8.3 Treatment and Recovery
Before reading the material below watch this video. Marco Badwal, Full-time Researcher Scholar at Harvard University, Ted Talk, January 18, 2019:
The Science of Habits | Marco Badwal | TEDxFS. by TEDx Talks. Marco is currently a full-time research scholar at Harvard University. The aim of the research is to help us to better understand learning and memory. Marco talks about the building and implementation of habits and their benefit to “get a bit better every day”. Marco is an upcoming cognitive neuroscientist from the University of Amsterdam (UvA), health consultant and enthusiastic Crossfitter. The impulse to better understand the human psyche and brain came first through his parents, who are both psychologists, and was later sparked by inspiring authors and researchers, such as Sam Harris.
Transcript
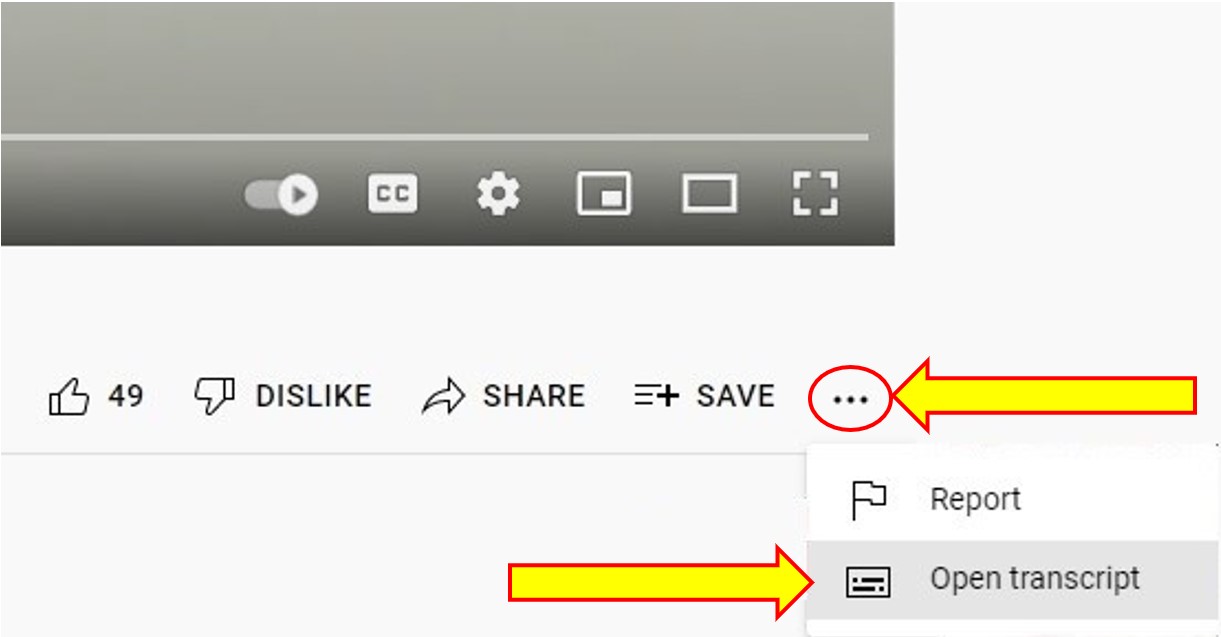
To Access the Video Transcript:
1. Click on “YouTube” on the bottom-right of the video. This will take you directly to the YouTube video.
2. Click on the More Actions icon (represented by three horizontal dots)
3. Click on “Open Transcript”
Can addiction be treated successfully?
Yes, addiction is a treatable disorder. Research on the science of addiction and the treatment of substance use disorders has led to the development of research-based methods that help people to stop using drugs and resume productive lives, also known as being in recovery.
Can addiction be cured?
Like other chronic diseases such as heart disease or asthma, treatment for drug addiction usually isn’t a cure. But addiction can be managed successfully. Treatment enables people to counteract addiction’s disruptive effects on their brain and behaviour and regain control of their lives.
These images showing the density of dopamine transporters in the brain illustrate the brain’s remarkable ability to recover, at least in part, after a long abstinence from drugs—in this case, methamphetamine.
Does relapse to drug use mean treatment has failed?
No. The chronic nature of addiction means that for some people relapse, or a return to drug use after an attempt to stop, can be part of the process, but newer treatments are designed to help with relapse prevention. Relapse rates for drug use are similar to rates for other chronic medical illnesses. If people stop following their medical treatment plan, they are likely to relapse.
Treatment of chronic diseases involves changing deeply rooted behaviours, and relapse doesn’t mean treatment has failed. When a person is recovering from an addiction relapse, it indicates that the person needs to speak with their doctor to resume treatment, modify it, or try another treatment.
Relapse rates for people treated for substance use disorders are compared with those for people treated for high blood pressure and asthma. Relapse is common and similar across these illnesses. Therefore, substance use disorders should be treated like any other chronic illness. Relapse serves as a sign for resumed, modified, or new treatment.
While relapse is a normal part of recovery, for some drugs, it can be very dangerous—even deadly. If a person uses as much of the drug as they did before quitting, they can easily overdose because their bodies are no longer adapted to their previous level of drug exposure. An overdose happens when the person uses enough of a drug to produce uncomfortable feelings, life-threatening symptoms, or death.
What are the principles of effective treatment?
