Introduction to Hand Hygiene
Hand hygiene is the single most effective technique to reduce the transmission of infections, including antibiotic-resistant organisms (ARO) and healthcare-associated infections (HAI) (Provincial Infectious Diseases Advisory Committee [PIDAC], 2014). Hand hygiene is the process of removing, killing, or destroying transient microorganisms or visible soiling from hands (Provincial Infectious Diseases Advisory Committee [PIDAC], 2012). This chapter discusses two hand-hygiene techniques: hand-washing with soap and water, and the use of alcohol-based hand rub (ABHR), also referred to as hand hygiene gel or hand sanitizer. Another form of hand hygiene is surgical-hand antisepsis. However, this method is typically reserved for specific medical procedures like surgery, which will not be addressed in this chapter.
Healthcare providers’ hands are the most common mode of transmission of microorganisms (PIDAC, 2014). As healthcare providers, your hands will touch various people and objects when providing care. As such, microorganisms can easily transfer from your hands to objects in the healthcare setting when proper hand hygiene practices are not followed. When you touch a client, their personal items, medical equipment, or the surrounding environment, you can indirectly transmit microorganisms to the client, another client, yourself, equipment, or transfer it to a new environment. Consistent and effective hand hygiene is required to break the chain of transmission.
Points of Consideration: Risk of Transmitting Healthcare-Associated Infections
According to Health Quality Ontario, from 2019–2020 Ontario hospitals had a rate of 85.6% of healthcare providers that performed hand hygiene before client contact, and 89% after client contact — A 3.4% decrease from 2018–2019.This still leaves a relatively significant number of healthcare providers at risk of transmitting HAIs to another client, themselves, colleagues, or healthcare setting environment due to a lack of hand hygiene.
To break the chain of transmission, according to Public Health Ontario (2014), there are four moments at which to perform hand hygiene when working in healthcare.
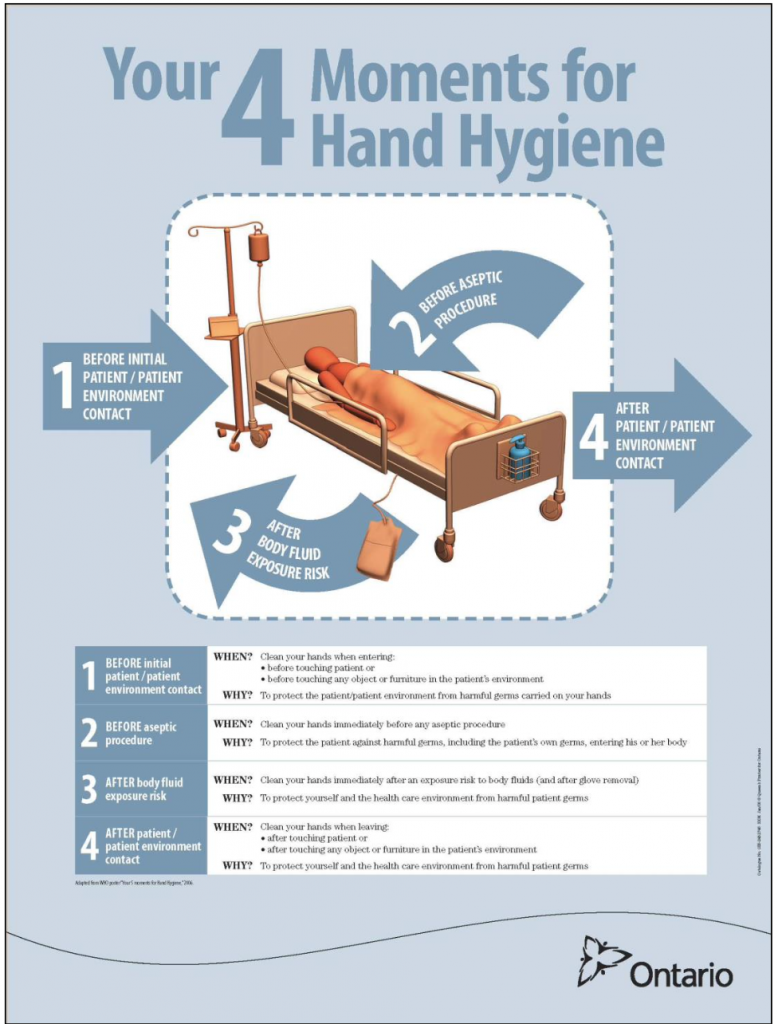
Note: Public Health Ontario’s 4 Moments for Hand Hygiene (PIDAC, 2014) is similar to other healthcare agencies’ guidelines. For example, British Columbia follows the five key moments. The moment “After contact with the client and their environment” is separated into two key points: one focusing on the client and another one focusing on the environment.
