1.3 FRC, Intrinsic PEEP and Respiratory Pressures
Going back to the balloon analogy, consider the process of blowing up a balloon. At what point is the balloon the hardest to blow up?
- When it is completely empty? or
- When there is a little air in it already?
An empty balloon requires very powerful and sustained breath to start inflating; but if there is a little air in the balloon already, you can blow it up with a gentler breath and you wouldn’t have to push so hard.
The lungs are no different. The initial little bit of air in the lungs requires a higher amount of pressure in order to open up the lungs a little, while a lung with some air can inflate much more easily. This is where the human body is so smart. The body stops the lungs from fully emptying—it keeps a small amount of air in the lungs at all times. This is referred to as the functional residual capacity (FRC) of the lungs. A term for the air left in the body at the end of exhalation is the intrinsic (physiologic) Positive End-Expiratory Pressure (PEEP). PEEP is very important, as it protects the lungs from the high blowing pressures that would normally be needed to inflate them from empty—decreasing the risk of trauma. We will revisit this concept in subsequent chapters.
Key Takeaway
The lungs never fully empty. Some air remains in the alveoli at all times. This is known as FRC or intrinsic PEEP. Positive End-Expiratory Pressure (PEEP) refers to the pressure left in the lungs at the end of exhalation—also known as the residual air left in the balloon to stop it from fully collapsing.
Object Lesson
Think for a moment about a balloon that you have reused for three different parties. The first time you blew it up, the rubber seemed sturdy, but over time, it became more fragile and compromised. The fourth time you tried to blow it up, the balloon popped even though it was not yet full. What happened here? The high pressure damaged the balloon over time. In the same way, your lungs can be damaged by consistent exposure to high pressure.
The main physiologic mechanism to achieve FRC is surfactant, a naturally produced lubrication that coats all the alveoli of the lungs. Surfactant stabilizes the surface of the alveoli so they do not collapse and helps facilitate the reserve of the FRC we explained earlier.
Object Lesson
Pressures in Respiratory Physiology
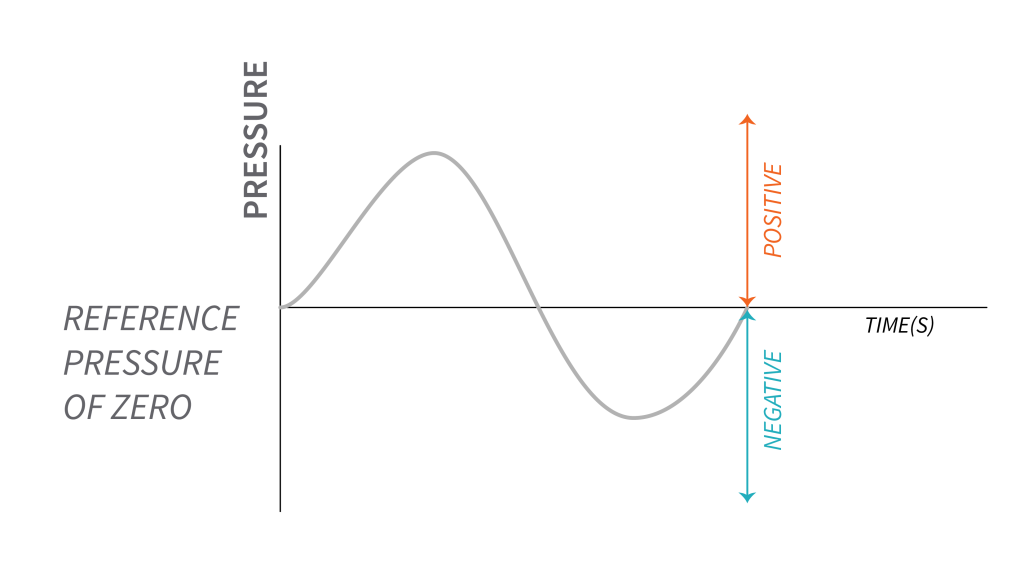
When dealing with breathing, it is important to have a good understanding of the pressure changes in the lungs during inspiration, expiration and at rest. Because pressures in the lungs are fairly low, they are usually measured in cmH2O and referenced to atmospheric pressure ([latex]P_{atm}[/latex]), which is given the value zero. Any pressure above atmospheric pressure is considered positive pressure, and any pressure below atmospheric pressure is considered negative.
