Airborne Precautions
Airborne precautions are used in addition to routine practices for clients who are known to have or are suspected of having an illness that is transmitted by small droplet nuclei that may stay suspended in the air and be inhaled by others. These particles can remain infectious for a long period of time when spread through the air.
Types of organisms in this category include tuberculosis (TB), measles, chickenpox (varicella), disseminated zoster, and severe acute respiratory syndrome (SARS).
Risk assessment for airborne microorganisms includes:
- Strict adherence to hand hygiene. Hand hygiene: before, during, and after care as needed.
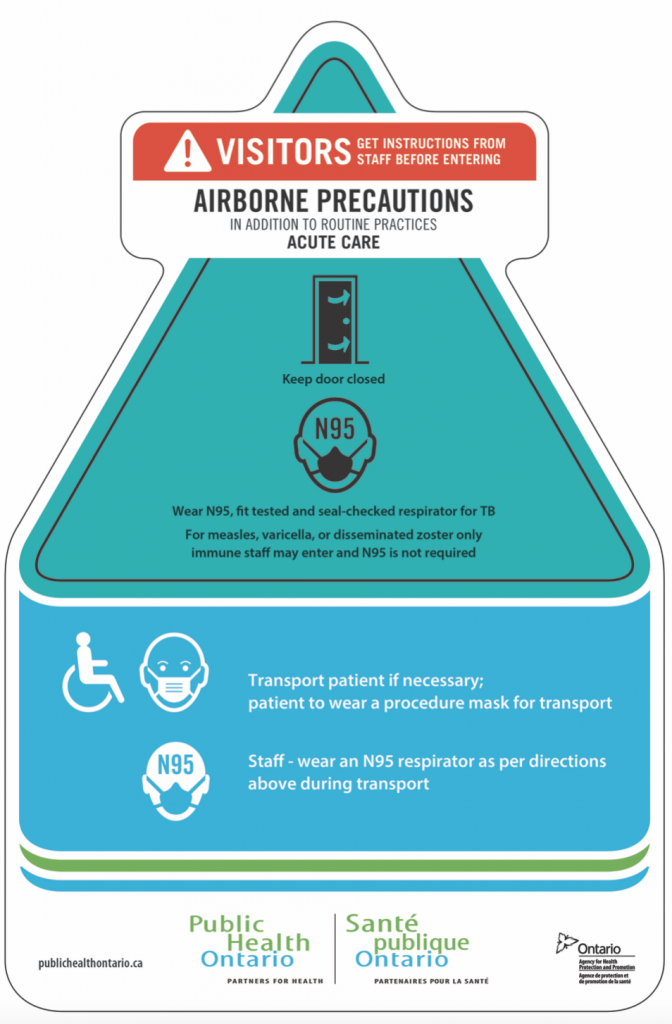
- N95 respirator is required prior to entering the room. Must remove N95 respirator after exiting the room.
- No immunocompromised persons can enter the room. Healthcare providers should know their vaccine status and have current vaccines.
- The client must have a negative pressure room with their own dedicated equipment. The door needs to be kept closed whether or not the client is in the room. The room should have bathroom facilities and be a single room, preferably one that is under negative pressure. If a negative pressure room is unavailable, refer to your healthcare setting policies to determine whether a transfer to another facility is mandated.
- Clean the environment daily and more frequently in high-touch areas. Protocols related to negative pressure rooms must be followed.
- Is the proper airborne-additional precaution sign on the door?
Points of Consideration: Negative Pressure Rooms
A negative pressure room is constructed with a special ventilation design that restricts and limits the spread of airborne microorganisms from the client’s room to the surrounding unit and healthcare setting through a pressurized system. The air pressure inside the room is lower than the air pressure outside the room. Due to this pressure system, which needs to be monitored, when the door opens, the airborne microorganisms in the room will not flow outside of the room and into the surrounding environment. Instead, the airborne microorganisms are sucked into a specialized engineered exhaust system that filters the air (e.g., with HEPA filters) before it is pushed outside of the healthcare facility (PIDAC, 2018).
When providing care to clients on airborne precautions, the door of a negative pressure room should always be closed to maintain the lower pressure inside the room. Some negative pressure rooms have an anteroom, which is a smaller entry room attached to the negative pressure room for healthcare providers to put on and remove PPE prior to entering the client’s room or prior to entering the healthcare unit. Review and follow the healthcare facility policies regarding negative pressure rooms and guidelines for airborne precautions.