Research shows that when treating addictions to opioids (prescription pain relievers or drugs like heroin or fentanyl), medication should be the first line of treatment, usually combined with some form of behavioural therapy or counselling. Medications are also available to help treat addiction to alcohol and nicotine.
Additionally, medications are used to help people detoxify from drugs, although detoxification is not the same as treatment and is not sufficient to help a person recover. Detoxification alone without subsequent treatment generally leads to the resumption of drug use.
For people with addictions to drugs like stimulants or cannabis, no medications are currently available to assist in treatment, so treatment consists of behavioural therapies. Treatment should be tailored to address each patient’s drug use patterns and drug-related medical, mental, and social problems. Discoveries in science lead to breakthroughs in drug use treatment.
What medications and devices help treat drug addiction?
Different types of medications may be useful at different stages of treatment to help a patient stop abusing drugs, stay in treatment, and avoid relapse.
- Treating withdrawal. When patients first stop using drugs, they can experience various physical and emotional symptoms, including restlessness or sleeplessness, as well as depression, anxiety, and other mental health conditions. Certain treatment medications and devices reduce these symptoms, which makes it easier to stop drug use.
- Staying in treatment. Some treatment medications and mobile applications are used to help the brain adapt gradually to the absence of the drug. These treatments act slowly to help prevent drug cravings and have a calming effect on body systems. They can help patients focus on counselling and other psychotherapies related to their drug treatment.
- Preventing relapse. Science has taught us that stress cues linked to drug use (such as people, places, things, and moods), and contact with drugs are the most common triggers for relapse. Scientists have been developing therapies to interfere with these triggers to help patients stay in recovery.
Common medications used to treat drug addiction and withdrawal:
- Opioid
- Methadone
- Buprenorphine
- Suboxone
- Extended-release naltrexone
- Lofexidine
- Nicotine
- Nicotine replacement therapies (available as a patch, inhaler, or gum)
- Bupropion
- Varenicline
- Alcohol
- Naltrexone
- Disulfiram
- Acamprosate
How do behavioural therapies treat drug addiction?

Behavioural therapies help people in drug addiction treatment modify their attitudes and behaviours related to drug use. As a result, patients are able to handle stressful situations and various triggers that might cause another relapse. Behavioural therapies can also enhance the effectiveness of medications and help people remain in treatment longer.
- Aversion therapy is often used to treat problems such as substance abuse and alcoholism. It works by teaching people to associate a stimulus that’s desirable but unhealthy with an extremely unpleasant stimulus
- Cognitive-behavioural therapy seeks to help patients recognize, avoid, and cope with the situations in which they’re most likely to use drugs.
- Cognitive-behavioural play therapy is commonly used with children
- Contingency management uses positive reinforcement such as providing rewards or privileges for remaining drug free, for attending and participating in counselling sessions, or for taking treatment medications as prescribed.
- Family therapy helps people (especially young people) with drug use problems, as well as their families, address influences on drug use patterns and improve overall family functioning.
- Motivational enhancement therapy uses strategies to make the most of people’s readiness to change their behaviour and enter treatment.
- Systems Desensitization relies heavily on classical conditioning
- Twelve-step facilitation (TSF) is an individual therapy typically delivered in 12 weekly sessions to prepare people to become engaged in 12-step mutual support programs. 12-step programs, like Alcoholic Anonymous, are not medical treatments, but provide social and complementary support to those treatments. TSF follows the 12-step themes of acceptance, surrender, and active involvement in recovery.
Self-Help Supports

- Celebrate Recovery is a Christ-centred based 12 step recovery program for anyone struggling with hurt pin or addiction of any kind.
- Families for Addiction Recovery is a support group for Families to assist in the process of healing
- Twelve-step meetings is an individual therapy typically delivered in 12 weekly sessions to prepare people to become engaged in 12-step mutual support programs. 12-step programs, like Alcoholic Anonymous, are not medical treatments, but provide social and complementary support to those treatments. TSF follows the 12-step themes of acceptance, surrender, and active involvement in recovery.
- Smart Recovery (SR) mutual support meetings are free and open to anyone who is seeking
science-based, self-empowered addiction recovery.
How do the best treatment programs help patients recover from addiction?
Stopping drug use is just one part of a long and complex recovery process. When people enter treatment, addiction has often caused serious consequences in their lives, possibly disrupting their health and how they function in their family lives, at work, and in the community.
Because addiction can affect so many aspects of a person’s life, treatment should address the needs of the whole person to be successful. Counsellors may select from a menu of services that meet the specific medical, mental, social, occupational, family, and legal needs of their patients to help in their recovery.
An important piece to remember is that everyone’s substance use and abuse/addiction is individual to each person. This being the case, we need to always be aware that every journey into health & wellness/recovery/treatment is different and so are the pieces that assist in making this a successful experience.
For more information on Canadian Supports
Explore Canadian Treatment Supports
For more information on Drug Treatment
References
Figure 8.3.1 – The Journal of Neuroscience. (2001). Loss of Dopamine Transporters in Methamphetamine Abusers Recovers with Protracted Abstinence [Photograph]. Journal of Neuroscience. https://www.jneurosci.org/content/21/23/9414
The Journal of Neuroscience. (n.d.). The Journal of Neuroscience. Retrieved March 22, 2022, from https://www.jneurosci.org/content/21/23/9414
Tedx Talks. (2019, January 18). The Science of Habits | Marco Badwal | TEDxFS [Video]. YouTube. https://www.youtube.com/watch?v=FSZyzhi8C9o

