Masks
Masks are protective coverings worn by healthcare providers to protect the mucous membranes of the nose and mouth. In healthcare, masks are often referred to as medical masks, procedural masks, or surgical masks. Medical masks are secured to the head by strings that are tied around the top and back of the head, or by elastic loops around the ears. The top edge of the mask has a bendable strip to better secure the seal of the mask over the bridge of the nose. Some masks have been combined with a shield or a visor that covers the eyes and can be worn when both a mask and eye covering is required.

Medical mask with visor

Medical mask
Medical masks should be worn during care, treatments, or procedures that may cause splashing or spraying of blood, body fluids, secretions, or excretions; when within 2 meters of a client who is coughing; or when required by routine practices or additional precautions. Medical masks should also be worn by healthcare providers to prevent transmission of exhaled respiratory droplets during certain procedures such as a central line insertion, and surgery or dressing changes that require aseptic technique (PIDAC, 2012).
Medical masks can differ in their filtration effectiveness and the way in which they fit. Single-use disposable medical masks are effective to use when providing care to most clients and should be changed when damp or soiled (Kozier et al., 2018). A medical mask, when properly worn, should fit snugly over the nose, mouth, and under the chin so that microorganisms and body fluids cannot enter or exit through the sides of the mask. If the healthcare provider wears glasses, the glasses should be placed over the top edge of the mask. This will prevent the glasses from becoming foggy as the person wearing the mask exhales. When medical masks become moist, they may not provide an effective barrier to microorganisms. As such, talking should be kept to a minimum, and masks should be discarded when moist (Potter et al., 2019).
Important Considerations when Wearing Medical Masks
Fun Fact about Masks in Healthcare
 It has been speculated that the original masks in healthcare were used during the bubonic plague during the Middle Ages. The masks were shaped like bird beaks so that the beak portion could be filled with strong-smelling substances like cinnamon or cloves. This was thought to protect the medical professionals from breathing in spoiled air from the East, which was thought to be the cause of the pandemic (Matuschek et al., 2020).
It has been speculated that the original masks in healthcare were used during the bubonic plague during the Middle Ages. The masks were shaped like bird beaks so that the beak portion could be filled with strong-smelling substances like cinnamon or cloves. This was thought to protect the medical professionals from breathing in spoiled air from the East, which was thought to be the cause of the pandemic (Matuschek et al., 2020).
Review the section on Putting It All Together for steps included in putting on and removing a medical mask.
Points of Consideration: Universal Masking
Universal masking refers to wearing a mask by all staff and visitors at all times. This policy has been instituted in many healthcare settings since the onset of COVID-19. Universal masking protects the wearer but also functions as source control, a personal practice that prevents the spread of microorganisms to others (Public Health Ontario, 2020a).
Respirators
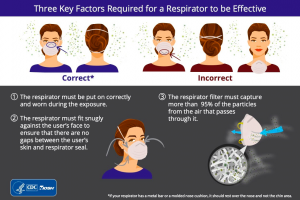
Respirators, like medical masks, are protective coverings worn by healthcare providers to protect the mucous membranes of the nose and mouth. Respirators are made of a high-filtration material that are more effective than medical masks. The N95 respirator is a disposable respirator that filters out 95% of small airborne particles, and is used to prevent inhalation of small particles that may contain pathogens transmitted by the airborne route (Kozier et al., 2018).

