35 8.1: Overview of Bladder Cancer
After reading this chapter, you will be able to:
- Describe the diagnosis, prognosis, and recurrence risk of urinary bladder cancer
- Explain the importance of novel advancements in treatment compared to current approaches to bladder cancer therapy
- List the multiple factors that go into designing tissue regeneration
- Discuss the role of stem cells and how application efficacy may be experimentally measured
- Identify the gaps in the experimental field of tissue engineering
Definition and Incidence
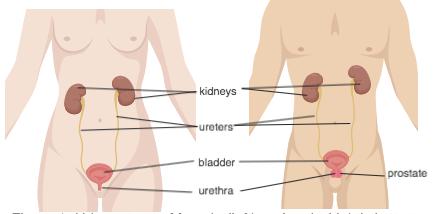
The bladder is a hollow organ with flexible muscular walls (Fig. 1). It functions in the urinary system as a place for urine storage until excretion. Bladder cancer (BC) occurs when cells lining this organ undergo changes that allow them to grow without control and can even have potential to spread to other parts of the body.
Bladder cancer is the ninth most common cancer throughout the world (Sanli et al.). This cancer occurs more often in males than females, but mortality rates is higher in females (Sanli et al.). The incidence rates rise with age and greatly varies among countries mainly because of exposure to different risk factors. The highest rates are observed in Europe, North America, Northern Africa and Western Asia, and the World Health Organization (WHO) estimates a twofold increase in the number of BC incidents in the future (Antoni et al.).
Causes and Risk Factors
As it occurs with the majority of cancers, it is difficult to identify with precision what causes the development of bladder cancer, but it can be connected to different risk factors (Bladder Cancer). In general terms, these factors can be divided in genetic and environmental.
1. Genetic Factors
These include familiar history, genetic polymorphisms and mutations in different genes.
- Familiar history – Having first degree relatives can increase the chance of getting bladder cancer but it is unusual to be inherited in families (Kim 22).
- Genetic polymorphisms – many polymorphisms are related with bladder cancer development, which at the same time affect the vulnerability to different environmental exposures (e.g. carcinogens). This also explains the difference of BC incidence between different races, white having the higher risk (Kim 22).
- Genetic mutations – mutations in different genes that are important in the regulation of normal cell division but when mutated can give rise to BC include tumor suppressor genes like p53, RB, TSG and p21 Ras oncogene (Kim 22).
2. Environmental Factors
- Exposure to chemicals – this group includes chemicals used for the production of paper, rope, dyes, fabrics as well as aromatic amines, arsenic, nitrites and nitrates (Kim 23).
- Smoking – This is considered the main risk factor for BC because the chemicals from smoking are processed in the body and some portion is eliminated through urine, so the bladder is exposed to these chemicals that can cause injure it over time.
- Infection and inflammation – chronic inflammation or recurrent infections in the urinary tract, can also be associated with increased risk in developing BC.
- Previous cancer therapy – treatment with either chemotherapy or radiation could induce BC. A chemotherapeutic drug called cyclophosphamide has been associated with BC (“Bladder Cancer – Symptoms and Causes”). Radiation for cancer treatment in women in the zone of the pelvis also increments the risk to develop BC.
Types of Carcinomas
Bladder cancer usually initiates in the urothelium which is a transitional epithelium lining the bladder. It is important to group BC into different types because this can help to decide the best therapeutic method to treat a patient. There is a big classification of BC but the main 3 types are:
- Urothelial carcinoma – also called transitional cell carcinoma. It starts in the urothelial or transitional cells which are found lining the internal layer of the bladder and these cells are important for the expansion and contraction of the bladder. This is the most frequent form of BC (“Bladder Cancer – Symptoms and Causes”).
- Squamous cell carcinoma – this type can be developed after a chronic inflammation or infection or from the use of catheters over long period of time (Kim 165). This carcinoma presents an ulcerated look. This form of cancer is more often seen in some areas of the world where infections are caused by parasites.
- Adenocarcinoma – this type of BC is not very common. The cells that are first affected in this BC type are the glandular cells responsible for the secretion of mucus in the bladder (“Bladder Cancer”).
