8.4 Addiction Treatments and Therapies
Addiction Treatments Past and Present
In the past, society viewed drug addiction as a moral flaw. Popular “treatments” involved imprisonment, sentencing to asylums, and church-guided prayer. Not surprisingly, these methods were generally ineffective. Today we understand that addiction is a brain disease characterized by fundamental and long-lasting changes in the brain. Modern treatments are based on scientific research. Treatment is tailored to the individual and typically involves a combination of drug and behavioural therapy. Today’s methods are very effective, with 40-70% of patients remaining drug-free.
There are many options that have been successful in treating drug addiction, including:
- behavioural counselling
- medication
- medical devices and applications used to treat withdrawal symptoms or deliver skills training
- evaluation and treatment for co-occurring mental health issues such as depression and anxiety
- long-term follow-up to prevent relapse
A range of care with a tailored treatment program and follow-up options can be crucial to success. Treatment should include both medical and mental health services as needed. Follow-up care may include community- or family-based recovery support systems.
This video provides a brief overview of the treatments covered in this chapter:
Recovery Options: Treatment for Drug Addiction and Alcoholism. by Carrier Clinic. 12-steps, AA, NA, S.M.A.R.T., detox, rehab, and other options for addiction treatment are discussed.
Transcript
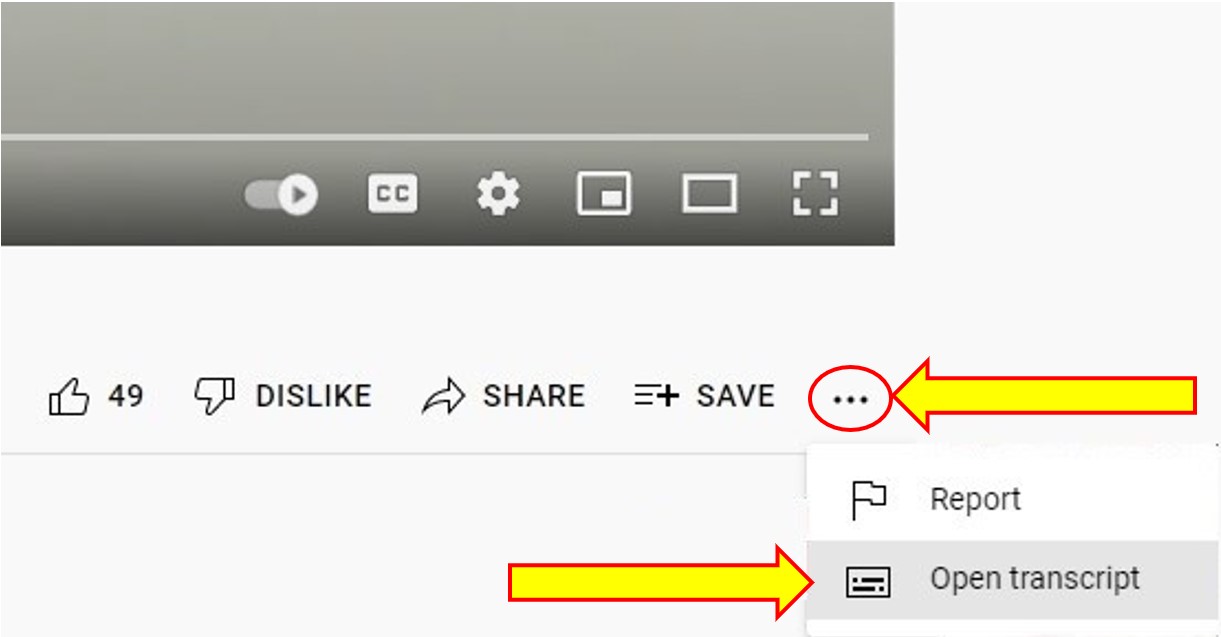
To Access the Video Transcript:
1. Click on “YouTube” on the bottom-right of the video. This will take you directly to the YouTube video.
2. Click on the More Actions icon (represented by three horizontal dots)
3. Click on “Open Transcript”
How are medications and devices used in drug addiction treatment?