As you may have already guessed, cm H2O literally refers to the weight of a centimeter (cm) of water (H2O) on a given spot. The atmospheric pressure is [latex]0\text { cmH}_2\text{O}[/latex] and any additional pressure would be above that.
Object Lesson
In this representation, the zero point represents the reference pressure. Pressure values above zero indicate positive pressure, while pressure values below zero indicate negative pressure.
Definition of Pressures and Pressure Gradients
In respiratory physiology, and inadvertently in mechanical ventilation, we will be referring to four main pressures and four important gradients. It is important to understand the impact of these pressures and gradients on respiration, so that we can apply physiology principles to mechanical ventilation, in order to safely ventilate patients.
Pressure at the airway opening, is sometimes called pressure at the mouth ([latex]P_m[/latex]) or airway pressure ([latex]P_{aw}[/latex]), or proximal pressure, when mechanical ventilation is applied. This pressure is equal to atmospheric pressure. Similarly, the pressure at the body surface ([latex]P_{bs}[/latex]) is equal to atmospheric pressure. Other pressures that are instrumental in the pressure gradients of breathing are the Palveoli (pressure in the alveoli) and the Ppleural (pressure in the pleural space). Pleural pressure ([latex]P_{pl}[/latex] or intrapleural pressure) is the pressure measured in the space between visceral and parietal pleurae. Alveolar pressure ([latex]P_{alv}[/latex]) is determined by the volume of air in the alveoli and the pressure being exerted around the alveoli—by the pleural pressure or the diaphragm. this pressure is sometime referred to as intrapulmonary pressure. This pressure depends on the elastic recoil of the lungs, specifically how compliant the lungs are. A stiff lung will require more pressure to inflate.
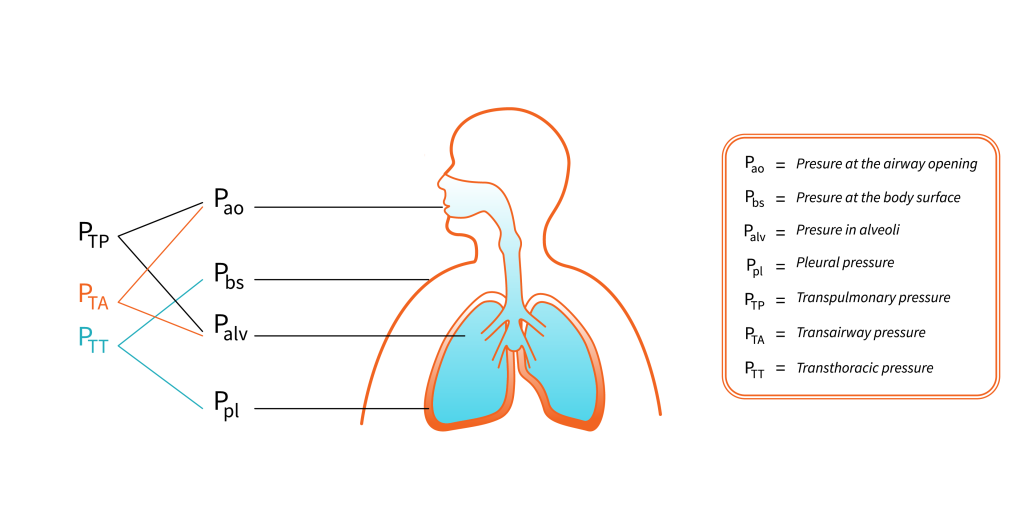
Four main pressure gradients determine different phases of the respiratory cycle, as follows:
Transairway pressure ([latex]P_{TA}[/latex]) is the pressure gradient between airway opening pressure and alveolar pressure. [latex]P_{TA}=P_{ao}-P_{alv}[/latex]. This pressure is reflective of airflow conditions, as it is the pressure required to generate flow through the airways. The gradient is always between airway opening and alveoli.
