7.2 Why Do We Need Mechanical Ventilation? – Respiratory Failure Type II
Hypercapnic Respiratory Failure or Type II
Let’s review the analogy of respiratory system as a chain.
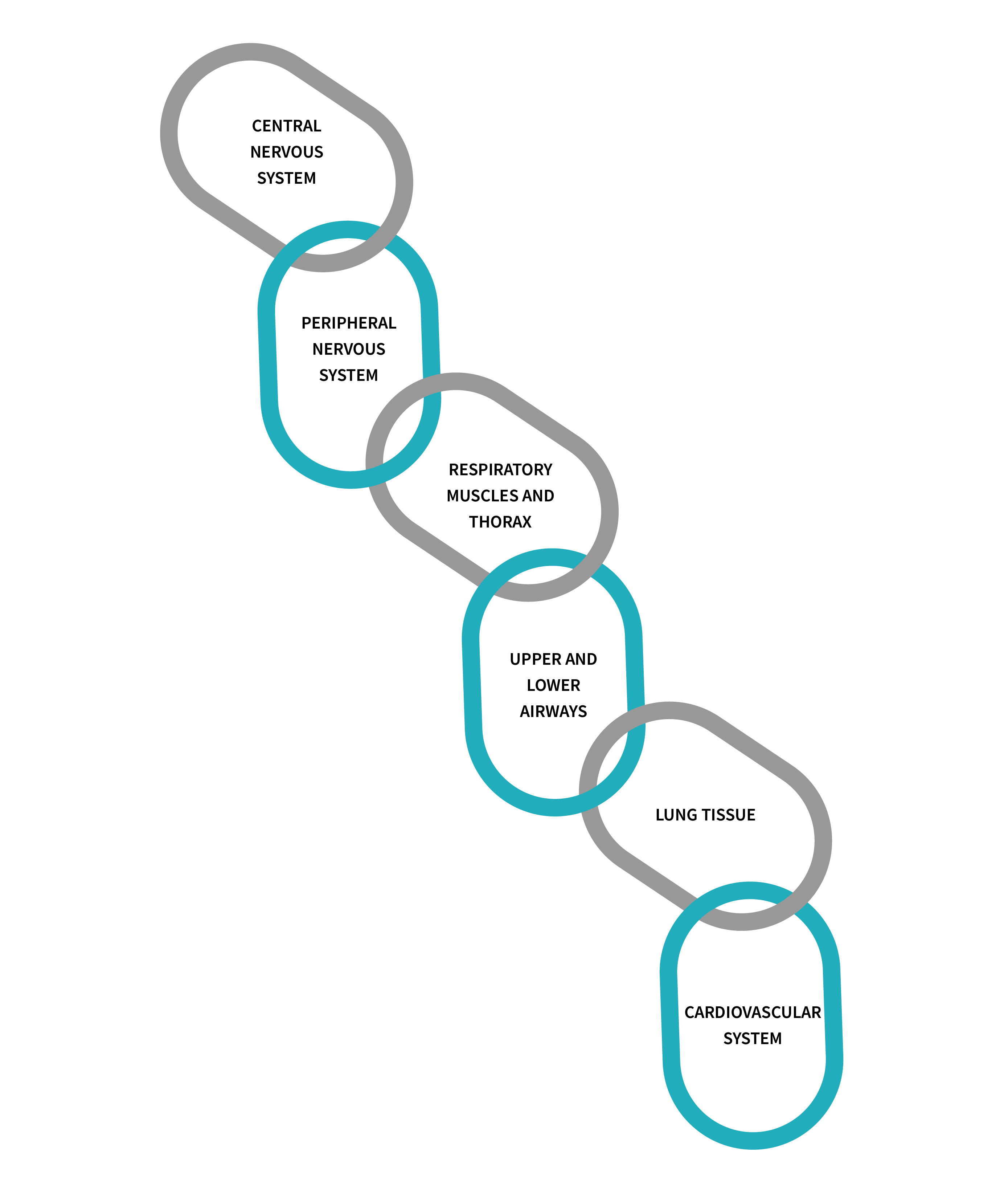
A problem with any of the first three components of this chain results in CO2 retention. In hypercapnic respiratory failure, the lungs fail to remove an adequate amount of CO2 due to inadequate alveolar ventilation, leading to an imbalance in the blood gases. Hypercapnic respiratory failure, also known as Type II ventilatory failure or pump failure, can be acute or chronic and is characterized by increased levels of CO2 in the blood, leading to respiratory acidosis.
