38 Physical Development in Older Adulthood
Theories of Aging
Why do we experience the negative effects of getting older and eventually die?). Jin (2010) highlighted modern biological theories of human aging in two categories.: Programmed Theories and Damage or Error Theories. These are two of the categories we discussed in the lecture and reading for Middle Adulthood. We will go through these theories more now. As we do, notice that it is not clear what is inevitable and what can be modified by us as societies and individuals. Programmed Theories follow a biological timetable, possibly a continuation of childhood development. This timetable would depend on “changes in gene expression that affect the systems responsible for maintenance, repair, and defense responses,” (p. 72). The second category includes Damage or Error Theories which emphasize environmental factors that cause cumulative damage in organisms. Examples from each of these categories will be discussed.
Genetics
One’s genetic make-up certainly plays a role in longevity, but scientists are still attempting to identify which genes are responsible. Based on animal models, some genes promote longer life, while other genes limit longevity. Specifically, longevity may be due to genes that better equip someone to survive a disease. For others, some genes may accelerate the rate of aging, while others decrease the rate. To help determine which genes promote longevity and how they operate, researchers scan the entire genome and compare genetic variants in those who live longer with those who have an average or shorter lifespan. For example, a National Institutes of Health study identified genes possibly associated with blood fat levels and cholesterol, both risk factors for coronary disease and early death (NIA, 2011a). Researchers believe that it is most likely a combination of many genes that affect the rate of aging.
Evolutionary Theory
Evolutionary psychology emphasizes the importance of natural selection ; that is, those genes that allow one to survive and reproduce will be more likely to be transmitted to offspring. Genes associated with aging, such as Alzheimer Disease, do not appear until after the individual has passed their main reproductive years. Consequently, natural selection has not eliminated these damaging disorders from the gene pool. If these detrimental disorders occurred earlier in the development cycle, they may have been eliminated already (Gems, 2014).
Cellular Clock Theory
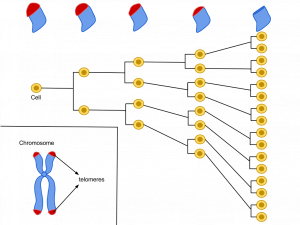
This theory suggests that biological aging is due to the fact that normal cells cannot divide indefinitely. This is known as the Hayflick limit, and is evidenced in cells studied in test tubes, which divide about 40-60 times before they stop (Bartlett, 2014). But what is the mechanism behind this cellular senescence? At the end of each chromosomal strand is a sequence of DNA that does not code for any particular protein, but protects the rest of the chromosome, which is called a telomere. With each replication, the telomere gets shorter. Once it becomes too short the cell does one of three things. It can stop replicating by turning itself off, called cellular senescence. It can stop replicating by dying, called apoptosis. Or, as in the development of cancer, it can continue to divide and become abnormal. Senescent cells can also create problems. While they may be turned off, they are not dead, thus they still interact with other cells in the body and can lead to an increase risk of disease. When we are young, senescent cells may reduce our risk of serious diseases such as cancer, but as we get older they increase our risk of such problems (NIA, 2011a). Understanding why cellular senescence changes from being beneficial to being detrimental is still under investigation. The answer may lead to some important clues about the aging process.
DNA Damage
Over time DNA, which contains the genetic code for all organisms, accumulates damage. This is usually not a concern as our cells are capable of repairing damage throughout our life. Further, some damage is harmless. However, some damage cannot be repaired and remains in our DNA. Scientists believe that this damage, and the body’s inability to fix itself, is an important part of aging (NIA, 2011a). As DNA damage accumulates with increasing age, it can cause cells to deteriorate and malfunction (Jin, 2010). Factors that can damage DNA include ultraviolet radiation, cigarette smoking, and exposure to hydrocarbons, such as auto exhaust and coal (Dollemore, 2006).
Mitochondrial Damage
Damage to mitochondrial DNA can lead to a decaying of the mitochondria, which is a cell organelle that uses oxygen to produce energy from food. The mitochondria convert oxygen to adenosine triphosphate (ATP) which provides the energy for the cell. When damaged, mitochondria become less efficient and generate less energy for the cell and can lead to cellular death (NIA, 2011a).