Transthoracic pressure ([latex]P_{TT}[/latex]) describes the pressure gradient required to expand and contract lungs and the chest wall in the same time. [latex]P_{TT}=P_{pl}-P_{bs}[/latex]. [latex]P_{TT}[/latex] is equal to the outward recoil force of the thorax when there is no airflow. The stronger this outward recoil force, the greater the [latex]P_{TT}[/latex].
Transpulmonary pressure ([latex]P_{TP}[/latex]) is the pressure gradient required to maintain alveolar inflation. [latex]P_{TP}=P_{alv}-P_{pl}[/latex]. In mechanical ventilation this gradient is often referred to as distending pressure.
Transrespiratory pressure ([latex]P_{TR}[/latex]) is the pressure gradient across the entire respiratory system, including airway opening, lungs, and chest wall. The components of this gradient are the respective gradients for airway, lungs and chest wall: the airway is represented by the transairway pressure ([latex]P_{TA}[/latex]), lungs are represented by the transpulmonary pressure ([latex]P_{TP}[/latex]) and chest wall is represented by transthoracic pressure ([latex]P_{TT}[/latex]).
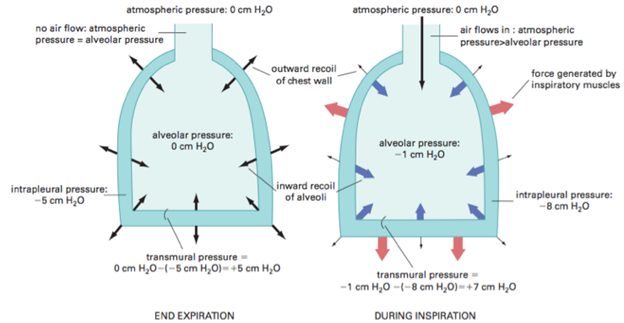
Now, let’s revisit inspiration and expiration from a pressure differential viewpoint. Remember, the lungs are glued to the diaphragm and the surrounding thorax by the pleural space. Think of this space as a large suction that is all around the lung. Just like the word suction hints at, the pleural space is a negative pressure at rest. Before inspiration occurs, the pleural space negative pressure [latex](-5\text { cmH}_2\text{O})[/latex] keeps a small amount of air in the lungs (equal to [latex]+5\text { cmH}_2\text{O}[/latex]) that cancels out the negative pressure in the lungs. This equalization stops the flow of air in or out and puts the lungs in a “rest state” until the diaphragm contracts and causes a negative pressure.
Key Takeaway
Since the pleural space has a negative pressure, to equal zero, air must be left in the lungs!