In a healthy respiratory system, the lungs help eliminate CO2 by exchanging it with oxygen during breathing. Ventilation refers to the movement of air in (O2) and out of the lungs (CO2). A detailed patient assessment will identify problems with ventilation. Parameters used to identify ventilatory problems will be described later in this chapter. Ventilation is simply described as the product of tidal volume and respiratory rate.
[latex]\begin{align*}V_E&=RR\times V_T\text{ where}\\V_E&=\text{Minute Ventilation},\\V_T&=\text{Tidal Volume},\\RR&=\text{Respiratory Rate (Frequency)}\end{align*}[/latex]
Object Lesson
Arterial level of CO2 (PaCO2) and Alveolar ventilation are inversely related. Higher alveolar ventilation leads to increased oxygen concentration and decreased CO2 concentration in the alveoli. Conversely, lower alveolar ventilation results in decreased oxygen concentration and increased CO2 concentration in the alveoli.
* PaCO2 is the single best index of alveolar ventilation.
Check Your Knowledge
What causes Hypercapnic respiratory failure?
Answer
The main causes of hypercapnic respiratory failure are impairment of the central nervous system, including neuromuscular transmission, mechanical defect of the thorax, and respiratory muscle fatigue.
Alveolar Ventilation and Dead Space
While minute volume provides an overall estimate of ventilation, alveolar ventilation provides information on the effectiveness of ventilation. Alveolar ventilation is determined by substracting physiological dead space ([latex]V_{Dphys}[/latex]) from tidal volume:
[latex]V_A=(V_T-V_{Dphys})\times RR[/latex]
[latex]V_A=[/latex] Alveolar Ventilation, [latex]V_T=[/latex] Tidal Volume, [latex]V_{Dphys}=[/latex] Physiologic dead space, [latex]RR=[/latex] respiratory rate (or frequency)
 |
 |
Object Lesson
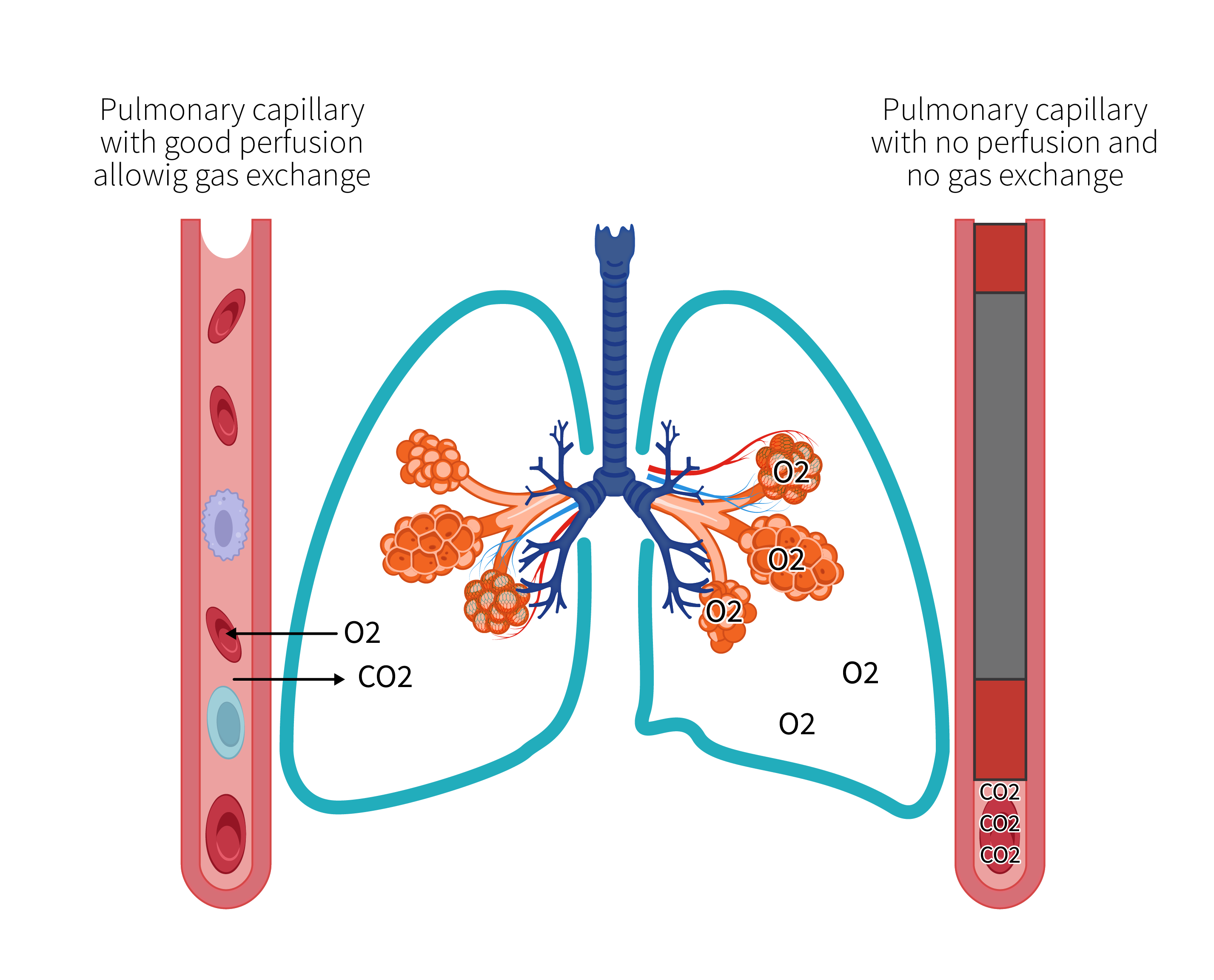
Recall from Chapter 1, physiologic dead space is the sum of anatomic dead space and alveolar dead space. Under normal circumstances, anatomic dead space is almost the same as physiologic dead space. In dead space causing diseases, however, physiologic dead space increases.
*Dead space refers to ventilated alveoli, that are not perfused.