Free Radicals
When the mitochondria uses oxygen to produce energy, they also produce potentially harmful byproducts called oxygen free radicals (NIA, 2011a). The free radicals are missing an electron and create instability in surrounding molecules by taking electrons from them. There is a snowball effect (A takes from B and then B takes from C, etc.) that creates more free radicals which disrupt the cell and causes it to behave abnormally (See Figure 9.11). Some free radicals are helpful as they can destroy bacteria and other harmful organisms, but for the most part they cause damage in our cells and tissue. Free radicals are identified with disorders seen in those of advanced age, including cancer, atherosclerosis, cataracts, and neurodegeneration. Some research has supported adding antioxidants to our diets to counter the effects of free radical damage because the antioxidants can donate an electron that can neutralize damaged molecules. However, the research on the effectiveness of antioxidants is not conclusive (Harvard School of Public Health, 2016).
Immune and Hormonal Stress Theories


Ever notice how quickly Canadian prime ministers and U.S. presidents seem to age? Before and after photos reveal how stress can play a role in the aging process. When gerontologists study stress, they are not just considering major life events, such as unemployment, death of a loved one, or the birth of a child. They are also including metabolic stress, the life sustaining activities of the body, such as circulating the blood, eliminating waste, cont rolling bodytemperature, and neuronal firing in the brain. In other words, all the activities that keep the body alive also create biological stress.
To understand how this stress affects aging, researchers note that both problems with the innate and adaptive immune system play a key role. The innate immune system is made up of the skin, mucous membranes, cough reflex, stomach acid, and specialized cells that alert the body of an impending threat. With age these cells lose their ability to communicate as effectively, making it harder for the body to mobilize its defenses. The adaptive immune system includes the tonsils, spleen, bone marrow, thymus, circulatory system and the lymphatic system that work to produce and transport T cells. T-cells, or lymphocytes, fight bacteria, viruses, and other foreign threats to the body. T-cells are in a “naïve” state before they are programmed to fight an invader, and become “memory cells”. These cells now remember how to fight a certain infection should the body ever come across this invader again. Memory cells can remain in your body for many decades, and why the measles vaccine you received as a child is still protecting you from this virus today. As older adults produce fewer new T-cells to be programmed, they are less able to fight off new threats and new vaccines work less effectively. The reason why the shingles vaccine works well with older adults is because they already have some existing memory cells against the varicella virus. The shingles vaccine is acting as a booster (NIA, 2011a).
Hormonal Stress Theory, also known as Neuroendocrine Theory of Aging, suggests that as we age the ability of the hypothalamus to regulate hormones in the body begins to decline leading to metabolic problems (American Federation of Aging Research (AFAR) 2011). This decline is linked to excess of the stress hormone cortisol. While many of the body’s hormones decrease with age, cortisol does not (NIH, 2014a). The more stress we experience, the more cortisol released, and the more hypothalamic damage that occurs. Changes in hormones have been linked to several metabolic and hormone related problems that increase with age, such as diabetes (AFAR, 2011), thyroid problems (NIH, 2013), osteoporosis, and orthostatic hypotension (NIH, 2014a).
As you look back over these various theories about what causes the negative changes related to getting older, notice that as societies and individuals we already know of actions we can take to influence many of these processes, and research is uncovering more and more.
Physical Changes Associated with Getting Older
The Baltimore Longitudinal Study on Aging (BLSA) (NIA, 2011b) began in 1958 and has traced the aging process in 1,400 people from age 20 to 90. Researchers from the BLSA have found that the aging process varies significantly from individual to individual and from one organ system to another. However, some key generalization can be made including heart muscles thickening with age, arteries becoming less flexible, and lung capacity diminishing. Kidneys become less efficient in removing waste from the blood, and the bladder loses its ability to store urine. Brain cells also lose some functioning, but new neurons can also be produced. Many of these changes are determined by genetics, lifestyle, and disease. Other changes in late adulthood include:
Body Changes: Everyone’s body shape changes naturally as they age. According to the National Library of Medicine (2014) after age 30 people tend to lose lean tissue, and some of the cells of the muscles, liver, kidney, and other organs are lost. Tissue loss reduces the amount of water in your body and bones may lose some of their minerals and become less dense (a condition called osteopenia in the early stages and osteoporosis in the later stages). The amount of body fat goes up steadily after age 30, and older individuals may have almost one third more fat compared to when they were younger. Fat tissue builds up toward the center of the body, including around the internal organs.
