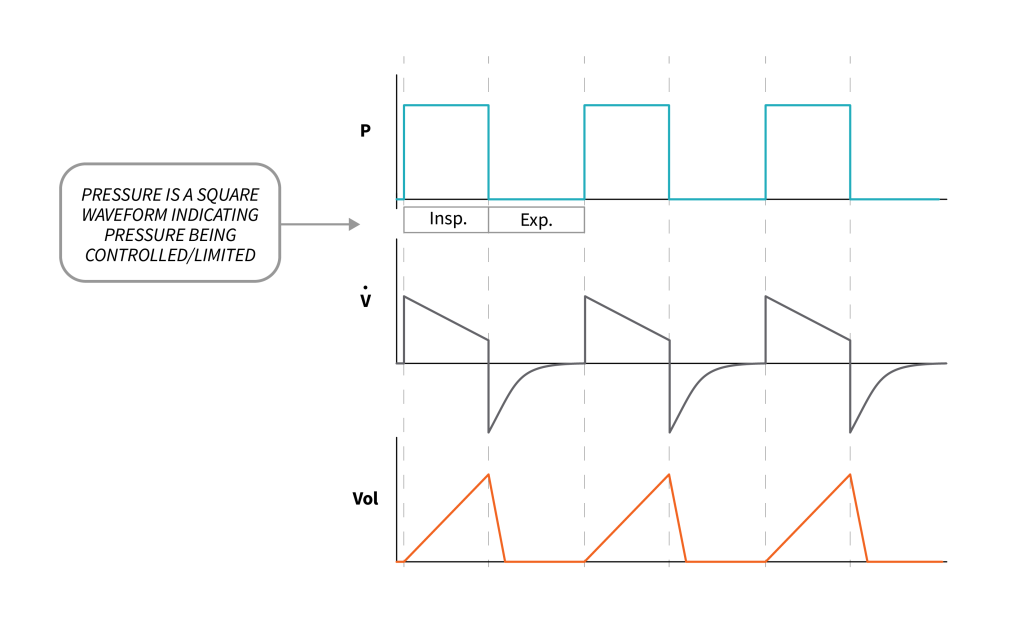
3.5 Pressure Control Ventilation
Ventilation is considered pressure-controlled (pressure-limited), when the ventilator keeps the pressure waveform in a specific pattern. Volume and flow waveforms may change based on changes in lung mechanics. When pressure is the control variable, instead of setting the tidal volume and flow of air directly, remember that we set the pressure applied to the lungs over a specified time that causes the lungs to inflate to a certain volume. All the same rules apply as with IBW and tidal volume. You will still measure your patient’s height and calculate their IBW and their tidal volume range, but instead of setting the tidal volume directly, you will set a pressure to be applied and then watch what volume you see in your lungs after about three breaths:
- Too high? Decrease the PC by [latex]2\text{ cmH}_2\text{O}[/latex].
- Too low? Increase the PC by [latex]2\text{ cmH}_2\text{O}[/latex] and assess.
A safe pressure control to start at is [latex]14\text{ cmH}_2\text{O}[/latex]. Even with a slightly higher PEEP, it will ensure your peak pressures are still well below [latex]35\text{ cmH}_2\text{O}[/latex].
Object Lesson
This change is very quick, and, within approximately a minute, you should be able to adjust the PC up or down to be approximately [latex]8\text{ mL/Kg}[/latex].
Note: Being off by approximately [latex]20\text{ mL}[/latex] is not an issue. You will never be exactly the same. Try to stay under the [latex]8\text{ mL}[/latex] instead of over. If you increased the PC by [latex]1\text{ cmH}_2\text{O}[/latex] and your tidal volumes go from below [latex]8\text{ mL/Kg}[/latex] to above, then undo that change and leave your volumes just below your maximum. Remember [latex]8\text{ mL/Kg}[/latex] is the upper limit, and we do not want our volumes to be above that.
The approach to setting your inspiratory time is very similar to the mentality with flow. A default Inspiratory time of [latex]0.8\text{ - }1.0[/latex] seconds works for most adult patients. A good rule of thumb is to use an Inspiratory time of [latex]1.0[/latex] second. If your [latex]\text{I:E}[/latex] is [latex]\text{1:1}[/latex], you can decrease your Itime by [latex]0.1[/latex] seconds to see if you can ensure your patient has enough time to exhale. Insufficient exhalation time should not be an issue unless your patient is triggering a lot of breaths above your set respiratory rate. The only time the [latex]\text{I:E}[/latex] would end up at [latex]\text{1:1}[/latex] or inverse is with high set RR (or patient triggering more breaths). Sedation could be considered in this case or a different ventilation strategy, when Itime of [latex]0.8\text{ - }1.0[/latex] seconds is causing issues, alarms, or an [latex]\text{I:E}[/latex] that is [latex]\text{1:1}[/latex] or inverse.
Default Itimes of [latex]0.8\text{ - }1.0[/latex] seconds should be fine for all patients as long as the [latex]RR[/latex] is less than [latex]24\text{ bpm.}[/latex] We will learn to make adjustments, such as increasing the [latex]RR[/latex], the I-time may start to be adjusted to ensure the [latex]\text{I:E}[/latex] stays greater than [latex]\text{1:1}[/latex].
|
Setting |
Patient Status |
Initial Setting |
|---|---|---|
| Inspiratory Time (I-time) | Adult patient with [latex]RR[/latex] set less than [latex]24\text{ bpm}[/latex]. Consult an expert clinician if you think the Itime is not appropriate ([latex]0.8\text{ - }1.0[/latex] seconds). |
[latex]1.0[/latex] seconds |
"Pressure Control Specific Settings: The Pressure Control and Inspiratory Time" from Basic Principles of Mechanical Ventilation by Melody Bishop, © Sault College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.

