8.1 The Theory behind Acid-Base and ABGs
On an ongoing basis, the human body is engaged in a complex balancing act—the pH of the body and blood. All of our cells and organs operate best at a specific pH. This level is referred to as the body’s homeostasis. There are two byproducts produced by different systems in the body that affect the pH of the body: carbon dioxide (CO2) and bicarbonate (HCO3). CO2 and HCO3 are monitored and altered by the body to insure a balanced pH. The brain oversees this balancing act by turning up or down specific processes in the body to regulate the levels of CO2 and HCO3 to try to get back to “normal” or balanced pH. Therefore, testing the blood levels of CO2 and HCO3 and checking the pH of the blood is a very quick and effective way of assessing how well the body is doing. Abnormal levels are often one of the first signs of deterioration and can help clinicians know whether they may need to intervene and support a patient to prevent respiratory or organ failure.
Acid-base balance and ABGs is a huge topic that could be an entire book. This chapter will focus on the main concepts you need to know and why the acid-base balance is important when it comes to how humans, specifically your patients, need to breathe. Let’s dive into this concept of body pH, CO2 and bicarbonate levels a little more…
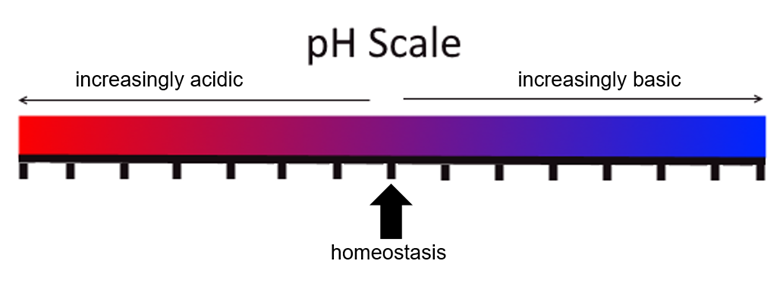
What is normal? The body is in homeostasis and happy with pH levels of [latex]7.35\text{ - }7.45[/latex]. This range is considered normal. If the pH of the body goes lower than [latex]7.35[/latex], the body pH is acidic. If the pH goes higher than [latex]7.45[/latex], the body pH is basic or alkaline.
Look at the following pH scale for a visual model of the spectrum from acidic (left) to basic (right) with a healthy and balanced homeostasis between them.
Carbon dioxide—the waste of every cell on a molecular level—is a potent acid. All cells create CO2 in the process of cellular respiration. Remember high school biology? You probably learned that CO2 is created as a waste product during the Krebs cycle. If left unchecked, the excess CO2 production would leave the body in a highly acidic environment.
Object Lesson
This acid (CO2) must be buffered—neutralized—by the body and then cleared out of the system. The entire focus of the acid base status is to neutralize the amount of CO2 present until it can be cleared by the lungs. Remember, we exhale CO2.
So how does neutralization happen, and how does the body regulate the pH without becoming acidic? Regulating pH can happen by two methods:
- Neutralization (buffering the acid)
- CO2 Clearance (acid removal)
Neutralization
The kidneys play the main role in neutralizing and regulating the pH of the body. Cellular processes can create acids at high rates and to combat this effect, the kidneys are able to regulate an important electrolyte that buffers, or neutralizes, any acid that is present. Bicarbonate is a negative ion that can bind to acidic Hydrogen (H+) ions in the body to get rid of circulating acid. In essence, bicarbonate (HCO3) “buffers” or neutralizes the circulating acid to stabilize the pH of the body. HCO3 is the most important electrolyte when it comes to the body’s regulation of pH. The combined compound carbonic acid (H2CO3) circulates in the body until it reaches the lungs where it breaks down into CO2 and is exhaled. The kidneys play the main role in neutralizing the acids by excreting acid in the urine while conserving or eliminating bicarbonate to ensure the perfect amount is present in the body to neutralize all the CO2 that is present. This process is referred to as the metabolic component of the ABG.