Skin and Hair: With age skin becomes thinner, less elastic, loses fat, and no longer looks plump and smooth. Veins and bones can be seen more easily and scratches, cuts, and bumps can take longer to heal. Years exposed to the sun may lead to wrinkles, dryness, age spots, and cancer. Older people may bruise more easily, and it can take longer for these bruises to heal. Some medicines or illnesses may also cause bruising. Gravity can cause skin to sag and wrinkle, and smoking can wrinkle the skin. Also, seen in older adults are age spots, previously called “liver spots”. They look like flat, brown spots and are often caused by years in the sun. Skin tags are small, usually flesh-colored growths of skin that have a raised surface. They become common as people age, especially for women, but both age spots and skin tags are harmless (NIA, 2015f).
Nearly everyone has hair loss as they age, and the rate of hair growth slows down as many hair follicles stop producing new hairs. The loss of pigment and subsequent graying begun in middle adulthood continues in late adulthood.
Sarcopenia is the loss of muscle tissue as a natural part of aging. Sarcopenia is most noticeable in men, and physically inactive people can lose as much as 3% to 5% of their muscle mass each decade after age 30, but even when active muscle loss still occurs (Webmd, 2016). Symptoms include a loss of stamina and weakness, which can decrease physical activity and subsequently further shrink muscles. Sarcopenia typically happens faster around age 75, but it may also speed up as early as 65 or as late as 80. Factors involved in sarcopenia include a reduction in nerve cells responsible for sending signals to the muscles from the brain to begin moving, a decrease in the ability to turn protein into energy, and not receiving enough calories or protein to sustain adequate muscle mass. Any loss of muscle is important because it lessens strength and mobility, and sarcopenia is a factor in frailty and the likelihood of falls and fractures in older adults. Maintaining strong leg and heart muscles are important for independence. Weight-lifting, walking, swimming, or engaging in other cardiovascular exercises can help strengthen the muscles and prevent atrophy.
Height and Weight: The tendency to become shorter as one ages occurs among all races and both sexes. Height loss is related to aging changes in the bones, muscles, and joints. People typically lose almost one-half inch every 10 years after age 40, and height loss is even more rapid after age 70. A total of 1 to 3 inches in height is lost with aging. Changes in body weight vary for men and woman. Men often gain weight until about age 55, and then begin to lose weight later in life, possibly related to a drop in the male sex hormone testosterone. Women usually gain weight until age 65, and then begin to lose weight. Weight loss later in life occurs partly because fat replaces lean muscle tissue, and fat weighs less than muscle. Diet and exercise are important factors in weight changes in late adulthood (National Library of Medicine, 2014).
Sensory Changes in Older Adulthood
Vision
During older adulthood, all the senses show signs of decline, especially among the oldest-old. In the last chapter, you read about the visual changes that were beginning in middle adulthood, such as presbyopia, dry eyes, and problems seeing in dimmer light. By older adulthood these changes are much more common. Three serious eyes diseases are more common in older adults: Cataracts, macular degeneration, and glaucoma. Only the first can be effectively cured in most people.
Cataracts are a clouding of the lens of the eye. The lens of the eye is made up of mostly water and protein. The protein is precisely arranged to keep the lens clear, but with age some of the protein starts to clump. As more of the protein clumps together the clarity of the lens is reduced. While some adults in middle adulthood may show signs of cloudiness in the lens, the area affected is usually small enough to not interfere with vision. More people have problems with cataracts after age 60 (NIH, 2014b) and by age 75, 70% of adults will have problems with cataracts (Boyd, 2014). Cataracts also cause a discoloration of the lens, tinting it more yellow and then brown, which can interfere with the ability to distinguish colors such as black, brown, dark blue, or dark purple.
