5.6 Pressure Control Ventilation
Now that we have fully discussed volume control ventilation, we will move on to pressure control. All of the principles we have learned so far still apply. The main difference between the two categories of ventilation is that in volume control, we set the volume, but in pressure control, we do not directly set the volume. Instead, in pressure control, we set the pressure.
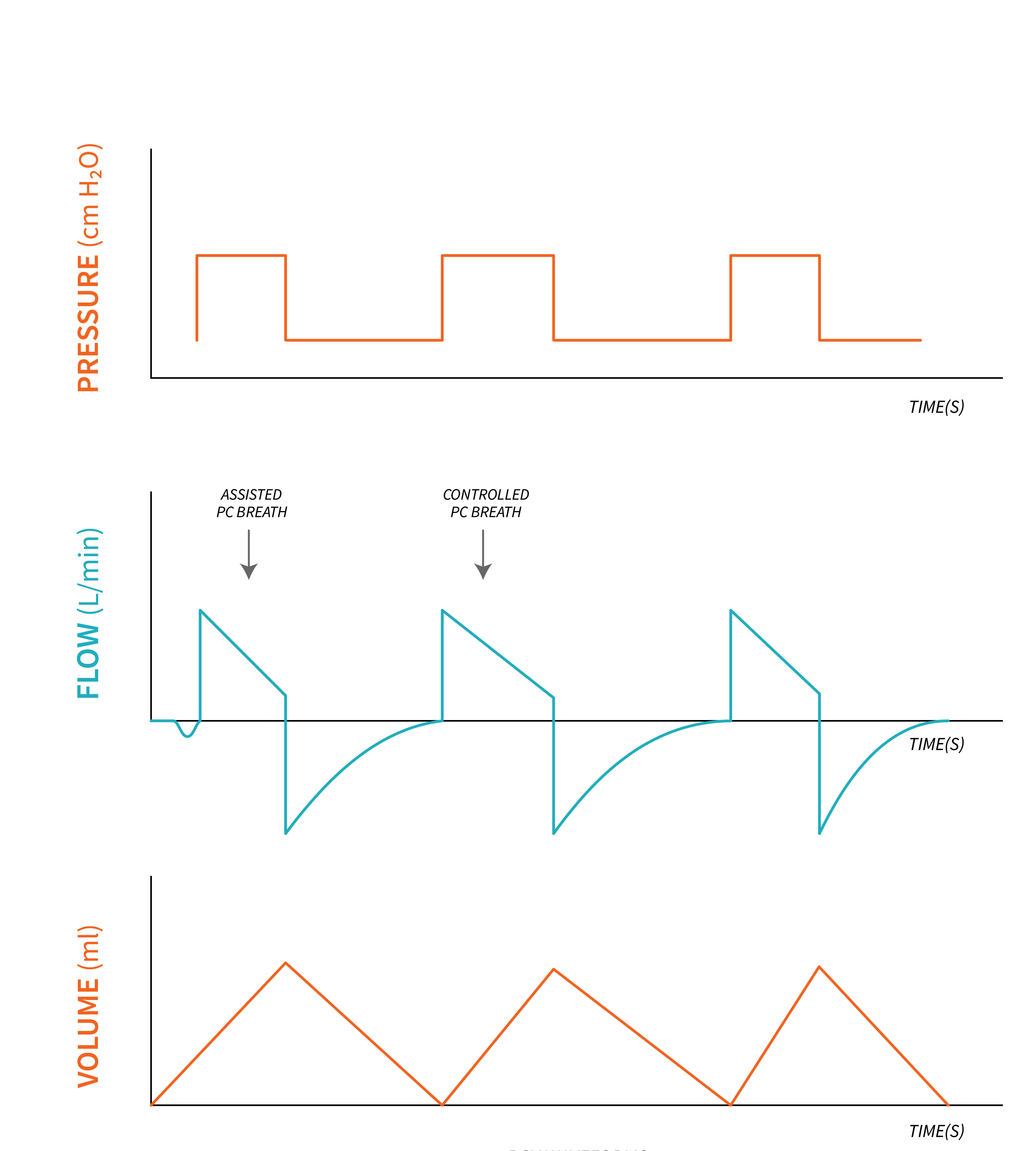
Pressure Control Ventilation (A/C-PC, PCV, CMV-PC) is a full control mode of ventilation—the ventilator will control almost all phases of the breath delivered based on the set parameters. The word “almost” all phases, is intentional, to allow inclusion of patient triggering a breath. In the absence of patient inspiratory effort, the ventilator controls ALL phases of the breath. Exhalation is still passive. The clinician sets a minimum respiratory rate and sets the positive pressure applied (pressure control) to the lungs that causes the lungs to inflate with volume. The pressure delivered is constant and does not change breath to breath unless the clinician changes it.