When an increase in dead space ventilation is suspected, the dead space to tidal volume ratio [latex](V_D/V_T)[/latex] can be determined with a simple calculation at the bedside using the Bohr-Enghoff equation. [latex]V_D/V_T[/latex] is a physiological measurement that assesses the efficiency of gas exchange in the lungs. It represents the proportion of each breath that is occupied by dead space, which is the volume of air that does not participate in gas exchange. This calculation requires collection and analysis of arterial blood gases and measurement of exhaled CO2.
[latex]\frac{V_D}{V_T}=\frac{(\text{P}_{\text{a}}\text{CO}_2-\text{P}_{\text{E}}\text{CO}_2)}{\text{P}_{\text{a}}\text{CO}_2}[/latex]
Where:
[latex]\frac{V_D}{V_T}[/latex] represents the physiological dead space to tidal volume ratio.
PaCO2 is the partial pressure of carbon dioxide in arterial blood.
PECO2 is the partial pressure of carbon dioxide in the mixed expired gas.
Check Your Knowledge
Can pulmonary embolism contribute to dead space ventilation?
Answer
Yes. When a pulmonary artery becomes obstructed by a blood clot, the blood flow to that specific lung region is compromised, leading to a ventilation-perfusion (V/Q) mismatch with ventilated alveoli that are not perfused, and increased dead space.
Significant reduction in alveolar ventilation, with subsequent hypercapnia, can result from impairment of central nervous system, such as drug overdose, tumors, intracranial hemorrhage with increased intracranial pressure (ICP), or traumatic brain injury. As previously discussed, unless supplemental oxygen is administered, patients experiencing hypoventilation will present with hypoxemia as well. Under normal circumstances, the body has the ability to respond to hypercapnia and hypoxemia by increasing respiratory drive (increasing alveolar ventilation). When the central nervous system is compromised, this response is reduced. These patients will require supplemental oxygen and ventilatory support. Neuromuscular disorders often lead to hypercapnic respiratory failure due to respiratory muscle impairment caused by problems with nerve damage, neuromuscular junction, or muscle damage.