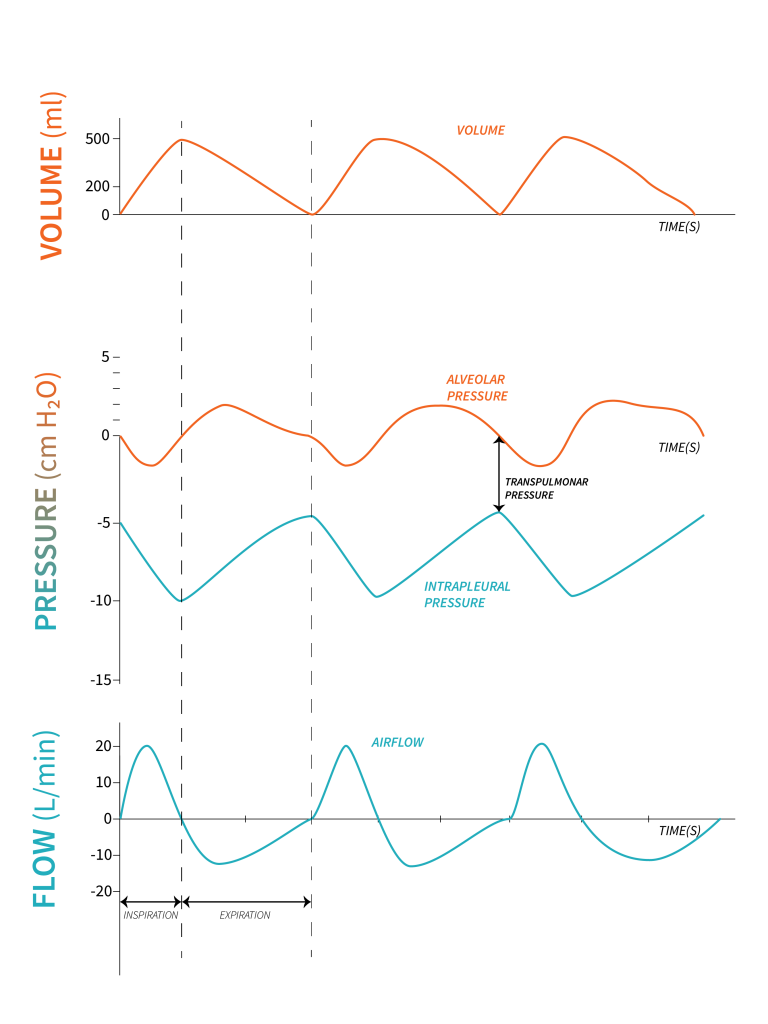
As the diaphragm contracts, the volume of the thoracic space increases and pressure in the pleural space decreases (it becomes more negative in relation to atmospheric pressure). The pressure in the pleural space drops from about [latex]-5\text { cmH}_2\text{O}[/latex] to about [latex]-10\text { cmH}_2\text{O}[/latex] at end inspiration. The negative pressure in the pleural space is transmitted to the alveoli, so alveolar pressure ([latex]P_{alv}[/latex]) becomes negative. Pressure at the airway opening is still atmospheric [latex](P_{ao}= 0)[/latex] while [latex]P_{alv}[/latex] is negative. Air flows from a point of high pressure to a point of low pressure. The gradient is always between [latex]P_{ao}[/latex] (pressure at the airway opening or atmospheric pressure) and [latex]P_{alv}[/latex]. This negative pressure gradient created from the contraction of the diaphragm, allows air to flow from airway opening into the lungs. Transpulmonary pressure ([latex]P_{TP}[/latex]) gradient widens, allowing lung inflation. Transairway pressure gradient ([latex]P_{TA}[/latex]) is about [latex]-5\text { cmH}_2\text{O}\;(0-[-5])[/latex]. As volume of air builds up in the alveoli, alveolar pressure return to zero. Airflow stops at end inspiration, because there is no longer a pressure gradient present [latex](P_{alv}=P_{ao})[/latex].
During expiration, respiratory muscles relaxation and elastic recoil of the lung tissue, results in a decrease in thoracic space and lung volume. Pleural pressure ([latex]P_{pl}[/latex]) returns to about [latex]-5\text { cmH}_2\text{O}[/latex]. As soon as the diaphragm relaxes, and stops the suction, the volume of air and therefore pressure in the chest is now higher than the pressure at the mouth. This state reverses that pressure gradient and air flows out of the lungs—in other words, exhalation occurs—until the pressures equilibrate.
Let’s review the process of inspiration and expiration again, this time using graphics. Becoming familiar with visual depictions of respiratory patterns is highly recommended, as graphics serve as valuable aids and tools in mechanical ventilation when it comes to recognizing issues and enhancing patient prognosis.
“FRC and Intrinsic PEEP” from Basic Principles of Mechanical Ventilation by Melody Bishop, © Sault College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.