The constant buffering process looks a little like this:
[latex]\text{CO}_2+\text{H}_2\text{O}\leftrightarrow\text{H}_2\text{CO}_3\leftrightarrow\text{H}\style{font-family:Arial}{\text{+}}+\text{HCO}_3\style{font-family:Arial}{\text{-}}[/latex]
CO2 Clearance
The other method of maintaining homeostasis is by CO2 clearance. CO2 is cleared out of the body through the lungs. CO2 is carried in the blood stream to the alveolar-capillary membrane where it diffuses into the alveoli to be exhaled with every breath. This process is referred to as the respiratory component of an ABG.
Any alterations to normal physiology or any disease process can cause changes to CO2 levels. These changes could occur in two ways:
- Changes in CO2 production of the cells, causing higher or lower levels to be circulating in the body (e.g., illness, increased metabolism, exercise)
- Changes to how much CO2 is eliminated by the alveoli—changes in gas exchange or increased/decreased CO2 amounts being exhaled every minute (e.g., changes to the respiratory rate or volume of breathing; impaired lungs that cannot contribute to gas exchange)
Either way, if either of these changes occur, the level of CO2 in the body can quickly start to increase or decrease. Remember: if you think of CO2 as an acid, any increase in CO2 would cause the pH to become acidic, while decreases in CO2 (acid) would cause the pH to become more alkaline (basic). Chemoreceptors in the brain—the same ones we talked about in Chapter 1—sense this change and try to drive the body back to homeostasis via two mechanisms:
- by altering the breathing pattern of the body, and
- by changing the levels of bicarbonate in the body.
The first line of defense for restoring acid-base balance is the respiratory system and altering the breathing pattern of the body, as this adjustment can be done immediately with effects being seen within minutes. As discussed in Chapter 1, higher levels of CO2, or more specifically a decrease in pH (becoming more acidic), will trigger the brain to stimulate the patient to breathe more to help clear more CO2. More importantly, increased breathing drives the pH back to a normal level because that is where the body functions best at.
The second line of defense for restoring acid-base balance is the metabolic process of the kidneys and changing bicarbonate levels. This process takes more time as HCO3 is either excreted in the urine or reabsorbed in the urinary system and needs time to be reabsorbed by the body. The metabolic process takes upwards of 24 to 48 hours to correct an imbalance. Though slower, bicarbonate levels can also regulate pH levels back to physiologic normal (7.35-7.45), so the respiratory system does not have to continue to do all the “work”.
The difference in correction time is an incredibly important differentiation to understand. Respiratory changes happen within minutes, while metabolic changes take 24 hours to start working. If for any reason a person’s drive to breathe is altered due to injury or illness, the ability of the brain to correct acid-base imbalances in the short term immediately disappears. Small alterations in pH can cause very large changes in level of consciousness and can be life threatening very quickly. If left uncorrected, the bicarbonate may not have enough time to change before the balance becomes life-threatening. This condition is termed respiratory failure (or ventilatory failure), and it requires some type of ventilatory support—in most cases mechanical ventilation. Mechanical ventilation is a clinician’s way to impact and change the patient’s current acid-base status when their own physiologic ability has become compromised or is deemed inadequate.
Don’t sweat it if you don’t really get it. The main takeaway messages are that the body wants to stay at a pH of [latex]7.35\text{ - }7.45[/latex] for vital organ and cellular functions to occur optimally. It achieves this by regulating the amount of CO2 and bicarbonate in the body. Remember:
- Bicarbonate = alkaline
- CO2 = acidic
As long as you have enough bicarbonate in the body to equal out the CO2 amount, the body will stay in balance.
Key Takeaway
Learn More
If you want more details about what you learned on this page, further reading on this topic can be found here:
“The Theory behind Acid-Base and ABGs” from Basic Principles of Mechanical Ventilation by Melody Bishop, © Sault College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.