Risk factors besides age include certain health problems such as diabetes, high blood pressure, and obesity, behavioral factors such as smoking, other environmental factors such as prolonged exposure to ultraviolet sunlight, previous trauma to the eye, long- term use of steroid medication, and a family history of cataracts (NEI, 2016a; Boyd, 2014). Cataracts are treated by removing and replacing the lens of the eye with a synthetic lens. In developed countries, such as the United States, cataracts can be easily treated with surgery. However, in developing countries, access to such operations are limited, making cataracts the leading cause of blindness in late adulthood in Third World nations (Resnikoff, Pascolini, Mariotti & Pokharel, 2004). As shown in Figure 9.15, areas of the world with limited medical treatment for cataracts often results in people living more years with a serious disability. For example, of those living in the darkest red color on the map, more than 990 out of 100,00 people have a shortened lifespan due to the disability caused by cataracts.
Older adults are also more likely to develop age-related macular degeneration, which is the loss of clarity in the center field of vision, due to the deterioration of the macula, the center of the retina. Macular degeneration does not usually cause total vision loss, but the loss of the central field of vision can greatly impair day-to-day functioning. There are two types of macular degeneration: dry and wet. The dry type is the most common form and occurs when tiny pieces of a fatty protein called drusen form beneath the retina. Eventually the macular becomes thinner and stops working properly (Boyd, 2016). About 10% of people with macular degeneration have the wet type, which causes more damage to their central field of vision than the dry form. This form is caused by an abnormal development of blood vessels beneath the retina. These vessels may leak fluid or blood causing more rapid loss of vision than the dry form.
The risk factors for macular degeneration include smoking, which doubles your risk (NIH, 2015a); race, as it is more common among Caucasians than African Americans or Hispanics/Latinos; high cholesterol; and a family history of macular degeneration (Boyd, 2016). At least 20 different genes have been related to this eye disease, but there is no simple genetic test to determine your risk, despite claims by some genetic testing companies (NIH, 2015a). At present, there is no effective treatment for the dry type of macular degeneration. Some research suggests that certain patients may benefit from a cocktail of certain antioxidant vitamins and minerals, but the results are mixed at best. They are not a cure for the disease nor will they restore the vision that has been lost. This “cocktail” can slow the progression of visual loss in some people (Boyd, 2016; NIH, 2015a). For the wet type medications that slow the growth of abnormal blood vessels, and surgery, such as laser treatment to destroy the abnormal blood vessels may be used. Only 25% of those with the wet version may see improvement with these procedures (Boyd, 2016).
A third vision problem that increases with age is glaucoma, which is the loss of peripheral vision, frequently due to a buildup of fluid in eye that damages the optic nerve. As you age the pressure in the eye may increase causing damage to the optic nerve. The exterior of the optic nerve receives input from retinal cells on the periphery, and as glaucoma progresses more and more of the peripheral visual field deteriorates toward the central field of vision. In the advanced stages of glaucoma, a person can lose their sight. Fortunately, glaucoma tends to progress slowly (NEI, 2016b).
Glaucoma is the most common cause of blindness in the U.S. (NEI, 2016b). African Americans over age 40, and everyone else over age 60 has a higher risk for glaucoma. Those with diabetes, and with a family history of glaucoma also have a higher risk (Owsley et al., 2015). There is no cure for glaucoma, but its rate of progression can be slowed, especially with early diagnosis. Routine eye exams to measure eye pressure and examination of the optic nerve can detect both the risk and presence of glaucoma (NEI, 2016b). Those with elevated eye pressure are given medicated eye drops. Reducing eye pressure lowers the risk of developing glaucoma or slow its progression in those who already have it.
Hearing
As you read in earlier sections of this text, our hearing declines both in terms of the frequencies of sound we can detect and the intensity of sound needed to hear as we age. These changes continue in late adulthood. Almost 1 in 4 adults aged 65 to 74 and 1 in 2 aged 75 and older have disabling hearing loss (NIH, 2016). Table 9.4 lists some common signs of hearing loss.
