37 8.3: Novel Treatment Methods Following a Radical Cystectomy
Adipose-derived Stem Cells and Therapeutic Use
With respect to stem cell therapies, adipose-derived stem cells (ASCs) exist as an autologous, multipotent mesenchymal stem cell source that can be easily, inexpensively, and non-invasively obtained. Most techniques for stem-cell based therapies call for ASCs mainly because they can be harvested with higher yields than other cell types making them particularly ideal for in vitro studies (Maj et al. 1). Additionally, studies have characterized ASCs with low immunogenicity and immunosuppressive properties (Patrikoski et al. 1221). This means that they serve as an excellent cell line source for immunomodulation therapies that aim to alter the immune response to a desired level. Allogeneic stem cell treatments often also choose ASCs, especially in in vivo studies, because genetically dissimilar and hence immunologically incompatible transplant hosts are not burdened by a humoral or cell-mediated immune response. It has been widely accepted that ASCs secrete a wide variety of soluble mediators in growth medium. This conditioned medium, when introduced to a different cell line, promotes cell and hence tissue regeneration. In many cases this can be shown to also restore tissue and organ functional defects (Maj et al. 1). However, ‘different cell lines’ is inclusive of carcinoma cells. The secretion of paracrine factors by ASCs can activate cell proliferative, migratory and invasive regulatory pathways in a similar manner in tumour-initiating cells to potentially progress cancer growth, metastases, and/or trigger recurrence (Maj et al. 1). Limited understanding of the efficacy of this particular mesenchymal cell type in oncological patients who are considering stem cell therapies for tissue engineering after surgery with chemotherapy is of significant concern.
Tissue Engineering
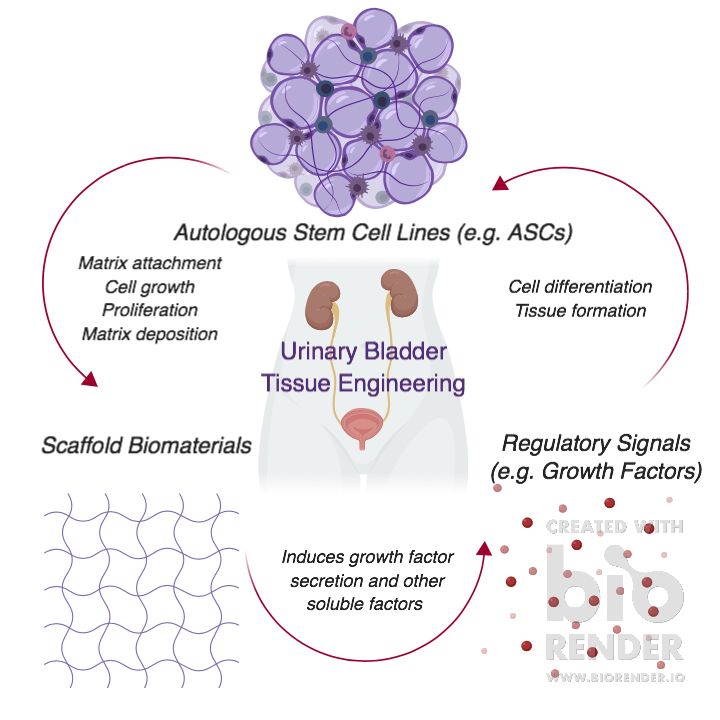
Tissue engineering is synonymous with the broader concept field of regenerative medicine and the use of stem cells in complex and often chronic diseases and conditions. The basics of tissue engineering is a three-fold consideration of 1) the autologous, allogeneic biological stem cells that must attach and migrate into a scaffold that will support cell growth and proliferation once deposited in the matrix; 2) the physical biomaterials like polymers that create the scaffold for the cells and facilitate growth factor delivery; and 3) the regulatory chemical signals of growth and mechanical stimuli that induce cell differentiation and tissue formation (Howard et al. 66). The range of biological cell sources suitable for these cell-seeded matrices that become tissue-engineered grafts for transplantation generally include embryonic stem cells, bone marrow stem cells, cord-derived mesenchymal stem cells (Howard et al.66). In site-specific instances, custom scaffolds for bladder wall substitution, for example, may employ bladder epithelial cells, smooth muscle cells, adipose-derived stem cells, and urine-derived stem cells (Maj et al. 1).
