Promoting Interprofessional Competency in Virtual Simulation
How does the educator promote team/group based interprofessional competencies in virtual simulations?
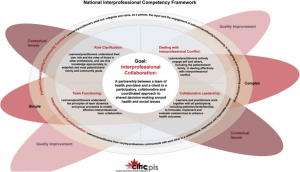
Interprofessional (IP) education is essential to reflect real-world clinical practice. Clinical practice is highly collaborative and team-based, and virtual simulation enactment, when played in small or large groups, is an excellent way to build these competencies. An IP competency framework should be integrated within the virtual simulation curriculum as a way to build on participants’ existing knowledge, values, skills, and attitudes, and to broaden awareness of all scopes of practice within the teams (CIHC, 2010; See Figure 4.3.)
- Select a software program that supports multi-user real-time interaction.
- Consider synchronous and asynchronous enactments.
- Prepare to address negative hierarchy and power differentials that may occur in the simulation to ensure that the participants’ developing role clarity is not impacted.
- Prepare to debunk healthcare professional stereotypes prior to these taking root in the novice practitioner’s own role identity and in their understanding of the role of others.
- When designing the simulation, it’s important to acknowledge all professions that would typically be present for the scenario you are developing. Avoid valuing one profession over another.
Click here to download an Alternative Text Description of Figure 4.3
Figure 4.3: National Interprofessional Competency Framework
Expert’s Corner: Facilitator Tips
Tips & Tricks for Facilitators Enacting Interprofessional Virtual Simulations
Before the Session:
-
Divide interprofessional team members evenly based on their roles into smaller breakout rooms on ZOOM or any other communication platform to increase diversity and representation within rooms.
-
Explore various interprofessional virtual simulation platforms that you can use based on your learning objectives: https://www.sim-one.ca/content/virtual-simulations-virtual-patients
After the Session:
-
Ask interprofessional team members to include or edit their full names and professional titles and/or their assigned roles in the simulation under the ‘Participants List’ on the right side of the ZOOM window at the beginning or during the pre-brief (e.g. John Walsh, RN, Medication Nurse). This provides a shared mental model of the participants and their roles in the simulations.
Credit: Sunayna Vuppal BScN, RN, MN – Simulation Educator at The Hospital for Sick Children
Expert’s Corner: Benefits of Simulation & IP Learning
In this video interview, Dr. David Topps discusses the benefits of virtual simulation and interprofessional learning. Hosted by Treva Job, Simulation Lead, Georgian College.

