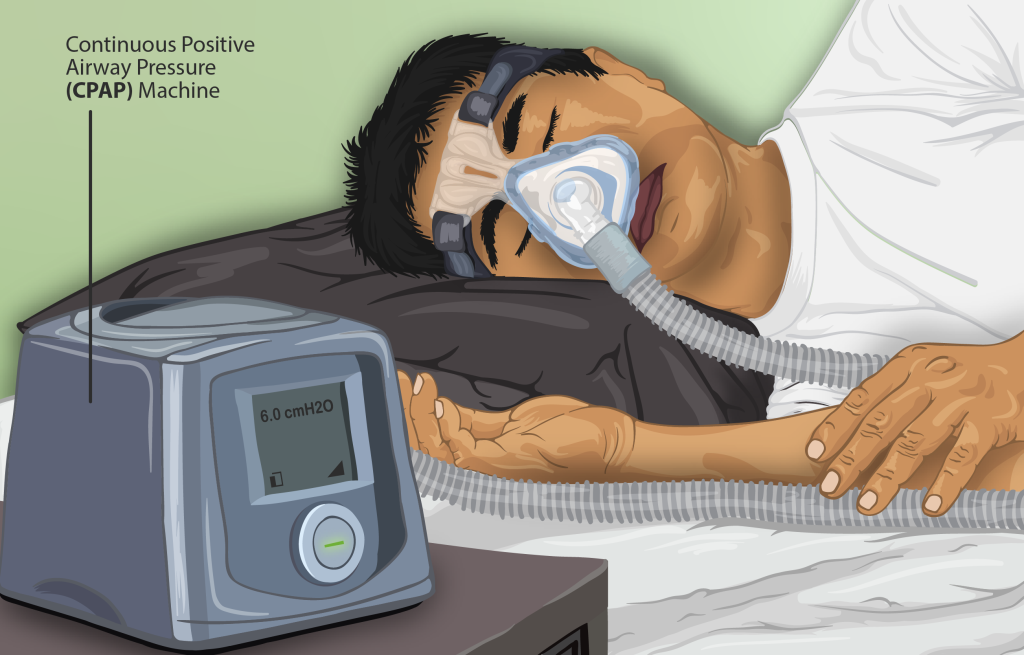
4.3 Continuous Positive Airway Pressure (CPAP)
Continuous Positive Airway Pressure (CPAP)—the name says it all. This mode applies one constant (or continuous) pressure that is maintained during both inspiration and expiration.
The main purpose of CPAP is to:
- Stents airway open. This would include
- May help offset autoPEEP
- Recruits alveoli, increases FRC
- Improves gas exchange
- Improved oxygenation and decreases FiO2
While CPAP/PEEP does not have a direct effect on ventilation and CO2 clearance, it can indirectly help, through various mechanisms, such as:
- Reduced atelectasis improving alveolar compliance and surface area for gas exchange increasing tidal volume and CO2 clearance
- Stent open upper airways in patients with obstructive sleep apnea or tracheomalacia increasing ventilation
- Counterbalance dynamic hyperinflation (auto PEEP) in patients with COPD exacerbations increasing effective tidal volume
Key Takeaway
CPAP vs. PEEP vs. EPAP vs. IPAP. What’s the difference?
Before moving forward it is important to review the terminology used in non invasive ventilation.
CPAP is the application of a continuous level of positive pressure during the entire respiratory cycle when the patient’s drive to breathe is intact (spontaneous breathing). CPAP does not provide inspiratory assistance, and therefore, is not considered a type of mechanical ventilation.
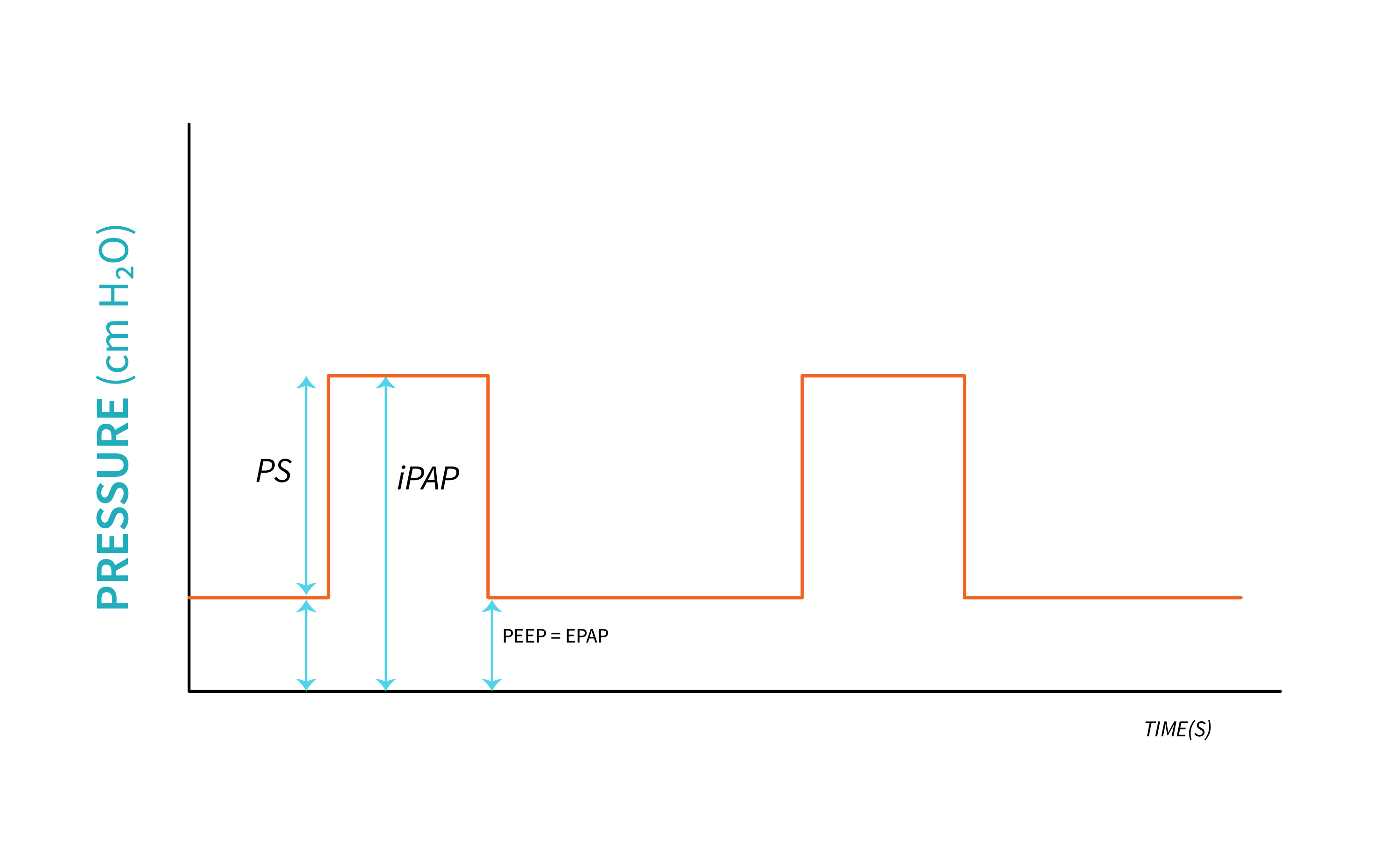
PEEP is the pressure delivered by the ventilator during exhalation. EPAP is equivalent to PEEP, and it is the baseline pressure that every breath starts and ends at.
IPAP is the pressure delivered by the ventilator during inspiration.
The difference between IPAP and EPAP is the Pressure support (PS) provided by the ventilator. This gradient is equivalent with driving pressure provided by the ventilator during controlled or assisted ventilation.
When thinking of a mask interface and pressure delivered, most people will think about CPAP and CPAP machines. CPAP is usually used for home patients that have obstructive sleep apnea. Though still pressure-applied, CPAP is not considered ventilation for a one main reason: Continuous Positive Airway Pressure (CPAP)—the name says it all. This mode literally applies one constant (or continuous) pressure through the circuit and mask interface to be delivered to the patient. Though CPAP is discussed in this chapter as a non-invasive therapy, it is not a