Respirators are also designed to fit snugly around the nose and mouth to prevent microorganisms and body fluids from entering or exiting through the sides of the mask. Since faces vary in size and shape, respirators need to be specifically fitted, and not every individual can fit the same respirator (Kozier et al., 2018).
Mask Fit Test
The following video shows what to expect during a mask fit test.
Respirators are secured to the head by tight elastic loops that are secured around the top and back of the head. Once the respirator has been applied, a seal test should be performed to ensure that there is an adequate seal (Kozier et al., 2018). Review steps in Putting On, Checking the Seal, and Removing Respirators.
Respirators should be worn during airborne precautions and procedures that generate aerosols. Aerosol-generating medical procedures, such as tracheostomy care, CPR, and nebulized therapy may increase risk of transmitting infectious agents. Airborne precautions may be initiated during specific procedures if a client is suspected of having or confirmed to have tuberculosis.
Clinical Tip
Respirators should be removed after leaving the client’s room and removed without touching the front of the mask so that self-contamination does not occur (Kozier et al., 2018).
Putting on, Checking the Seal, and Removing a Respirator
Putting on a Respirator
Steps |
Additional Information |
1. Perform hand hygiene. |
 |
2. Place the respirator in your hand with the open portion of the respirator facing up and the nose piece at the fingertips and the straps around the bottom of the hand. |
 |
3. Place the respirator in your hand against your face between the bridge of your nose and under your chin. Allow the straps to hang on the top of your hand. |
 |
4. First pull the top strap so that it rests high on the top of your head. |
 |
5. Pull the bottom strap over the top of the head and position it around the back of the neck and below the ears. |
 |
6. Place your fingertips from both hands at the top of the metal nosepiece and form it over the bridge of the nose. |
 |
Respirator Seal Check
1. Place one or both hands over the respirator and inhale quickly to see if the respirator seals to the face. Then exhale. If the exhaled air is felt, then there is not a proper seal with the mask. |
 |
2. If air leaks around the nose, then readjust the nosepiece. If air leaks around the edges of the mask, then re-adjust the face portion and straps until a proper seal is obtained.Note: If a proper seal cannot be obtained, then do not enter the room and ask for assistance or try a different size or model. |
 |
Removing a Respirator
1. Lift bottom strap from around the neck and over the head without touching the respirator. |
 |
2. Lift the top strap off of the head and avoid touching the respirator. |
 |
3. Discard the mask while holding the straps. |
 |
4. Perform hand hygiene. |
 |
Source: Centers for Disease Control & Prevention & National Institute for Occupational Safety & Health (2010). |
Points of Consideration: Respirators and Facial Hair
(Centers for Disease Control and Prevention & National Institute for Occupational Safety and Health, 2017).

For those with facial hair that cannot be removed, a powered air purifying respirator (PAPR) can be worn. A PAPR uses a blower that forces air through a filter cartridge and into the hood of the wearer. PAPRs that are loose fitting can be worn by healthcare providers with facial hair (Centers for Disease Control abd Prevention, 2019; Ontario Health Quality, 2020).
Clinical Tip
Wearing a Hijab
- Choose hijabs made out of jersey material; the stretchable nature of this material makes it easy to wear masks with ear loops. This also allows easy access for your stethoscope.
- Depending on the availability at your organization, masks ties (as opposed to loops) are convenient as you can secure the tie on top of your hijab. Mask extenders can also be used with surgical masks with ear loops, and secured on top of the hijab.
- A light turtleneck can be worn under your scrubs, in addition to a surgical cap; this allows you to cover both your hair and neck, while protecting yourself.
- Treat your hijab as a part of your uniform. Bring an extra hijab for the commute home, and allocate your scrubs and hijab to their own laundry load on your return home.
- If there is excess cloth hanging from your hijab, this may come in contact with clients when performing assessments or procedures. Tuck excess material into your scrub top or shirt to prevent this from occurring.
- When wearing an N95, go to the washroom, take your hijab off, put your N95 mask on, and then put on your hijab. This ensures a better seal of the N95 mask, instead of putting the mask on top of your hijab.
- N95 strings may make it difficult to loop the strings for a surgical mask with a visor attached behind your ears, so for eye protection, consider wearing a face shield or goggles.
(R. Raham, personal communication, March 15, 2021)
Attribution
This page was remixed with our own original content and adapted from:Clinical Procedures for Safer Patient Care — Thompson Rivers University Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon is used under a CC BY 4.0 Licence. This book is an adaptation of Clinical Procedures of Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, which is under a CC BY 4.0 Licence. A full list of changes and additions made by Renée Anderson can be found in the About the Book section.

