Gloves
Gloves are disposable, one-time-use coverings to protect the hands of healthcare providers. Gloves protect the hands of the healthcare provider from coming into contact with body fluids (e.g., blood, urine, feces, mucous membranes, and non-intact skin) or equipment and other surfaces that may have been contaminated with body fluids. Gloves should not be worn for routine activities such as taking vital signs or transferring a client in a wheelchair, unless indicated. Inappropriate use of gloves has been associated with the transmission of pathogens (PIDAC, 2012). Gloves should also be worn by the healthcare provider when there is a potential chance that they may transmit their own body fluids from non-intact skin on hands to those receiving care.
Gloves are to be task-specific and should not be worn for more than one task or procedure on the same client, as some tasks may have a greater concentration of microorganisms than other tasks. For example, wear gloves to assist a client with incontinent care, but wash hands and put on a new pair of gloves to assist with their oral care. Gloves should never be reused or washed to be used again. Reusing gloves has been linked with the transmission of organisms such as Methicillin-resistant Staphylococcus aureus (MRSA) and Gram-negative bacilli (PIDAC, 2012).
Gloves should always be used in combination with hand hygiene. Gloves should never replace the need for hand hygiene, which should always be performed prior to applying gloves and again after gloves are removed, for several reasons:
- Gloves may have imperfections such as holes or cracks that are not visible.
- Hands may have become contaminated while removing the gloves.
- Gloves may have become damaged while wearing. (PIDAC, 2012).
Ensure that your nails are short prior to applying gloves so that your nails do not puncture them. Don gloves after hand hygiene to ensure your hands are completely dry and choose the appropriate gloves for the activity (see points of consideration below). There is no specific method for putting on gloves. The healthcare provider should be careful when donning gloves to avoid tearing, and donned gloves should completely cover the wrists. When removing gloves, the healthcare provider should use glove-to-glove and skin-to-skin technique so that they do not contaminate themselves.
Gloves can be made of latex rubber (with or without powder), vinyl, or synthetic materials (PIDAC, 2012). Most gloves are not hand-specific and can be worn on either the left or right hand. Gloves come in a variety of sizes such as small, medium, large, and extra large and should have a snug fit, not too tight or too loose, to provide better protection to the healthcare provider.
Points of Consideration: Glove Use
The integrity of gloves differs according to:
- The quality of material of the glove.
- The length of time the gloves were used.
- The type or intensity of work done while wearing.
- Presence of leaks or imperfections of gloves (PIDAC, 2012).
Additional Notes of Importance
- Various types of gloves should be made available to healthcare providers so that gloves can be selected according to use.
- Quality vinyl gloves are appropriate for the majority of tasks.
- Gloves made of synthetic materials or latex (e.g., nitrile or neoprene) are better for tasks that require some degree of manual dexterity or for contact with clients of short duration.
- Use hand-care lotions approved by the facility to ensure the compatibility with gloves.
-
When gloves are worn with a gown, the gloves should be close fitting around the wrist to cover the cuff of the gown providing a better barrier (PIDAC, 2012).
Important Considerations when Wearing Gloves
Application and Removal of Gloves
Safety Considerations:
- Hands must be clean and dry before putting on gloves. Gloves do not replace the need for hand hygiene.
- Hand hygiene must be performed every time gloves are removed. Gloves are not completely free of leaks or 100% tear-proof, and hands may become contaminated when gloves are removed.
- Gloves are for single-client use and must be removed after caring for one client. Reuse of gloves has been associated with transmission of antibiotic-resistant organisms.
- Change or remove gloves if moving from a contaminated site to a non-contaminated site on the same person or if touching the environment.
- Wear gloves that fit properly. Different sizes are available.
- Gloves must be removed immediately and discarded in a waste bin after the activity for which they were used and before exiting a client’s environment.
- Gloves are not required for health care activities where contact is limited to intact skin, such as taking blood pressure.
