7.1 Why Do we need mechanical ventilation – Respiratory Failure Type I
Respiratory failure occurs when the cardio-respiratory system is unable to provide adequate tissue oxygenation and/or CO2 removal. This condition can become life threatening, and it is important for respiratory therapists to recognize impending respiratory failure and take appropriate action. Respiratory Failure can be classified as acute or chronic.
Key Takeaway
Acute Respiratory Failure (ARF) has a sudden onset and may present with hypoxemia alone, or hypoxemia may be accompanied by hypercapnia. Acute Respiratory Distress Syndrome (ARDS) is a severe form of Respiratory Failure, and will be discussed later. Chronic Respiratory Failure is often caused by chronic lung disease or neuromuscular disease.
Reasons for mechanical ventilation due to respiratory failure can fall into two main categories:
- Hypoxemic respiratory failure (also called hypoxia or Type I respiratory failure) is the inability to oxygenate the body adequately. Issues with the lungs, circulating blood, or the heart can result in inadequate oxygen being delivered to the organs and tissue. If not corrected, this low oxygen can cause organ failure and irreversible damage.
- Hypercapnic respiratory failure (also called pump failure or Type II respiratory failure) is characterized by high CO2 levels and can occur because of compromised breathing or other illnesses in the body. If CO2 increases to a level the body cannot clear by increasing breathing, mechanical ventilation is indicated. An ineffective drive to breathe can also occur if there is an injury to the brain or neurological control to breathing, leading to respiratory failure. It can occur with spinal or nerve injuries as well, where the triggers of ventilation do not result in an intact signal to breathe. These cases may require mechanical ventilation to take over the impaired drive to breathe.
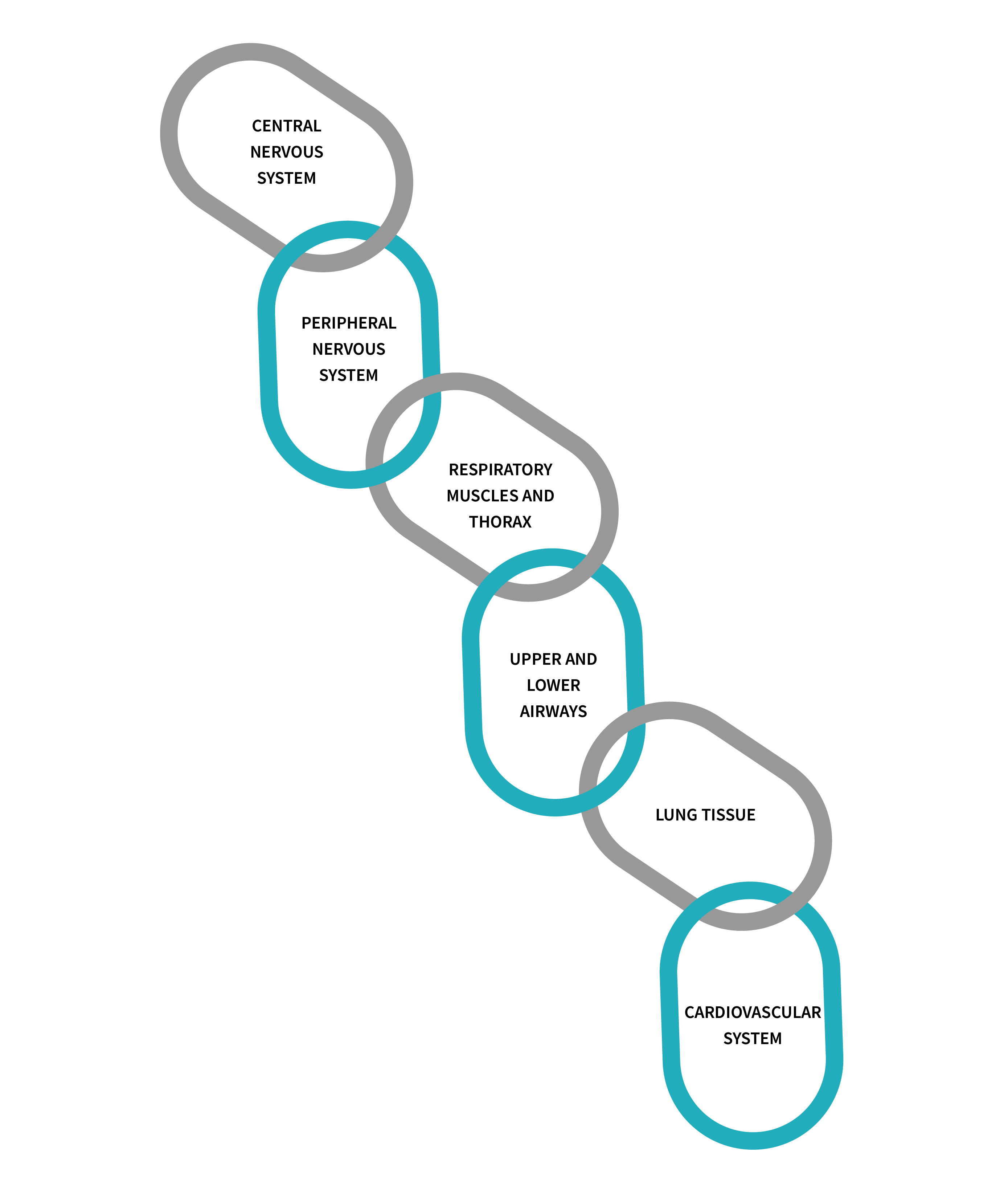
Integrity of the complex system that is required for breathing and maintenance of normal O2 and CO2 levels compatible with metabolic demand is essential to all organ functions. Imagine this complex interaction between respiratory and cardiovascular systems as a chain with multiple links. Problems can arise at any level of this chain. Failure of one or more of links in the chain can lead to development of ARF.