In the field of reconstructive urology, scaffold transplant to tissue voids after a radical cystectomy have been proven to effectively provide the necessary structural support, growth factors, and cells needed for cell viability and tissue engineering. In vivo studies using rat models have demonstrated ASCs with normal, non-cancerous bladder cells in acellular matrices to have morphological regeneration of bladder smooth muscle and nerve as well as bladder capacity (Zhe et al. 412). The latter property means the host can benefit from maintaining what is now lower storage pressure of urine within the bladder. Even with introducing novel scaffold designs such as autologous myofibroblast-silk fibroin structures that create a bag-like structure for improved ASC survival in presence of urine have demonstrated improved morphological regeneration and bladder urinary function (Wang et al. 8; Zhe et al. 410). Similar findings have been delineated with canine models to support the reconstructive effects with potential clinical applications (Hou et al. 7).
On the oncological front, these results are both positive and positively unclear. Results for cancer cell viability have been demonstrated in vitro with human adipose-derived stem cells, the conditioned medium they produce, and specific bladder carcinoma cell lines of various malignancies and different source genders (Maj et al. 10). Proliferation, migration and invasion of cancer cells can occur significantly. Thus, the outcome of tissue engineering in urinary bladder regeneration is not only dependent on the cells to survive, proliferate, and regenerate, they must also not induce recurrence or trigger tumour-initiating cells to metastasize.
Figure 9. An overview of tissue engineering and it’s components. Under CC by 4.0.
Biomarkers of Efficacy
Secretion of soluble growth factors in the scaffold act as signalling molecules on growth factor receptors (GFRs) found on the plasma membrane of cell lines of interest. The receptors activate two specific pathways of interest in tissue regeneration by phosphorylation at the kinase domains. Activation of transcriptional activity of proteins that promote growth through the PI3K/AKT/mTOR signalling pathway or repress apoptosis via the GRB2/MEK/ERK1/2 pathways are valid means of measuring cell proliferation and viability of normal cells for tissue regeneration. ERK1/2 are also responsible for regulating epithelial-to-mesenchymal transition (EMT) that promotes migration when the protein is phosphorylated. These pathway activities can be measured via an InstatELISA Array for total and phosphorylated-AKT and total ERK and phosphorylated-ERK (Read the Did you know? box).
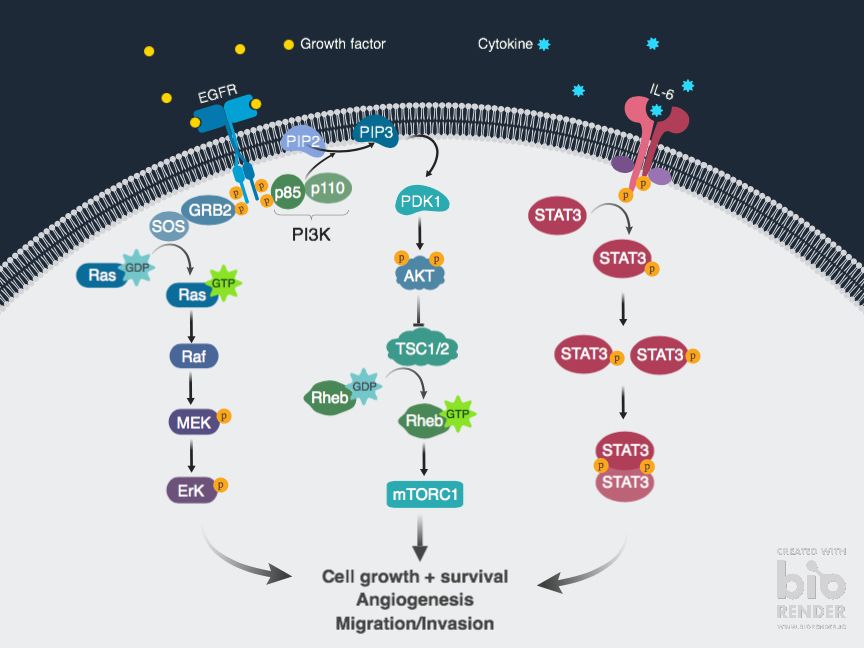
Figure 10. Mechanistic outline of PI3K/AKT/mTOR and GRB2/MEK/ERK 1/2 signalling pathways for both normal and carcinomic bladder cells using only the EGFR as an example. IL-6 has been included in the diagram to represent one of several proinflammatory cytokines measured for involvement in urinary bladder tumorigenesis. Figure made in Biorender.