method of non-invasive ventilation (NIV). Ventilation at its core refers to the clearance of carbon dioxide. As we have discussed, CO2 clearance happens during exhalation, and if you want to clear more CO2, you need to take a bigger breath in and, most importantly, out. In order to help the lungs inflate larger, a higher pressure must be applied during inspiration. Since CPAP is one constant pressure, CPAP does not change the pressure applied to help augment tidal volumes and does not contribute to the clearance of CO2.
The main benefit of CPAP stems from the patient breathing spontaneously in and out against the set pressure. Exhaling against positive pressure, produces a back pressure that increases the air left in the lungs at the end of a breath. This can help open collapsed airways or alveoli and is often referred to as a splinting effect.
Object Lesson

To explain back pressure, imagine breathing out through a thin straw. You are pushing against a resistance. You know how you feel pressure in your lungs as you are trying to blow into this narrow straw? That increased pressure is actually happening. Breathing out against a constant pressure of air, like CPAP, would cause the same thing. That increased pressure in the lungs will hold extra air in all areas of the lungs and help blow open (recruit) any areas of collapse. This is a back pressure that causes the “splinting effect.”
This splinting effect can be useful for specific lung issues. It is beneficial in recruiting collapsed alveoli. Involving more alveoli in air exchange will improve ventilation. Another benefit of this “splinting effect” is seen with patients who have symptoms of obstructive sleep apnea. CPAP stops the soft tissue of their nasopharyngeal region from collapsing and closing off. In a way, CPAP is similar to PEEP but just called something different because we are not in an invasive ventilation mode.
CPAP is periodically used for patients that need some help with recruiting or splinting open their airways, but in critical care and hospital settings, NIV or BiPAP is usually preferred because it allows the practitioner more control over oxygenation and ventilation. Therefore, we will focus on NIV instead of CPAP, as it is used to a much larger degree in critical care medicine.
Key Takeaway
“Continuous Positive Airway Pressure (CPAP)” from Basic Principles of Mechanical Ventilation by Sault College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.

