Introduction to Infection Prevention and Control Practices
Infection prevention and control refers to practices that can prevent or reduce the risk of transmission of microorganisms. Evidence-based best practices for infection prevention and control provide guidelines to healthcare providers to ensure safe, quality care is provided to clients, visitors, healthcare providers, and the healthcare environment.
When infection prevention and control practices are used consistently, the transfer of healthcare-associated infections (HAIs) can be prevented in healthcare settings. HAIs are infections that occur when a person is infected with a pathogen during their care in a healthcare setting. A survey conducted by the Canadian Nosocomial Infection Surveillance Program (2020) found that participating Canadian hospitals estimated that 7.9% of clients had at least one HAI. Hand hygiene is considered the most important and effective measure to prevent HAIs. HAIs will be discussed further in Chapter 3.
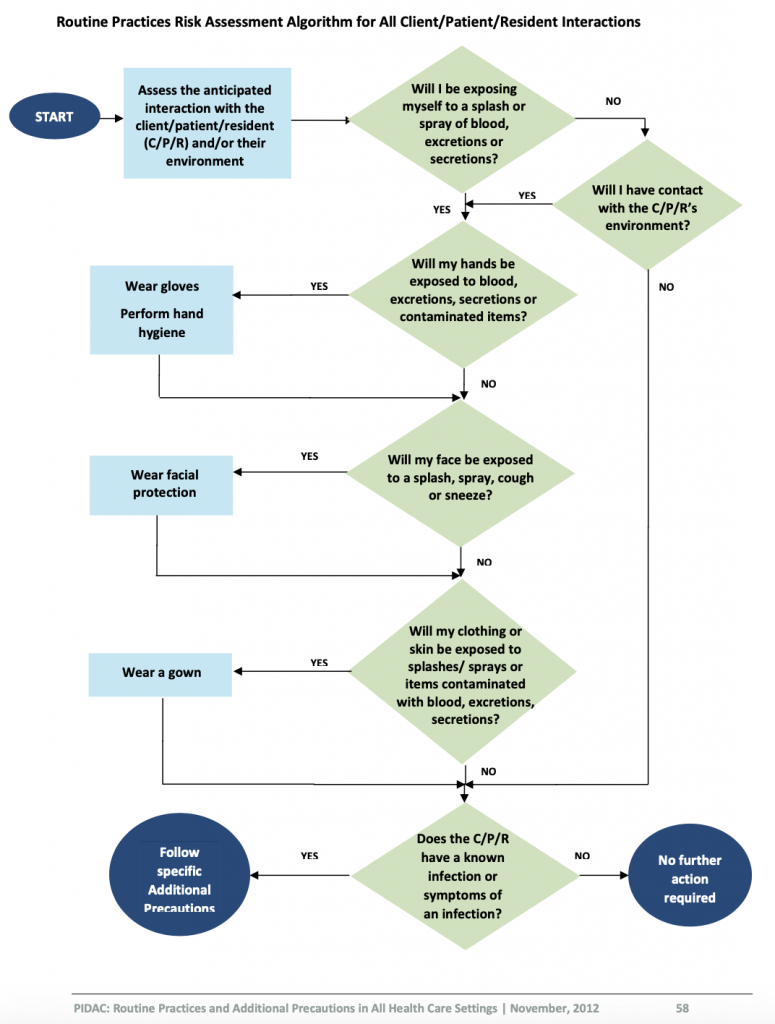
Prior to providing care, healthcare providers must perform a point-of-care risk assessment of the environment before every interaction with clients to ensure safe care and determine the potential risk for exposure to infections. Risks include exposure to blood, body fluids, mucous membranes, non-intact skin, contaminated surfaces or soiled items, and even airborne particles. Once you have completed a risk assessment, you need to assess how to decrease your risk of exposure, determine the infection prevention and control practices required to minimize your risk (e.g., hand hygiene, required PPE) and how to prevent the risk transmission to others (Provincial Infectious Diseases Advisory Committee [PIDAC], 2012).
Performing a risk assessment is foundational in the prevention of infection transmission. Public Health Ontario outlines how to perform a risk assessment related to routine practices and additional precautions (https://www.publichealthontario.ca/-/media/documents/r/2012/rpap-risk-assessment.pdf?la=en).
When performing the risk assessment, you need to ask yourself a series of questions prior to providing care for every client. The answers from the risk assessment will help you to identify and determine which infection prevention and control strategies you need to implement to reduce the risk of transmission of microorganisms.
