4.3 – Cellular Therapy Using Mesenchymal Stem Cells
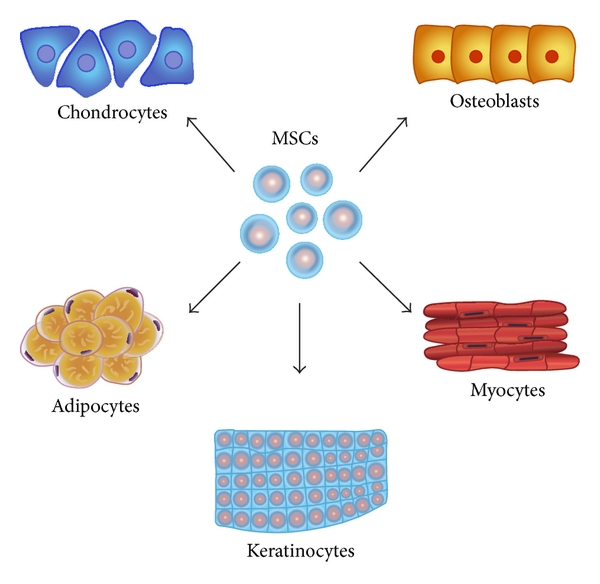
In exploring the treatment options for Inflammatory Bowel Disease, iPSCs may be a useful method of cellular therapy due to its ability to differentiate into mesenchymal stem cells (MSCs). MSCs are multipotent stem cells that are able to differentiate into various cell types including osteoblasts, adipocytes and chondrocytes. They are the targets for new therapeutic treatment of IBD because they are able to modulate the immune system by suppressing the activity of different inflammatory pathways (Chow et al., 2017). It is shown that adult MSCs can suppress T cell activation, proliferation and secretion of cytokines. More recently, studies show that systemic injection of MSCs is able to reduce intestinal inflammation in mouse models (Liang et al.,2011). Additionally, humans treated with cellular therapy for CD and UC have observed similar results where intestinal inflammation was reduced. With this amount of evidence, treating individuals with IBD through MSCs seems plausible.
Although the use of MSCs for IBD treatment seems promising, their use as a feasible therapeutic option remains questionable due to current limitations associated with this treatment. One of the major limitations is how MSCs are sourced. Currently, is it not clear whether an allogenic or autologous source of MSC has an effect on the efficacy of the treatment (Swenson & Theise, 2011). Autologous MSCs are derived from the individual itself whereas allogenic MSCs are derived from another individual. Some studies suggest that the source does not have immune rejection while other studies show contradicting evidence. Other studies suggest that the donor age of MSCs also has an effect on the efficacy of treatment. Cells from older donors have reduced capability of supporting vascular formation and wound healing (Duscher et al.,2014). Additionally, variability in MSCs between donors have impacts on the consistency of treatment. Donors with type O blood have MSCs with greater potential for proliferation and self renewal (Nitkin & Bonfield, 2017). Furthermore, unknown genetic factors of treatment recipients may impact the efficacy of treatment.
To address the various limitations involved with the uniform sourcing of the MSCs, a viable solution is to derive MSCs from induced pluripotent stem cells (iPSCs). Previous studies show that iPSC derived MSCs functionally and phenotypically resemble bone marrow and adipose-tissue derived MSCs. Therefore MSCs derived from iPSC (called iMSCs) can potentially be a more sustainable and uniform source of treatment.
KEY TAKEAWAYS
- MSCs are the targets for new therapeutic treatment of IBD because they are able to modulate the immune system.
- Their use as a feasible therapeutic option remains questionable due to current limitations such as the source, donor age and MSC variability.
- Previous studies show that iPSC derived MSCs functionally and phenotypically resemble bone marrow and adipose-tissue derived MSCs.