Medications and devices can be used to manage withdrawal symptoms, prevent relapse, and treat co-occurring conditions.
Withdrawal. Medications and devices can help suppress withdrawal symptoms during detoxification. Detoxification is not in itself “treatment,” but only the first step in the process. Patients who do not receive any further treatment after detoxification usually resume their drug use. One study of treatment facilities found that medications were used in almost 80 percent of detoxifications (SAMHSA, 2014).
Harm Reduction. Medications and devices are sometimes needed to assist in reducing harm for an extended period. The will assist by suppress withdrawal symptoms for an extended period of time. Detoxification is not in itself “treatment,” but only the first step in the process. Patients who receive Harm Reduction support have a higher success rate for treatment.
Relapse prevention. Patients can use medications to help re-establish normal brain function and decrease cravings. Medications are available for the treatment of opioid (heroin, prescription pain relievers), tobacco (nicotine), and alcohol addiction. Scientists are developing other medications to treat stimulant (cocaine, methamphetamine) and cannabis (marijuana) addiction. People who use more than one drug, which is very common, need treatment for all of the substances they use.
- Opioids: Methadone (Dolophine®, Methadose®), buprenorphine (Suboxone®, Subutex®, Probuphine®, Sublocade™), and naltrexone (Vivitrol®) are used to treat opioid addiction. Acting on the same targets in the brain as heroin and morphine, methadone and buprenorphine suppress withdrawal symptoms and relieve cravings. Naltrexone blocks the effects of opioids at their receptor sites in the brain and should be used only in patients who have already been detoxified. All medications help patients reduce drug seeking and related criminal behaviour and help them become more open to behavioural treatments. A NIDA study found that once treatment is initiated, both a buprenorphine/naloxone combination and an extended-release naltrexone formulation are similarly effective in treating opioid addiction. Because full detoxification is necessary for treatment with naloxone, initiating treatment among active users was difficult, but once detoxification was complete, both medications had similar effectiveness.
- Tobacco: Nicotine replacement therapies have several forms, including the patch, spray, gum, and lozenges. These products are available over the counter. The U.S. and Canada have approved two prescription medications for nicotine addiction: bupropion (Zyban®) and varenicline (Chantix®). They work differently in the brain, but both help prevent relapse in people trying to quit. The medications are more effective when combined with behavioural treatments, such as group and individual therapy as well as telephone quit-lines.
- Alcohol: Three medications have been FDA-approved for treating alcohol addiction and a fourth, topiramate, has shown promise in clinical trials (large-scale studies with people). The three approved medications are as follows:
- Naltrexone blocks opioid receptors that are involved in the rewarding effects of drinking and in the craving for alcohol. It reduces relapse to heavy drinking and is highly effective in some patients. Genetic differences may affect how well the drug works in certain patients.
- Acamprosate (Campral®) may reduce symptoms of long-lasting withdrawal, such as insomnia, anxiety, restlessness, and dysphoria (generally feeling unwell or unhappy). It may be more effective in patients with severe addiction.
- Disulfiram (Antabuse®) interferes with the breakdown of alcohol. Acetaldehyde builds up in the body, leading to unpleasant reactions that include flushing (warmth and redness in the face), nausea, and irregular heartbeat if the patient drinks alcohol. Compliance (taking the drug as prescribed) can be a problem, but it may help patients who are highly motivated to quit drinking.
- Co-occurring conditions: Other medications are available to treat possible mental health conditions, such as depression or anxiety, that may be contributing to the person’s addiction.
The Controversy of Maintenance and Medication

When we use medication or maintenance to treat drug addiction are we just replacing one drug with another? Does the addict simply become addicted to a legal drug? No. With pharmaceutical substance-abuse treatment, the user can begin to function normally again and stop the cravings. Using drugs to treat cravings and prevent relapse buys crucial time for behavioural and cognitive therapies to begin working.