- Indiscriminate or improper glove use (e.g., wearing gloves all the time) has been linked to transmission of pathogens.
- Gloves should fit snugly around wrists and hands for use with a gown to provide a better skin barrier.
Putting on Gloves
Steps |
Additional Information |
1. Perform hand hygiene with alcohol-based hand rub and ensure that your hands are dry. |
 |
2. Once hands are dry, select the appropriate size of gloves from the box, taking care that only the gloves required are touched. |
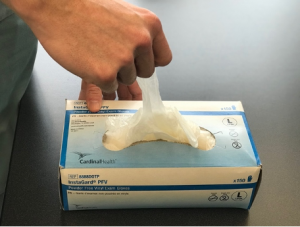 |
3. Apply gloves. Gloves are not hand-specific and no special technique is required. |
 |
4. Adjust the gloves to cover the wrist. |
 |
5. If a gown is worn, ensure that the cuff of the gloves is over the cuff of the gown. |
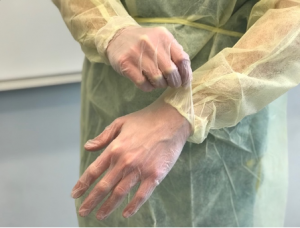 |
6. Complete care as required. |
Removing Gloves Using Glove-to-Glove and Skin-to-Skin Technique
Steps |
Additional Information |
1. Grasp the cuff of the contaminated glove just below the wrist on the palmar surface, taking care not to touch your skin. |
 |
2. Peel the glove off completely by rolling the glove inside out, and hold onto the removed glove in the palm of the remaining gloved hand. |

|
3. Insert two fingers under the cuff of the second contaminated glove. |
 |
4. Using the two fingers, continue to pull off the second contaminated glove by turning it inside out. |
 |
5. Dispose of gloves int the appropriate receptacle. |

|
6. Perform hand hygiene with alcohol-based hand rub and ensure that hands are dry. |
 |
Source: Kozier et al., 2018 |
Test Yourself!
While watching the interactive video on how to remove gloves using the glove-to-glove and skin-to-skin technique, apply your knowledge and critical thinking skills by answering the questions throughout the video.
Please note: there is no sound in this video.
Points of Consideration: Latex Allergy
A latex allergy is a reaction to the proteins in natural rubber latex (American Academy of Allergy, Asthma and Immunology, 2021). When people come in contact with latex, an allergic reaction may occur. Most reactions are mild (e.g., asthma-like symptoms or contact dermatitis), but there are some rare severe cases (i.e., reactions). Many hospitals have moved away from using latex gloves, but latex is commonly used in many healthcare products such as IV tubing, urinary catheters, syringes, dressings, and bandages. People at risk for developing a latex allergy are:
- Healthcare providers and others who frequently wear latex gloves.
- People who have had many surgeries (10+).
- People who are often exposed to natural rubber latex.
- People with other allergies, such as hay fever (e.g., allergic rhinitis), or allergies to certain foods.
Note that powdered latex gloves have also been associated with latex allergies. If an allergy to latex exists, the best treatment is to avoid latex and use a medical alert bracelet to inform others of the allergy (PIDAC, 2012).
Fun Fact About Gloves in Healthcare
In earlier eras, those in obstetric practice used sheep ceca (large intestines) to partially cover their hands before cotton, silk, leather, and rubber gloves arrived in the 19th century. Gloves were initially used to protect the hands from injury and not protect their hands from body fluids (Ellis, 2008).
Attribution
This page was remixed with our own original content and adapted from: Clinical Procedures for Safer Patient Care — Thompson Rivers University Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon is used under a CC BY 4.0 Licence. This book is an adaptation of Clinical Procedures of Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, which is under a CC BY 4.0 Licence. A full list of changes and additions made by Renée Anderson can be found in the About the Book section.
Infection Prevention and Control Practices by Michelle Hughes and Kendra Allen is licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted.