Apply Your Learning
Volume will vary based on changes to the set pressure control. The higher the pressure delivered, the higher the volume. But just like volume control where the pressures can change breath to breath based on lung condition, we see the same thing in pressure control with the volume changing breath to breath based on the compliance and resistance of the lungs. If the compliance increases, the same pressure control will give you a larger volume. If the resistance increases, this will decrease the volume into the lungs.
Think back to the analogy of the balloon versus the tire for compliance. If no change in pressure is applied, which object will inflate larger with the same pressure?
Now, recall the analogy of lane closures on a highway for resistance in the airways. How would opening a lane back up—decreasing resistance—affect the volume of traffic getting through?
With the same amount of pressure given, the balloon would inflate quicker and easier than a tire, resulting in a higher volume inside the balloon. The same thing occurs with lungs. With the same pressure control settings, “stiffer” lung tissue that has poor compliance or increased resistance will exhibit smaller volumes than “healthy” lungs with normal compliance and resistance.

Let’s apply this concept to our asthma patient. During an acute asthma exacerbation, their airway has increased resistance to air coming in. Any pressure being pushed in would conclude with less volume in the lungs compared to a healthy lung with normal airway resistance. Asthmatic airways decrease the flow of air getting into the lungs and resist inflation. If bronchodilators were given and the airways started to open, the lung volumes would start to increase as the airway resistance starts to return to normal.
Apply Your Learning
In pressure control, the volume being delivered over time is an additional vital sign that you can trend to see whether the lungs are improving or getting worse. Volumes must be continuously monitored to ensure they are enough to effectively ventilate your patient, but not too high that they cause damage. Pressure control (Inspiratory Pressure) should be limited to deliver tidal volumes within a safe range for the patient’s lungs.
Key Takeaway
|
Summary of Basic Settings |
|
|---|---|
In A/C pressure control, you will directly set:
|
In A/C pressure control, you will observe but not directly set:
|
The clinician will set how often a minute the breaths are being delivered. Also set is the driving pressure of air into the lungs, as well as the amount of time the pressure is applied for [latex](T_i)[/latex]. What is not set in Pressure Control Ventilation (A/C-PC) is the specific volume being given. The volume is a direct product of the amount of driving pressure (PC), and the time that pressure is applied for [latex](T_i)[/latex]. In other words, the pressure and time delivered would be set, and the volume would be an outcome of how long and how hard the ventilator pushes air into the lungs.
Inspiratory Flow is not a set parameter either. The clinician sets the Inspiratory time [latex](T_i)[/latex] that the breath is delivered for, but the patient can alter the amount of flow that is being given by the ventilator, pulling whatever flow they require for the duration of time indicated in the set inspiratory time.
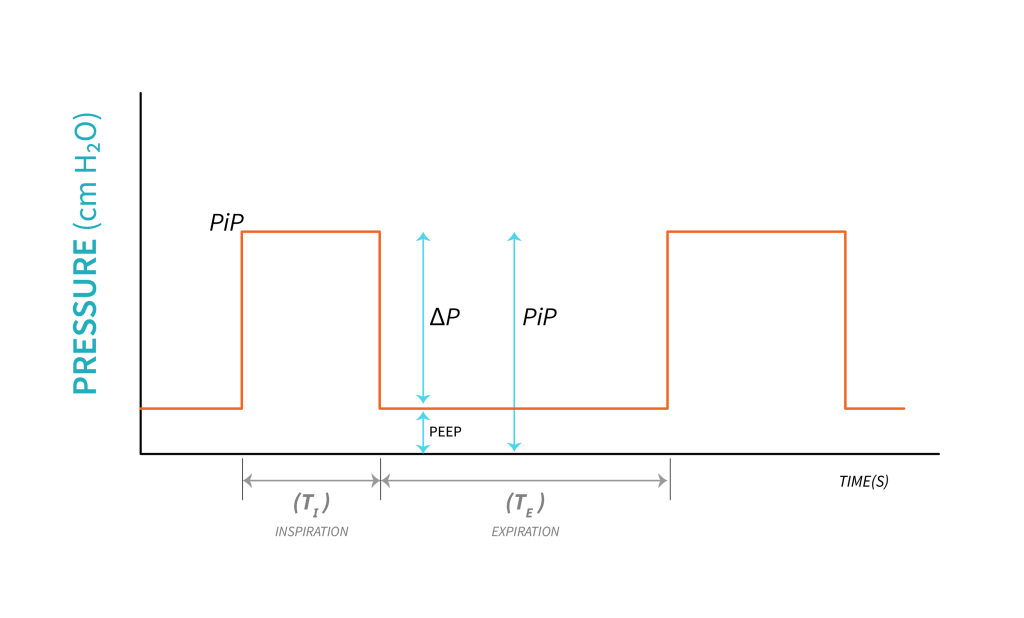
Depending on the ventilator, the clinician sets Peak Inspiratory Pressure in some occasions, and in others, driving pressure (PC or [latex]\Delta P[/latex]). When Peak Inspiratory Pressure (PIP) is not directly set by the clinician ([latex]\Delta P[/latex] is set instead), it remains very controllable in pressure control ventilation as it is the sum of all pressures experienced in the lungs [latex](\text{PIP}=\text{PEEP}+\Delta P)[/latex]. The PIP is the highest pressure being delivered to the alveoli. Since the pressure being delivered [latex](\Delta P)[/latex] is set, the PIP is the [latex]\Delta P[/latex] plus whatever baseline you were at (PEEP). Think back to the mountain range analogy. Standing at the bottom of a mountain, you are not at sea-level altitude. How high is the peak? It’s not just “how high the mountain is”. The altitude at the peak would be the total altitude above sea level, which would be the altitude at basecamp (PEEP), plus the height of the mountain [latex](\Delta P)[/latex]. Take look at these two examples:
- [latex]\text{PEEP }5+\Delta P\text{ 10}=\text{PIP }15[/latex]
- [latex]\text{PEEP }8+\Delta P\text{ 12}=\text{PIP }20[/latex]
Apply Your Learning
Now you try! Your ventilator settings are: [latex]\text{PEEP }6,\Delta P\;15[/latex]. What is your PIP? What would your PIP be if you decrease [latex]\Delta P[/latex] to [latex]12[/latex]?
What will your PIP be, if you increase PEEP to [latex]8[/latex]?
When Peak Inspiratory Pressure (PIP) is directly set on a ventilator, the baseline PEEP will be included in that setting. PIP is still the sum of [latex]\text{PEEP}+\Delta P[/latex], however, [latex]\Delta P[/latex] is determined by the PIP and PEEP settings [latex](\text{PIP}-\text{PEEP}=\Delta P)[/latex].
For example, if we set [latex]\text{PIP}=20[/latex] and [latex]\text{PEEP}=5[/latex], [latex]\Delta P[/latex] is [latex]20-5=15[/latex]. Tidal volume will be determined by how much air can be pushed into the lungs with a pressure of [latex]15[/latex]. If we want to increase tidal volume, we would want to increase [latex]\Delta P[/latex], but this ventilator does not offer that feature directly. Instead we can increase PIP to increase the difference between PIP and PEEP, which is [latex]\Delta P[/latex].
Apply Your Learning
With a PEEP of [latex]6[/latex] and PIP of [latex]22[/latex]. What is [latex]\Delta P[/latex]?
What will [latex]\Delta P[/latex] be, if you increased PEEP to [latex]8[/latex]?
The [latex]\text{I:E}[/latex]—as previously explained—is very important to ensure the patient has adequate time to exhale and decrease the risk of auto-PEEP (air-trapping). The clinician sets the Inspiratory time and the respiratory rate, but not the [latex]\text{I:E}[/latex] directly. The [latex]\text{I:E}[/latex] is the outcome of those settings and will remain constant as long as the [latex]RR[/latex] and inspiratory time remain unchanged. If the patient starts to trigger breaths above the set [latex]RR[/latex], the [latex]\text{I:E}[/latex] will change as the total [latex]RR[/latex] increases with patient-triggered breaths.
Remember, [latex]T_i[/latex] is important to ensure the [latex]\text{I:E}[/latex] is not an inverse ratio. There should always be more exhalation time than inspiration. If needed, the [latex]RR[/latex] or [latex]T_i[/latex] can always be adjusted to ensure adequate expiration time.
Key Takeaway
When thinking about the impact that pressure and volume have on each other and how lung compliance will affect the pressures or volumes in the lungs, always think about balloons. When thinking about how a settings change will affect the opposite, think of two identical balloons with the change to how you are blowing into the balloon (the ventilator pushing the air based on the settings). When thinking about how lung compliance and resistance affects the pressure or volumes, think about the balloon and the tire and remember what settings are constant (volume or pressure) depending on what mode you are in. From there, consider how you would need to change the set parameters to achieve the inflation you want.
Knowing that pressure is the control variable and it stays constant for every breath in pressure control ventilation, consider the impact of changing lung compliance or airway resistance on ventilation. In pressure control ventilation, with constant pressure, when compliance decreases, less tidal volume will be delivered to the lungs. The same will happen when airway resistance increases.
Now, what about [latex]P_{TA}[/latex] and [latex]P_{plat}[/latex] in pressure control ventilation? The still play important roles. When analyzing the pressure-time waveform, it may seem that [latex]P_{TA}[/latex] is equivalent to [latex]P_{plat}[/latex] due to their square shape. However, this assumption is incorrect. [latex]P_{plat}[/latex] is actually measured under conditions of no flow, where only elastic pressure is evaluated.