Maintenance programs are controversial because the treatments are drugs that often have potent, intoxicating effects, and because patients often require continuous treatment, sometimes over many years. The classic example of a maintenance-based drug treatment is methadone or suboxone, taken once a day to suppress heroin withdrawal. This is becoming a more therapeutic maintenance option.
How are behavioural therapies used to treat drug addiction?
Behavioural therapies help patients:
- modify their attitudes and behaviours related to drug use
- increase healthy life skills
- persist with other forms of treatment, such as medication
Patients can receive treatment in many different settings with various approaches.
Outpatient behavioural treatment includes a wide variety of programs for patients who visit a behavioural health counsellor on a regular schedule. Most of the programs involve individual or group drug counselling, or both. These programs typically offer forms of behavioural therapy such as:
- cognitive-behavioural therapy, which helps patients recognize, avoid, and cope with the situations in which they are most likely to use drugs (*See information below)
- multidimensional family therapy—developed for adolescents with drug abuse problems as well as their families—which addresses a range of influences on their drug abuse patterns and is designed to improve overall family functioning
- motivational interviewing, which makes the most of people’s readiness to change their behaviour and enter treatment
- motivational incentives (contingency management), which uses positive reinforcement to encourage abstinence from drugs
Treatment is sometimes intensive at first, where patients attend multiple outpatient sessions each week. After completing intensive treatment, patients transition to regular outpatient treatment, which meets less often and for fewer hours per week to help sustain their recovery.
In September 2017, the FDA permitted marketing of the first mobile application, reSET®, to help treat substance use disorders. This application is intended to be used with outpatient treatment to treat alcohol, cocaine, marijuana, and stimulant substance use disorders.
There have been many new mobile applications created and available on all mobile devices. The application is intended to give support, autonomy, hope, answers, encouragement, be part of a community, independent and connectivity wherever you are. This of course is in addition to your recovery plan, not the only component of your recovery plan.
Mobile applications to assist in treating Substance Use Disorders, Alcohol and Gambling (Behaviour Addictions):
- Alberta Health News – Addiction and Mental Health Mobile Apps Directory
- New Interactive Risk Assessment Tool Helps People in Canada Assess Their Gambling
- The Best Alcohol Addiction Recovery Apps of 2021
- Smartphone Apps Targeting Alcohol and Illicit Substance Use: Systematic Search in in Commercial App Stores and Critical Content Analysis
- Apps to Help You Cope with Addiction
- Free Sobriety Apps to Boost Your Recovery
Inpatient or residential treatment can also be very effective, especially for those with more severe problems (including co-occurring disorders). Licensed residential treatment facilities offer 24-hour structured and intensive care, including safe housing and medical attention. Residential treatment facilities may use a variety of therapeutic approaches, and they are generally aimed at helping the patient live a drug-free, crime-free lifestyle after treatment. Examples of residential treatment settings include:
- Therapeutic communities, which are highly structured programs in which patients remain at a residence, typically for 6 to 12 months. The entire community, including treatment staff and those in recovery, act as key agents of change, influencing the patient’s attitudes, understanding, and behaviours associated with drug use. Read more about therapeutic communities in the Therapeutic Communities Research Report at https://www.drugabuse.gov/publications/research-reports/therapeutic-communities.
- Shorter-term residential treatment, which typically focuses on detoxification as well as providing initial intensive counselling and preparation for treatment in a community-based setting.
- Recovery housing, which provides supervised, short-term housing for patients, often following other types of inpatient or residential treatment. Recovery housing can help people make the transition to an independent life—for example, helping them learn how to manage finances or seek employment, as well as connecting them to support services in the community.
Behavioural and Cognitive Therapy
Counselling, support groups, and other forms of therapy are crucial to preventing relapse. In order to stay off drugs, addicts must learn new ways of thinking and behaving. Cognitive and behaviour therapy can include such things as learning to:
- Talk openly about personal experiences
- Manage problems without turning to drugs
- Identify and correct problem behaviour
- Identify and correct harmful patterns of thinking
- Recognize drug cravings
- Identify and manage high-risk situations
- Establish motivation to change
- Improve personal relationships
- Develop refusal skills
- Manage time more efficiently
Principles of Effective Treatment
Based on scientific research since the mid-1970s, the following key principles should form the basis of any effective treatment program:
- Addiction is a complex but treatable disease that affects brain function and behaviour.
