3.3 Concurrent Disorders
We all have mental health, like we all have physical health. Our mental health is shaped by many factors, including “our social, economic, and physical environments” (1). It can depend on what we are experiencing at any moment, our ability to cope and our ability to be resilient. Reflect on the reasons why people use substances. As we have explored, not all substance use will develop into a substance use disorder. There are many reasons why people use substances, one reason you may not have explored is mental health. Mental health is one of the social determinants of health, and good or poor mental health does play a role in a person’s substance use.
There are many individual factors that make people vulnerable or resilient to a substance use disorder (2). When we look at these characteristics, they may include positive self-image, self-control, or social competence as well as chronic illness, poverty, and homelessness (3). You may start to see a connection between mental health and substance use. There is a direct relationship (sometimes called a correlation) between mental health disorders and substance use disorders.

This is different than someone using a substance because of how they are feeling. Emotions like happiness and sadness may be a reason why someone uses a substance, for example having a drink at a social event. The difference between mental health and a mental health disorder, for example, depression, is that the mental health disorder is a diagnosable illness, like a substance use disorder. Healthcare practitioners use the DSM-V to diagnose mental health disorders, like substance use disorders. Some of the people you will meet will be living with mental health disorders AND substance use disorders; this may be called a concurrent disorder, or a dual diagnosis. People who have a concurrent disorder may experience a “combination of problems, such as: anxiety disorder and an alcohol problem, schizophrenia and cannabis dependence, borderline personality disorder and heroin dependence, and bipolar disorder and problem gambling” (4).
Which comes first, mental health or substance use? There are researchers on both sides of this argument. According to the Canadian Mental Health Association, “people who experience problems with alcohol or drug use are more likely to be diagnosed with a mental illness and people who experience a mental illness are more likely than others to also experience a substance use problem” (5). What we do know empirically, which means through research and observation, is mental health disorders and substance use disorders are related, regardless of which came first.
Food For Thought
- Reflect on a mental health disorder and substance use disorder. Why do you think they are related?
- Why do you think people who have mental health disorders use substances?
- What role do you think early diagnosis of a mental health disorder plays in the development of a substance use disorder? Why?
Please watch this video by Royal Talks, which helps explain the concurrent disorders and the importance of support for improved health outcomes.(6)
Connections Between Substance Use & Mental Health and Identifying Ways of Getting Help. Royal Talks (Royal Mental Health Centre) The landscape of substance use in Canada is changing. Societal impacts of the opioid crisis and cannabis legalization are now ever-present discussions in the media and our daily conversations. A significant portion of our population is affected directly or indirectly by substance use and/or mental health difficulties. Presenters: Dr. Isabelle Ares, Ph.D., C.Psych. Psychologist, Substance Use and Concurrent Disorders Program, The Royal Dr. Suzanne Bell, Ph.D., C.Psych. Psychologist, Substance Use and Concurrent Disorders Program, The Royal
Transcript
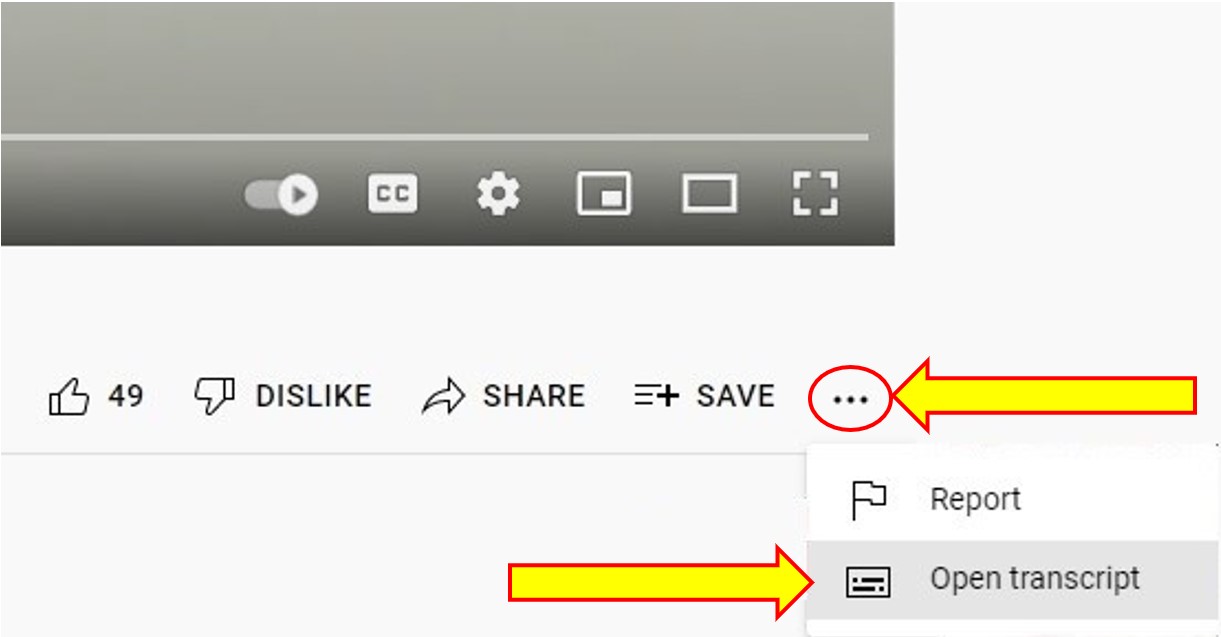
To Access the Video Transcript:
1. Click on “YouTube” on the bottom-right of the video. This will take you directly to the YouTube video.
2. Click on the More Actions icon (represented by three horizontal dots)
3. Click on “Open Transcript”
The risks of developing a substance use disorder if you have been diagnosed with a mental health disorder are high. According to the Mental Health Commission of Canada, “people living with mental illness are twice as likely as other Canadians to experience problematic substance use” (7). When we dig further into mental health disorders and look at specific disorders, Buckley et al. (8) suggest at least 50% of people who have been diagnosed with schizophrenia have a co-occurring substance use disorder.
Mental illness can impact anyone at any time; however, “70% of mental health problems have their onset during childhood or adolescence” (9) making substance use among youth especially problematic. If a young person is using substances to reduce the impacts of a mental health disorder, it is critical the mental health disorder be diagnosed early, so the appropriate treatments can be implemented, and the outcomes can improve. Early intervention programs that diagnose mental health disorders, along with programs to improve mental health, reduce risks for developing a substance abuse disorder. Promoting mental health, preventing mental health disorders, and preventing substance use are part of Health Canada’s focus on helping to “prevent, treat or reduce the harms associated with opioids, stimulants, alcohol, prescription drugs, and other potentially harmful substances” (10).
One way we can support individuals with concurrent disorders is to ensure they have access to appropriate resources, and the resources are working in collaboration.
Food For Thought
- Reflect on collaboration.
- What does collaboration mean to you?
- What is one strategy you could use to ensure collaboration with a community agency or healthcare provider?
As Social Service workers it is important to be aware of any diagnosis your client may have. This will help you direct clients to appropriate services for their health.
Activities
- Imagine you are working with a client who lives with depression and has an alcohol disorder.
- Brainstorm a list of resources that would be appropriate to address their concurrent disorder.
- Why did you choose these resources?
- What resources could you direct family members to if requested?
- Why is it important to be aware of family supports?
Chapter Attribution:
This Chapter is an adaptation of Exploring Substance Use in Canada by Julie Crouse is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Changes include adding material.
References
- World Health Organization. (2014). Social determinants of mental health, (p. 8). https://apps.who.int/iris/bitstream/handle/10665/112828/9789241506809_eng.pdf
- Substance and Mental Health Services Association. (n.d.). Risk and protective factors. https://www.samhsa.gov/sites/default/files/20190718-samhsa-risk-protective-factors.pdf
- Mawani, F. N., & Gilmour, H. (2010). Validation of self-rated mental health. Statistics Canada. https://www150.statcan.gc.ca/n1/en/pub/82-003-x/2010003/article/11288-eng.pdf?st=SgFoG2gh
- Centre for Addiction and Mental Health. (2021). Concurrent disorders, (para. 1). https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/concurrent-disorders
- Canadian Mental Health Association. (2018, December 4). Concurrent mental illness and substance use problems, (para. 2). https://cmha.ca/brochure/concurrent-mental-illness-and-substance-use-problems/
- Royal Talks. (2019). Connections between substance use & mental health and identifying ways of getting help. [Video]. Youtube. https://www.youtube.com/watch?v=lWhmc0tAuqc
- Mental Health Commission of Canada (2021). Mental health and substance use, (para. 1). https://mentalhealthcommission.ca/what-we-do/mental-health-and-substance-use/
- Buckley, P. F., Miller, B. J., Lehrer, D. S., & Castle, D. J. (2009). Psychiatric comorbidities and schizophrenia, Schizophrenia Bulletin, 35(2), 383–402. https://doi.org/10.1093/schbul/sbn135
- Canadian Scholars Press.Government of Canada. (2006). The human face of mental health and mental illness in Canada. Public Health Agency of Canada. https://www.phac-aspc.gc.ca/publicat/human-humain06/pdf/human_face_e.pdf
- Government of Canada. (2021). Substance use and addictions program. https://www.canada.ca/en/health-canada/services/substance-use/canadian-drugs-substances-strategy/funding/substance-use-addictions-program.html#wb-auto-4