Inside of the cell, quantification of bladder cells (BC) in the S-phase (i.e. DNA synthesis) via reverse transcription-PCR (RT-qPCR) is one way of measuring cell proliferation. Upregulations in specific immunological protein levels such as IL-6 and IL-8 can be identified via ELISArray techniques on ASC-BC co-cultures (Maj et al. 2). These soluble factors are not only necessary for matrix formation but also continue to demonstrate cell viability. Alternatively, a more direct approach would be to assess metabolic activity with either an alamarBlue assay or an MTT assay. The latter assay, for example, converts water soluble MTT compound to insoluble formazan crystals after incubation to demonstrate said viability. The same techniques may be used for ASCs co-cultured with bladder carcinoma cells to determine the extent of concern for their viability and proliferative capacity. Histological analysis of homogeneous collagen bundles, myofibroblasts, mesothelial cells, smooth muscle cells (SMCs), and nerve cells inside and on the surface of the scaffold for in vivo models can be used to demonstrate augmentation (Zhe et al. 405). Immunofluorescence analysis of these samples is important to demonstrate transdifferentiation.
Outside of the cell in the extracellular matrix (ECM), the focus for efficacy is the interplay between ECM adhesion, migration, and invasion. The first property is marked by specific ECM protein expression levels measured via an ECM Cell Adhesion Array Kit, for example. ECM components include collagen I, collagen II, collagen IV, fibronectin, laminin, tenascin, vitronectin, and β-catenin which regulates the components upstream (Maj et al. 11). Higher OD values with increased absorbance will indicate increased adhesion in non-cancerous bladder cells but the opposite, proportional trend will be seen in bladder cancer cells (BCCs). By effect, decreased migration and invasion will be measured via QCM Chemotaxis Cell Migration and QCM ECMatrix Cell Invasion Assays for normal bladder cells. Likewise, the increase of migratory and invasive cells will be measured in cancerous cell lines.
Advantages and Limitations of Tissue Engineering in the Literature
The efficacy of tissue engineering as a treatment is still being reviewed. An advantage of many studies is the importance placed on maintaining stem cell viability by modifying scaffold material and thus shape to withstand the environment of the transplant site. The novel bag-shaped scaffold used in Wang et al. study is an example of overcoming stem cell sensitivity to urine which is especially important when using ASCs because continuous secretion of growth factors from a viable cell is needed (Wang et al. 8; Zhe et al. 410).
With bladder cancer cells, studies like the one from Maj et al. recognize that specific use of adipose stem cells in conditioned medium on bladder cancer cells is ideal for both their in vitro and future in vivo studies for a couple reasons. First, low immunogenicity means humoral or cell-mediated immune response will not occur. This makes ASCs ideal for either study design and lower variability is observed in the result. Second, by using a single cell line source of ASCs, varying upregulation levels of different proteins is not observed and the study can maintain consistency this way. However, this means their in vitro study in particular is limited by not co-culture conditioning multiple source tissues for adipose-derived stem cells (ASCs) such that the cells reflect cell population behavior.
The Maj et al. study is also burdened by the fact that in in vivo studies, even with some biokinetic differences, the results extrapolated for clinical testing in humans carry more confidence than culture dishes. The study does not indicate whether the ASCs are viscerally or subcutaneously derived. The importance of this detail is in the variability of the soluble factors secreted. Without the cell line interacting with a living model, there is an area of uncertainty as to how the data should be interpreted. As a result, more preclinical investigations that clarify the results in comparison to other studies is warranted. The results given the design limitations mean that we cannot determine how the secreted soluble factors interact with bladder cancer cells at the targeted site which would have otherwise been possible in vivo.
A general emerging and complex limitation of stem cells in cancer therapy is their varying ability to have a significant effect when cells lines are more malignant. While it is good news that ASCs are effective in promoting migration and invasion of certain cells according to some literature, it is important to remind the reader that the cell lines in question are malignant and problematic for the host. On the oncological front, more studies are using cancer cell lines that do not appropriately represent and behave like all cancer cell types. This means that the abnormal function is due to a high mutation count following multiple passages of a metastasized and aggressive cell. This muddles our understanding of both in vitro and in vivo studies on stem cell efficacy.
In addition, study designs on tissue engineering with ACS-BCCs are limited by not thoroughly evaluating data for AKT pathway activity which is responsible for cell proliferation. The study by Maj et al., fails to compare phosphorylated AKT to total AKT and likewise for the ERK pathway.
Did you know?
If the total protein levels are the same but phosphorylation goes up then kinase activity is being regulated. If both total and phosphorylated protein levels go up then the pathway is being regulated at the transcriptional level.
Test Your Knowledge!
- What are the advantages and disadvantages of adipose-derived stem cells?
- What are the three basic considerations for tissue-engineering?
- What are the three main growth factors involved in tumour proliferation for bladder cancer?
- What is the main disadvantage of tissue-engineering?