Clinical Tip
As soon as you complete your care and tasks with the client and their environment, you need to immediately perform hand hygiene before touching anything (e.g., your glasses, face, or the client’s chart).
Clinical Tip
Gloves do not replace the need for hand hygiene. Glove integrity varies; therefore, hand hygiene must be performed before and after removing gloves.
Hand Hygiene Safety Considerations
- Instruct and support clients and their visitors on the importance of hand hygiene, proper technique, and ways to incorporate hand hygiene routines into everyday practice.
- Certain practices can increase the risk of skin irritation and should be avoided. For example, washing hands regularly with soap and water immediately before or after using an alcohol-based product is not only unnecessary but may lead to dermatitis.
- Use healthcare facility-approved hand lotion.
- Always err on the side of caution, and wash hands whenever in doubt.
Safety Alert: Factors that Reduce Hand Hygiene Effectiveness
Clinical Tip
Proper hand hygiene technique and use of products can decrease the risk of skin irritation and dermatitis (PIDAC, 2014). Ensure that you assess your hands, follow the facility hand hygiene protocols and hand-care policies to maintain healthy skin integrity of your hands. ABHR is less irritating to hands and should be used when hands are not visibly soiled or contraindicated according to the client’s diagnosis.
Types of Hand Hygiene
There are two methods of hand hygiene commonly used in the healthcare setting: hand hygiene with an ABHR and hand hygiene with soap and water (PIDAC, 2014).
Alcohol-Based Hand Rub |
Soap and Water |
Preferred method when hands are not visibly soiled (e.g., blood, body fluids, waste). |
Preferred method when hands visibly soiled, to remove organic matter. |
Takes less time. |
Performed with suspected or confirmed diagnosis of C. difficile, norovirus, and Bacillus anthraces. |
More effective. |
Takes more time. |
Less drying and irritating to hands. |
Washing, rubbing, rinsing, and drying actions remove most transient bacteria. |
Rubbing action is important to remove and kill transient bacteria. |
Harsher on hands and increases risk of skin breakdown. |
ABHR products, soap dispensers, and hand washing sinks should be accessible at the point of care and placed in convenient locations for healthcare providers and visitors to use before and after client contact (PIDAC, 2012).
 |
 |
Clinical Tip
Role-model effective hand hygiene practice by performing hand hygiene in front of clients and their visitors prior to and after care to initiate a trusting relationship. Being responsible in maintaining an infection-free environment demonstrates respect and accountability in client care. Encourage and support clients and their visitors to also practice hand hygiene.
Digital Story with Kendra Allen
Test your Knowledge
Attribution
This page was remixed with our own original content and adapted from:
Clinical Procedures for Safer Patient Care — Thompson Rivers University Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon is used under a CC BY 4.0 Licence. This book is an adaptation of Clinical Procedures of Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, which is under a CC BY 4.0 Licence. A full list of changes and additions made by Renée Anderson can be found in the About the Book section.
Physical Examination Techniques: A Nurse’s Guide by Jennifer Lapum, Michelle Hughes, Oona St-Amant, Wendy Garcia, Margaret Verkuyl, Paul Petrie, Frances Dimaranan, Mahidhar Pemasani, and Nada Savicevic is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, except where otherwise noted.

