher pressures will be needed to inflate the lungs.
Lung resistance refers to obstructions along the pathway that air will take into the lungs. Air flows through the ventilator circuit, through the endotracheal tube into the trachea, bronchus, bronchioles and then to the alveoli. The amount of force needed to start to move air through these tubes is termed resistance. Think about blowing into a straw vs. a paper towel roll. You need to blow harder to get air passing through the straw compared to the paper towel roll because it is more narrow. The narrower the tube, the higher the resistance to air movement. Any narrowing of the airways will cause a resistance to airflow, and the air will not be able to enter the lungs as easily. A good analogy for lung resistance is lane closures on a highway. Not as may cars get through and it will slow traffic down. Lung resistance will decrease the amount of air entering the lungs for every breath and will require a higher pressure as well.
As you can see, both of these factors—lung compliance and lung resistance—impact the pressures needed to deliver the set volume in volume control.
Object Lesson

Imagine blowing up two very different balloons with the exact same volume over the same amount of time. Balloon 1 is a regular birthday balloon that has been blown up many times, but Balloon 2 is a long skinny “balloon animal” balloon that has never been blown up before. Obviously, the stiffer and longer Balloon 2 will be harder to inflate and it will definitely need a higher pressure to achieve the set volume, than Balloon 2, which is looser and inflates more easily.
The same can be said for ventilating lungs. If you deliver an equal volume of air at the same flow to normal or “healthy” lungs versus damaged or “stiff” lungs, the pressures required to inflate those lungs would be different. Stiffer lungs would require a higher pressure to achieve the same volume.
We have spent a large amount of time highlighting the relationship between pressure and volume—specifically how the pressures will increase as the volume is increased. This correlation is noticed when the clinician is making changes to the settings. In contrast, the changes noted due to compliance and resistance happen without any changes being made on the ventilator. Instead, these changes occur breath-to-breath over time as the lung condition changes. For example, if a patient has asthma, the resistance of their lungs increases as their airways constrict, or tighten, during an asthma attack. Air can’t get into the lungs as easily.
Remember, in volume control, the ventilator will adjust the pressure needed to reach the volume that is set. When the resistance increases, or if compliance drops, in volume control ventilation, this will cause an increase in the peak pressures to overcome the changes in the lungs and deliver the set volume. With this in mind, when ventilating in volume control, the pressures required by the ventilator to deliver the set volume can give you information about the status of the lungs. In a way, monitoring the pressures over time can give you another vital sign to monitor and can sometimes give you direct information on if the lungs are improving or getting worse. This information may help direct care or prompt the need for medical treatment, depending on the lung pathology, to help improve the compliance and resistance.
Let’s review the pulmonary pressures and their definitions to better understand the impact of changes in compliance and resistance on volume control ventilation.