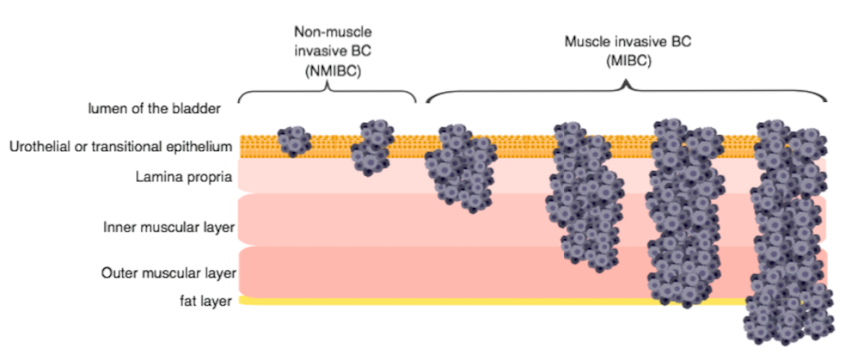
In addition, another way of determining tumor invasion is used, depending on whether the tumor is invading or not the muscular layer of the bladder. This can be either muscle invasive bladder cancer (MIBC) or non-muscle invasive bladder cancer (NMIBC). MIBC have the potential to spread to other areas of the body causing metastasis. (Fig. 2)
Signs and Symptoms of Bladder Cancer
Symptoms and signs can help in the early detection of bladder cancer which can be useful for determining a proper and effective treatment. Some of the symptoms presented during BC are:
- Hematuria or blood present in urine is the main symptom of BC
- Pain when urinate
- Urination can be more frequent and urgent.
- Pain in pelvic area or abdominal area
- Pain in the back
Diagnosis and Staging
For the diagnosis of BC some techniques have been used, including urine cytology, cystoscopy, CT urography, and biopsy.
- Urine cytology – a sample of urine is taken to be examined with a microscope. This test is used to reveal the cells present in urine which includes searching for cancerous cells (Kim 68).
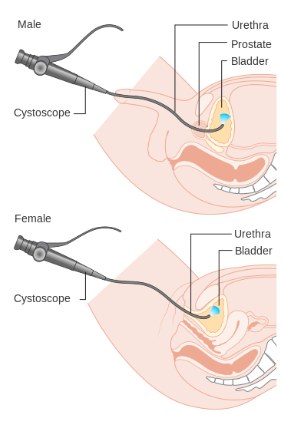
- Cystoscopy – this is considered the main method for BC diagnosis. During this procedure, the physician introduces a small tube through the urethra. This tube contains a camera for internal visualization of the bladder and in this way, abnormalities and presence of tumors can be detected. (Fig. 3)
- CT urography – it is an imaging technique where a dye is applied intravenously for contrast which allows to visualize the urinary tract and helps to detect zones where cancer can be present (“Bladder Cancer – Diagnosis and treatment”).
- Biopsy – where a tissue sample is collected from the bladder to analyze and detect for the presence of cancer.
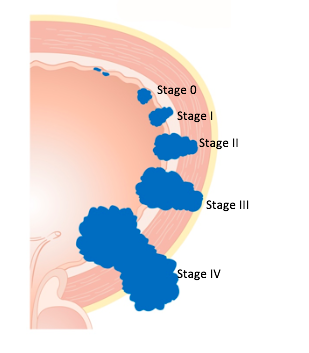
All these techniques used for diagnosis are essential for the later characterization of the stage of the bladder cancer for prognosis and treatment. For guiding, doctors use 5 stages which includes stage 0 to IV. (Fig. 4)
- Stage 0 – indicates an early form of cancer where the cells are localized lining the bladder.
- Stage I – the cancer has propagated to the next layer which is the lamina propria.
- Stage II – the cancer has advanced into the muscular layer of the bladder becoming a muscle-invasive bladder cancer (MIBC).
- Stage III – cancer has invaded other fat tissues surrounding the bladder.
- Stage IV – organs that are close to the bladder are now affected because the cancer has extended and can even spread through the lymph nodes or cause metastasis.
Recurrence Risk
Although the rates of mortality in BC patients is not extensive, the rates of BC recurrence are very high. According to the Canadian Cancer Society, around 70% of BC patients will have reappearance of BC (“Prognosis and Survival for Bladder Cancer – Canadian Cancer Society”). Thus, in order to is important to keep a constant surveillance after treatment in order to prevent progression of cancer in case of recurrence.
Test Your Knowledge!
- What are the main risk factors associated with bladder cancer?
- What are the three types of bladder cancer?
- What are the five signs and symptoms of bladder cancer?
- What are the four techniques used in the diagnosis of bladder cancer?