PIP is determined by the combined effect of both elastic and resistive pressures acting on the lungs. To identify the specific component causing low volume, an inspiratory hold can be performed. This allows us to differentiate between resistive [latex]P_{TA}[/latex] and elastic [latex]P_{plat}[/latex]. By evaluating the elastic pressure that distends the lung under zero flow conditions, we gain insights into the lung’s distensibility.
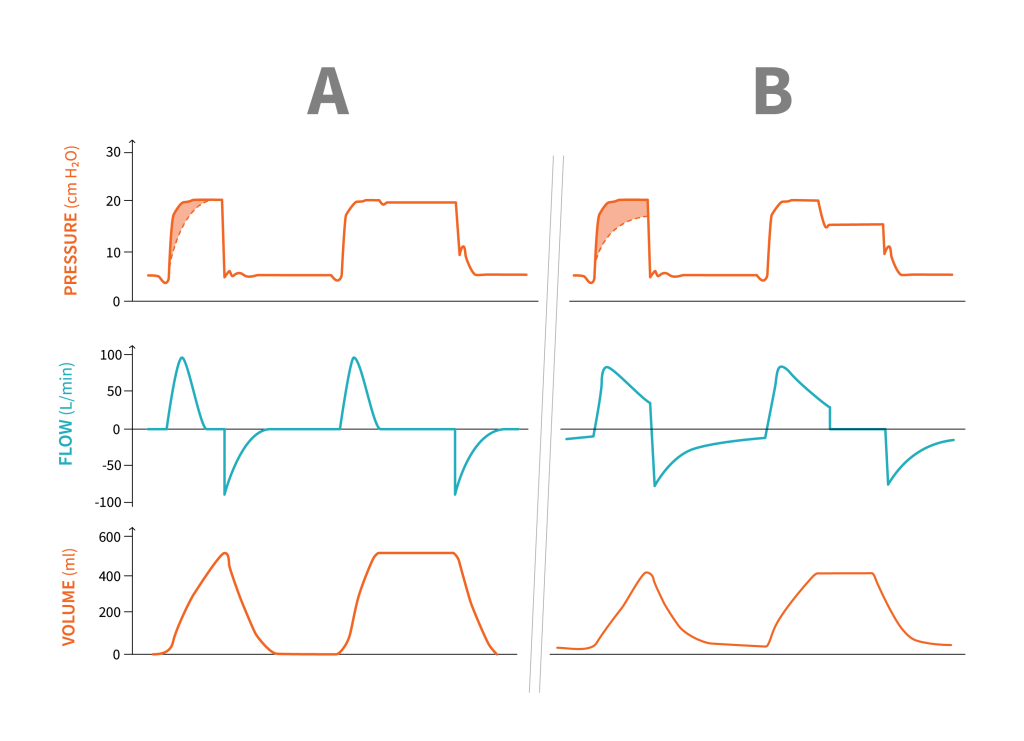
Let’s examine the diagrams provided. In subject A, where resistance is low, flow reaches zero at the end of inspiration. Consequently, PIP is very close to or equal to [latex]P_{plat}[/latex]. On the other hand, subject B, with increased resistance, experiences incomplete flow cessation at the end of inspiration resulting in a lower [latex]P_{plat}[/latex] compared to [latex]P_{peak}[/latex]. This indicates that more of the total pressure generated by the ventilator is utilized to overcome the resistance to flow.
Please refer to the accompanying diagrams for a visual representation of these concepts.
I hope this clarifies the distinction between [latex]P_{TA}[/latex] and [latex]P_{plat}[/latex] in pressure control ventilation. If you have any further questions or require additional clarification, please feel free to ask.
For more information on this topic, read this excellent article on the topic:
Regardless of whether you ventilate in pressure control or volume control, it is important to constantly monitor the volumes being delivered and the peak pressures being experienced by the lungs. Both of these values, if left unchecked, can cause overdistention of the alveoli and result in damage. High pressures can result in barotrauma while high volume causing damage is referred to as volutrauma.
When would you use Pressure Control or Volume Control? Realistically, both modes can achieve similar outcomes as long as the clinician is setting patient-oriented ventilator settings and ventilator outcome parameters closely to ensure lungs are not exposed to over distention via barotrauma or volutrauma. Patient comfort should also be closely monitored, and settings such as RR, flow, and Itime should be changed to achieve optimal matching of patient’s demands. This approach will improve comfort and ensure ventilator synchrony—where breath delivery is matching the timing of the patient’s physiologic effort.
“Pressure Control Ventilation” from Basic Principles of Mechanical Ventilation by Melody Bishop, © Sault College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.