The first three components of this chain represent the “ventilatory pump” and are responsible for alveolar ventilation. A problem with any of these components results in CO2 retention which will eventually compromise oxygenation, limiting alveolar gas exchange. Problems with the next components, airway and lung tissue, result in inadequate oxygenation but normal CO2 elimination, assuming the ventilatory “pump” function is maintained. The last link in the respiratory system chain, representing gas transport in circulation, can result in inadequate O2 delivery to the tissues and CO2 removal. Cases of shock severe anemia and/or hemoglobin dysfunction could also cause ARF. Often, multiple chain links are broken at the same time, resulting in ARF of multiple causes. For example, a patient who suffered a head injury, (involving the central nervous system) lung contusion (involving lung tissue) and hemorrhagic shock (involving circulation) may develop ARF from multiple causes without appropriate intervention.
Remember when we learned about those chemoreceptors in the brain which are sensing oxygen and CO2 levels? Anything that interrupts the signal from the brain to the lungs, or if the signals or subsequent breaths are not adequate for what the body needs, will require ventilation. The body naturally wants to keep the CO2 levels within a desired range and wants to take in enough oxygen to feed the body. When a patient gets sick or has any type of organ dysfunction, this can quickly cause a disruption in the balance of the body by increase the oxygen consumption or increasing the CO2 production of the cells. When this happens, the body will try to compensate, but this compensation can only go so far. As patients get sicker, there may come a point where the oxygen levels are too low (hypoxic failure) or CO2 levels are too high for the lungs to compensate (hypercapnia), and mechanical ventilation is necessary to help restore healthy levels of CO2 or oxygen.

Cyanosis will occur if hypoxic failure is left untreated. Mechanical ventilation will prevent oxygen levels from falling to this low level. The health care provider must always act quickly to treat hypoxic failure.