If a healthcare facility does not have a negative pressure room, it is recommended the client is moved to a single room and should wear a mask at all times, if capable. However, some healthcare settings cohort clients with COVID-19 depending on room availability and client presentation. Clients do not need to wear a N95 mask. When possible, the client should be moved to another facility that has a negative pressure room available. (PIDAC, 2012).
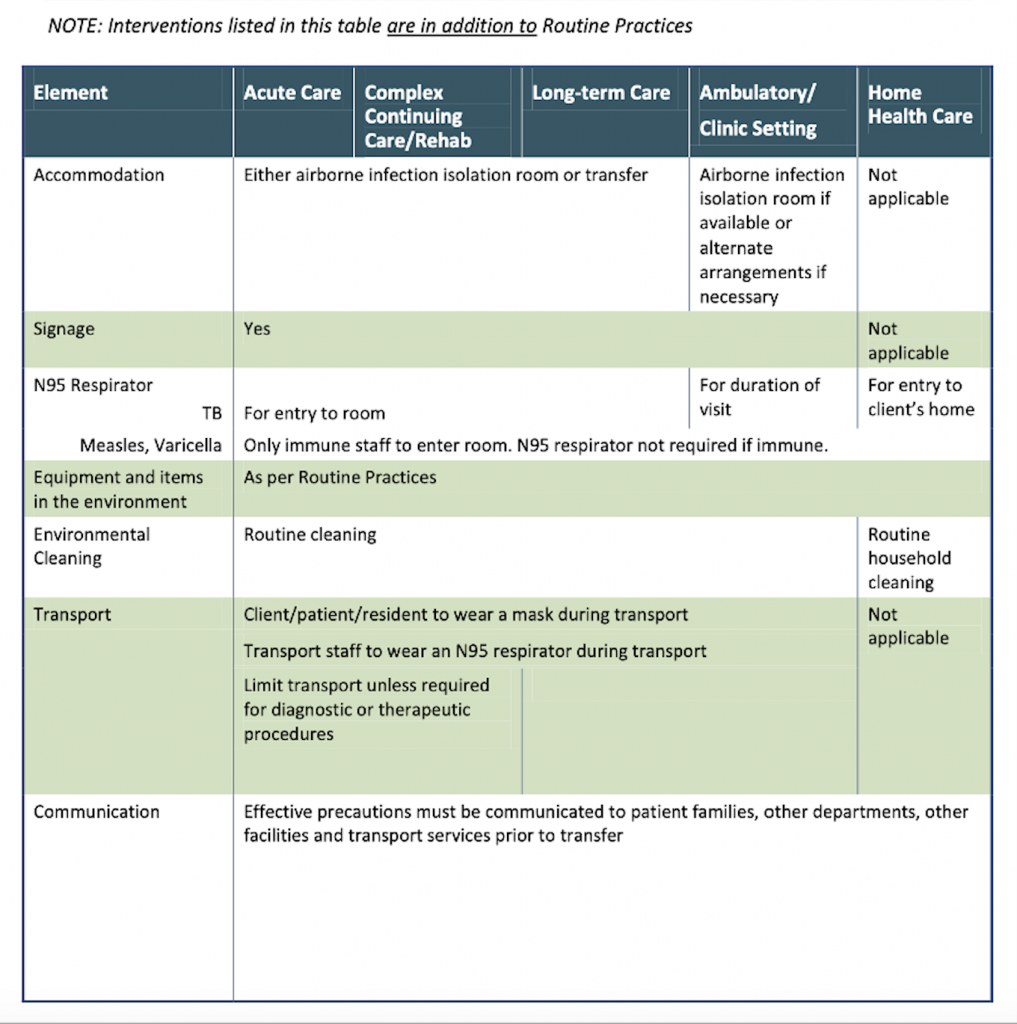
To prevent the transmission of airborne-precaution microorganisms, it is important to follow routines practices and the additional precautions outlined in the following tables by Public Health Ontario (PIDAC, 2012):
Test your Knowledge
Attribution
This page was remixed with our own original content and adapted from:
Clinical Procedures for Safer Patient Care — Thompson Rivers University Edition by Renée Anderson, Glynda Rees Doyle, and Jodie Anita McCutcheon is used under a CC BY 4.0 Licence. This book is an adaptation of Clinical Procedures of Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, which is under a CC BY 4.0 Licence. A full list of changes and additions made by Renée Anderson can be found in the About the Book section.