Performing a Risk Assessment
Review Public Health Ontario (2012) decision trees Performing a Risk Assessment related to Routine Practices and Additional Precautions to determine the steps required by healthcare providers to assess their risk.
Digital Story with Czarielle Dela Cruz
Test your Knowledge on Performing a Risk Assessment
Medical and Sterile Asepsis
There are two types of techniques used to prevent the spread of infections: medical asepsis and sterile asepsis. Medical asepsis, or clean technique, reduces and prevents the spread of microorganisms (Potter et al., 2019). Examples include hand hygiene, using personal protective equipment, and following routine practices.
Sterile asepsis, or sterile technique, is a strict technique to eliminate all microorganisms from an area (Potter et al., 2019). Examples include using steam, hydrogen peroxide, or other sterilizing agents to clean surgical tools.
Routine Practices
Routine practices include performing a point-of-care risk assessment, hand hygiene, wearing the appropriate personal protective equipment (PPE) when needed, respiratory etiquette, safe handling of sharps, controlling the surrounding environment, using avoidance procedures and actions, and following environmental cleaning and disinfecting protocols. To decrease the risk of infections, it is your responsibility to ensure that you understand and consistently follow routine practices with all clients, with every interaction, and in every healthcare setting to prevent and control the transmission of microorganisms (PIDAC, 2012). The principles of routine practices are based on the assumption that all clients are potentially infectious, even when asymptomatic. Infection prevention and control routine practices should be used to prevent exposure to blood, body fluids, secretions, excretions, mucous membranes, non-intact skin, or soiled items (PIDAC, 2012).
All clients can potentially be infectious; thus, it is important to consider which routine practices to follow and why. Routine practices refer to minimum practices that should be used with all clients. Routine practices will prevent transmission of microorganisms from client to client, client to healthcare provider, healthcare provider to client, and healthcare provider to healthcare provider.
Routine Practices include:
Additional Precautions
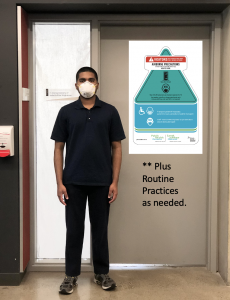
Certain types of infectious microorganisms require additional precautions in addition to routine practices. Additional precautions include contact, droplet, and airborne precautions or a combination of these precautions. The mode of transmission of the infectious agent will determine which additional precautions are required. The client may have a suspected infection according to their clinical signs and symptoms, or could have an infection confirmed with a test result. Healthcare providers must follow the additional precaution guidelines according to the healthcare setting policies.
Additional precautions can include PPE, specialized equipment (e.g., N95 respirator), specialized accommodation and signage, client-dedicated equipment, advanced cleaning protocols, limited movement of the client and specific environmental protocols (e.g., client placement, negative-pressure-engineered rooms). Additional precautions will be discussed further in Chapter 6.
Routine Practices and Additional Precautions
| Routine Practices | Additional Precautions |
| Point-of-care risk assessment. | Routine practices. |
| Hand hygiene. | Additional PPE requirements according to clients confirmed or suspected diagnosis, including contact, droplet, and airborne precautions. |
| Personal protective equipment (PPE) when needed. | Specialized accommodations (e.g., single room, negative pressure room, cohort room, and signage). |
| Respiratory etiquette. | Dedicated client equipment. |
| Safe handling of sharps. | Engineering requirements to control environment (e.g., negative pressurised rooms, filtered air). |
| Controlling the surrounding environment. | Advanced or additional cleaning protocols. |
| Avoidance procedures and actions. | Limited transportation of client throughout the healthcare setting. |
| Environmental cleaning and disinfecting, including medical equipment and linens. | Communication of client’s additional precaution status to interprofessional healthcare team. |
Test your Knowledge
Attribution
This page was remixed with our own original content and adapted from:
Clinical Procedures for Safer Patient Care — Thompson Rivers University Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon is used under a CC BY 4.0 Licence. This book is an adaptation of Clinical Procedures of Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, which is under a CC BY 4.0 Licence. A full list of changes and additions made by Renée Anderson can be found in the About the Book section.
Physical Examination Techniques: A Nurse’s Guide by Jennifer Lapum, Michelle Hughes, Oona St-Amant, Wendy Garcia, Margaret Verkuyl, Paul Petrie, Frances Dimaranan, Mahidhar Pemasani, and Nada Savicevic is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, except where otherwise noted.