Hypoxemic Respiratory Failure or Type I Respiratory Failure
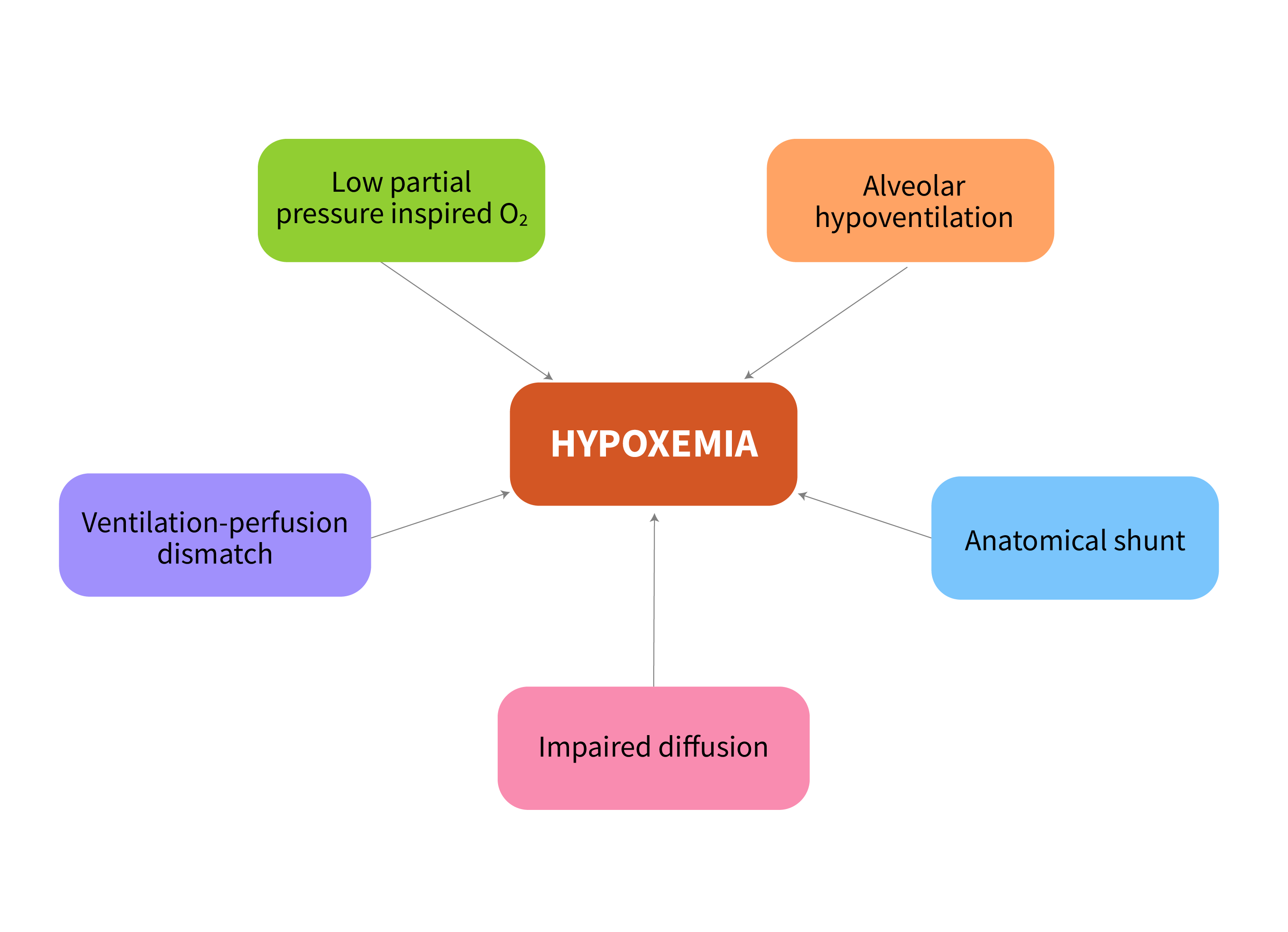
The main causes of Hypoxemic respiratory Failure (Type 1) are Ventilation/Perfusion (V/Q mismatch) or shunt, Alveolar hypoventilation, diffusion impairment, and decreased inspired oxygen.
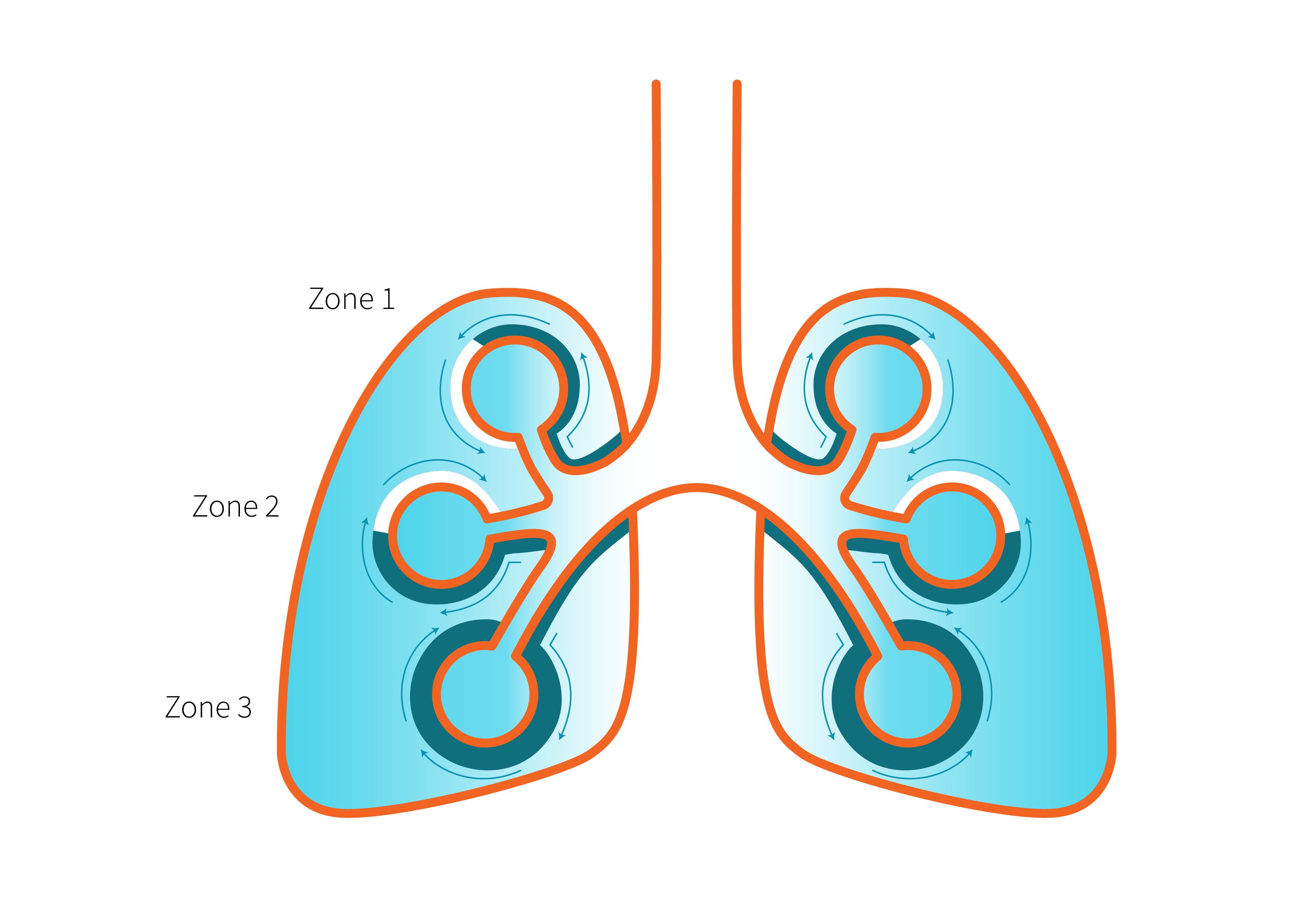
Ventilation/Perfusion Mismatch
- Zone 1: At the top of the lung = VA/Q ratio is increased
- Zone 2: At the middle of the lung= VA/Q = 1
- Zone 3: At the bottom of the lung = VA/Q ratio is decreased
Object Lesson
Ventilation/perfusion mismatch usually responds to O2 therapy, while shunt does not.
Alveolar Hypoventilation
While alveolar hypoventilation is discussed mostly in the context of hypercapnic respiratory failure, it can also lead to hypoxemia. Alveolar hypoventilation refers to a decrease in the amount of fresh air reaching the alveoli, resulting in reduced O2 intake and increased CO2 retention.
When alveolar hypoventilation occurs, the exchange of oxygen and carbon dioxide in the alveoli is compromised. This can lead to a decrease in the O2 content within the alveoli, resulting in lower O2 levels available for transfer into the bloodstream. As a result, the O2 saturation of arterial blood can decline, leading to hypoxemic respiratory failure.
Diffusion Limitations
Diffusion is defined as the movement of air and oxygen across the alveolar capillary membrane along a pressure gradient. Diffusion limitation is seen in conditions affecting gas exchange, such as interstitial lung disease, where destruction of interstitium leads to impaired gas exchange. Destruction of alveolar tissue can also impair diffusion. Abnormalities in pulmonary circulation may lead to impaired gas exchange due to reduced blood flow available.
Decreased Inspired Oxygen
Hypoxic respiratory failure caused by decreased inspired oxygen occurs when the body oxygen requirements are greater than available oxygen. Knowing that the concentration of oxygen is the same anywhere on the planet, [latex]21\%[/latex], this low inspired oxygen is seen at high altitude due to decreased atmospheric pressure, or in situations where the body's increased oxygen requirements go unrecognized for prolonged periods of time without appropriate intervention (i.e. provide O2 at higher FiO2).
Check Your Knowledge
"Why Do We Need Mechanical Ventilation" from Basic Principles of Mechanical Ventilation by Melody Bishop, © Sault College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
"Ventilation Perfusion Ratio" from Human Physiology by Human Physiology Students from University of Guelph is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted.