- No single treatment is right for everyone.
- People need to have quick access to treatment.
- Effective treatment addresses all of the patient’s needs, not just his or her drug use.
- Staying in treatment long enough is critical.
- Counselling and other behavioural therapies are the most commonly used forms of treatment.
- Medications are often an important part of treatment, especially when combined with behavioural therapies.
- Treatment plans must be reviewed often and modified to fit the patient’s changing needs.
- Treatment should address other possible mental disorders.
- Medically assisted detoxification is only the first stage of treatment.
- Treatment doesn’t need to be voluntary to be effective.
- Drug use during treatment must be monitored continuously.
- Treatment programs should test patients for HIV/AIDS, hepatitis B and C, tuberculosis, and other infectious diseases as well as teach them about steps they can take to reduce their risk of these illnesses.
Is treatment different for criminal justice populations?

Scientific research since the mid-1970s shows that drug abuse treatment can help many drug-using offenders change their attitudes, beliefs, and behaviours towards drug abuse; avoid relapse and successfully remove themselves from a life of substance abuse and crime. Many of the principles of treating drug addiction are similar for people within the criminal justice system as for those in the general population. However, many offenders don’t have access to the types of services they need. Treatment that is of poor quality or is not well suited to the needs of offenders may not be effective at reducing drug use and criminal behaviour.
In addition to the general principles of treatment, some considerations specific to offenders include the following:
- Treatment should include the development of specific cognitive skills to help the offender adjust attitudes and beliefs that lead to drug abuse and crime, such as feeling entitled to have things one’s own way or not understanding the consequences of one’s behaviour. This includes skills related to thinking, understanding, learning, and remembering.
- Treatment planning should include tailored services within the correctional facility as well as transition to community-based treatment after release.
- Ongoing coordination between treatment providers and courts or parole and probation officers is important in addressing the complex needs of offenders re-entering society.
- Education in addictions, mental health and strategies as well as counselling.
Key Takeaways
- Drug addiction can be treated, but it’s not simple. Addiction treatment must help the person do the following:
- stop using drugs
- stay drug-free
- be productive in the family, at work, and in society
- Successful treatment has several steps:
- detoxification
- behavioural counselling
- medication (for opioid, tobacco, or alcohol addiction)
- evaluation and treatment for co-occurring mental health issues such as depression and anxiety
- long-term follow-up to prevent relapse
- Medications and devices can be used to manage withdrawal symptoms, prevent relapse, and treat co-occurring conditions.
- Behavioural therapies help patients:
- modify their attitudes and behaviours related to drug use
- increase healthy life skills
- persist with other forms of treatment, such as medication
- People within the criminal justice system may need additional treatment services to treat drug use disorders effectively. However, many offenders don’t have consistent access to the types of services they need.
For More Information:
Type your examples here.
- Research Report on Medications to Treat Opioid Addiction
- Research Report on Therapeutic Communities
- Naloxone – a medication designed to rapidly reverse an opioid overdose
References
CAMH. (n.d.-b). Mental Illness & Addiction Index. Retrieved April 28, 2022, from https://www.camh.ca/en/health-info/mental-illness-and-addiction-index
CAMH. (n.d.-b). Information in Other Languages. Retrieved April 28, 2022, from https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/information-in-other-languages
Carrier Clinic. (2015, January 29). Recovery Options: Treatment for Drug Addiction and Alcoholism [Video]. YouTube. https://www.youtube.com/watch?v=e4D4QUaEp_w
Connex Ontario. (2022). Help in Other Languages. Retrieved February 2, 2022, from https://www.connexontario.ca/other-languages
Poole, N., & Vitalla, K. (n.d.). Substance Use and Indo-Canadian Women. Here to Help. Retrieved April 28, 2022, from https://www.heretohelp.bc.ca/visions-women-vol2/substance-use-and-indo-canadian-women

