3.1 The Effects of Exercise on the Cardiovascular System
Despite an individual’s race, sex or age, it has been found that exercise and lifestyle physical activity (structured or non-structured) might protect against the progress of CVD and improve physical and physiological function (Ozemek et al.). Cardiovascular disease (CVD) has been estimated to cause up to 40% of all deaths globally by 2020. Increasing physical exercise from childhood is an important way to control for risk factors associated with CVD as they begin to develop in individuals during that age. It is recommended by public health authorities for children and youth to exercise daily for a minimum of 60 minutes daily to prevent the increase of CVD risk factors and help delay the onset of cardiac-related diseases (Costa-Pereira et al.). For people who already suffer from CVDs, exercise is known to be an important intervention which reduces the risk for recurrence of cardiac-related incidents by reducing blood pressure levels and help prove lipid profile (Veldhuijzen van Zanten et al.).
Metabolic syndrome which is a cluster of pathological conditions such as obesity, hypertension etc., is also closely associated with developing high-risk CVD (Kra ̈nkel et al.). The metabolic inflammation processes are strongly influenced by an individual’s genetic, epigenetics, surrounding environment and personal lifestyle choices which predisposes them in developing CVD. However, both endurance and resistance exercise training (ET) targets specific physiological parameters such as glucose levels, lipid profile and has anti-inflammatory effects alongside overall physical fitness improvements. Furthermore, beneficial outcomes from exercise on the vascular system are well documented as it improves vascular function. The stress induced by exercise causes structural changes in the vascular walls in addition to altering signaling pathways and inflammatory processes connected with vascular function profile (Veldhuijzen van Zanten et al.).
Moreover, heart failure (HF) is a life-threatening condition which is caused by ischemic cardiac diseases and is linked with the loss of cardiomyocytes (Shen et al.). ET is highly encouraged in patients suffering from HF because of its beneficial effects on functional capacity (Adamopoulos et al.).However, HF patients have reduced exercise capabilities due to dysfunctional changes in their cardiovascular and respiratory systems. Moreover, during peak exercise performance, there is 4 to 6-fold increase in CO and the ability to increase CO in response to exercise is a key regulatory factor for the cardiovascular system. However, in response to exercise-induced stress, HF patients cannot increase CO levels sufficiently due to impaired myocardial contractility, hypoxia and muscular ineffectiveness (Adamopoulos et al.). Although the mechanism remains unknown, the heart is capable of limited, endogenous regenerative capacity, thus there is increased interest in the field of cardiac regeneration particularly after a cardiac injury.
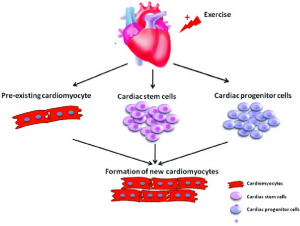
Myocardial infarction (MI) can destroy billions of cardiomyocytes in a few hours and can activate a severe inflammatory response (Shen et al.). The adult mammalian heart has limited regenerative properties, thus self-repair mechanisms in the ischemic myocardium predominantly relate to the formation of collagen-rich scars. This can progressively cause fibrosis of cardiac tissue, the development of ventricular modeling and ultimately heart failure (Shen et al.). As the heart cannot compensate for the loss of all cardiomyocytes, techniques enhancing cardiac endogenous regenerative abilities can help discover new therapeutic strategies for HF treatment. Several studies have indicated exercise may potentially lead to the generation of new cardiomyocytes by stimulating resident cardiac stem cells (CSCs) and progenitor cells (CPCs). There is cardiac growth by both cardiomyocyte hypertrophy (increase in cell size) and hyperplasia (increase in cell number) (Shen et al.).