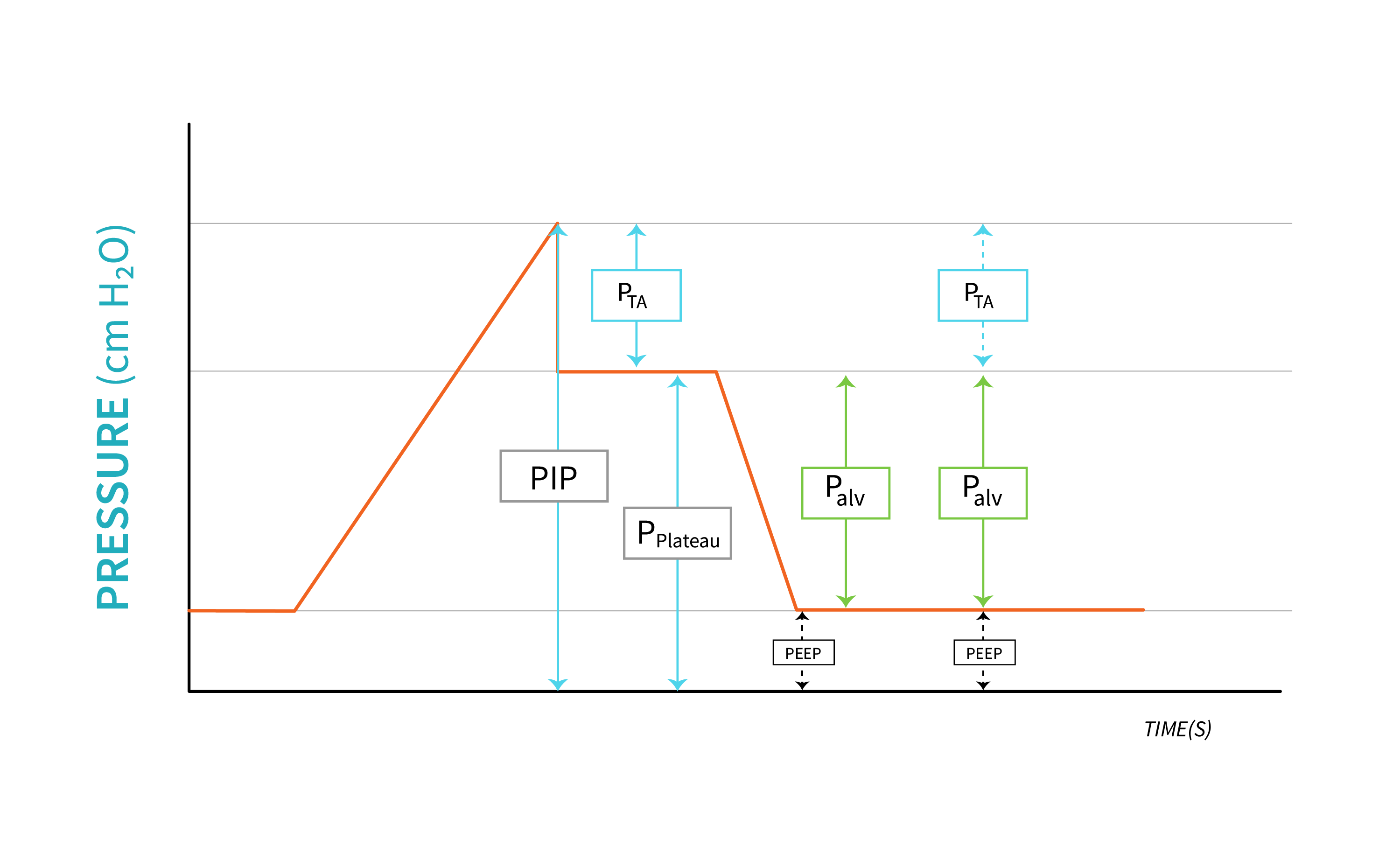
Remember from Chapter 1 that a change in lung compliance will be reflected on the alveolar pressure [latex](P_{alv})[/latex], which in term will affect plateau pressure [latex](P_{plat})[/latex]. Plateau pressure is often measured and monitored during volume control ventilation to identify changes in compliance. A change in airway resistance will be reflected on the transairway pressure [latex](P_{TA})[/latex].
Key Takeaway
To visualize the impact of changes in compliance and resistance on pulmonary pressures and implicitly on volume control ventilation, observe the Pressure-Time waveform above, and note that we can express peak inspiratory pressure, mathematically as:
[latex]\text{PIP}=\text{PEEP}+P_{alv}+P_{TA}[/latex]
We can also rewrite this equation as:
[latex]\text{PIP}=\text{PEEP}+\left(\frac{V_T}{C_s}\right)+(\dot V \times R)[/latex]
An increase in any one of the pulmonary pressures will cause an increase in peak pressure, which is what the ventilator will recognize and alert the clinician with an alarm. It is then the clinician’s responsibility to identify which component of the total pressure caused it to increase.
Example
A decrease in compliance will cause plateau pressure to increase. This, in turn, will cause the peak pressure to increase in order to deliver the same volume. The ventilator will alarm High Pressure to alert the clinician who will identify the increased plateau pressure by performing an inspiratory pause.
To conclude, in volume control, the volume delivered is constant, but there will be changes in peak pressures ([latex]\text{PIP}[/latex] or [latex]P_{peak}[/latex], which refers to the highest pressure experienced by the alveoli during a breath) to achieve the set volume for both the following situations:
- the clinician changing the set parameters (volume, flow/time).
- breath-to-breath changes based on the compliance and resistance of the lungs.
Impacts to peak pressures should be considered by the clinician when making changes, and lung pathology should be considered if changes are noted in the pressure when no adjustments to settings are made. Peak pressures should not be allowed to go too high. Remember that high pressures can cause damage to the alveoli of the lungs. Ideally, pressures should be kept below [latex]30\text{ cmH}_2\text{O}[/latex], with a maximum of [latex]35\text{ cmH}_2\text{O}[/latex], to ensure the alveoli do not get damaged. We will discuss this concept further in Chapter 5 when we discuss Volume Control settings.
Key Takeaway
Any time you connect a patient to a ventilator, you always set FiO2 and PEEP. In A/C (control mode) volume control, in addition to these settings, you must decide how often the patient is breathing as you are taking over control of the breath initiation. Therefore, the Respiratory Rate (RR) must be set. In A/C volume control, you set the volume of air delivered with every single breath. This amount is always the same and will not change unless you, the clinician, change it. Pressure is not set: it is an outcome based on the volume and flow/time of the breath and the state of the lungs you are ventilating. Target plateau pressure lower than [latex]30\text{ cmH}_2\text{O}[/latex] with peak pressure of [latex]35\text{ cmH}_2\text{O}[/latex].
“Volume Control Ventilation” from Basic Principles of Mechanical Ventilation by Melody Bishop, © Sault College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.