Presbycusis is a common form of hearing loss in late adulthood that results in a gradual loss of hearing. It runs in families and affects hearing in both ears (NIA, 2015c). Older adults may also notice tinnitus, a ringing, hissing, or roaring sound in the ears. The exact cause of tinnitus is unknown, although it can be related to hypertension and allergies. It may come and go or persist and get worse over time (NIA, 2015c). The incidence of both presbycusis and tinnitus increase with age and males have higher rates of both around the world (McCormak, Edmondson-Jones, Somerset, & Hall, 2016).
Your auditory system has two jobs: To help you to hear, and to help you maintain balance. Your balance is controlled by the brain receiving information from the shifting of hair cells in the inner ear about the position and orientation of the body. With age this function of the inner ear declines which can lead to problems with balance when sitting, standing, or moving (Martin, 2014).
Taste and Smell
Our sense of taste and smell are part of our chemical sensing system. Our sense of taste, or gustation, appears to age well. Normal taste occurs when molecules that are released by chewing food stimulate taste buds along the tongue, the roof of the mouth, and in the lining of the throat. These cells send messages to the brain, where specific tastes are identified. After age 50 we start to lose some of these sensory cells. Most people do not notice any changes in taste until ones 60s (NIH: Senior Health, 2016b). Given that the loss of taste buds is very gradual, even in older adulthood, many people are often surprised that their loss of taste is most likely the result of a loss of smell.
Our sense of smell, or olfaction, decreases more with age, and problems with the sense of smell are more common in men than in women. Almost 1 in 4 males in their 60s have a disorder with the sense of smell, while only 1 in 10 women do (NIH: Senior Health, 2016b). This loss of smell due to aging is called presbyosmia. Olfactory cells are located in a small area high in the nasal cavity. These cells are stimulated by two pathways; when we inhale through the nose, or via the connection between the nose and the throat when we chew and digest food. It is a problem with this second pathway that explains why some foods such as chocolate or coffee seem tasteless when we have a head cold. There are several types of loss of smell. Total loss of smell, or anosmia, is extremely rare.
Problems with our chemical senses can be linked to other serious medical conditions such as Parkinson’s, Alzheimer’s, or multiple sclerosis (NIH: Senior Health, 2016a). Any sudden change should be checked out. Loss of smell can change a person’s diet, with either a loss of enjoyment of food and eating too little for balanced nutrition, or adding sugar and salt to foods that are becoming blander to the palette.
Touch
Research has found that with as we get older, we may experience reduced or changed sensations of vibration, cold, heat, pressure, or pain (Martin, 2014). Many of these changes are also aligned with a number of medical conditions that are more common among older people, such as diabetes. However, there are changes in the touch sensations among healthy older adults. The ability to detect changes in pressure have been shown to decline with age, with it being more pronounced by the 6th decade and diminishing further with advanced age (Bowden & McNelty, 2013). Yet, there is considerable variability, with almost 40% showing sensitivity that is comparable to younger adults (Thornbury & Mistretta, 1981). However, the ability to detect the roughness/smoothness or hardness/softness of an object shows no appreciable change with age (Bowden & McNulty, 2013). Those who show increasing insensitivity to pressure, temperature, or pain are at risk for injury (Martin, 2014).
Pain
According to Molton and Terrill (2014), approximately 60%-75% of people over the age of 65 report at least some chronic pain, and this rate is even higher for those individuals living in nursing homes. Although the presence of pain increases with age, older people are less sensitive to pain than younger adults (Harkins, Price, & Martinelli, 1986). Farrell (2012) looked at research studies that included neuroimaging techniques involving older people who were healthy and those who experienced a painful disorder. Results indicated that there were age-related decreases in brain volume in those structures involved in pain. Especially noteworthy were changes in the prefrontal cortex, brainstem, and hippocampus. Women are more likely to identify feeling pain than men (Tsang et al., 2008). Women have fewer opioid receptors in the brain, and women also receive less relief from opiate drugs (Garrett, 2015). Because pain serves an important indicator that there is something wrong, a decreased sensitivity to pain in older adults is a concern because it can conceal illnesses or injuries requiring medical attention.
Chronic health problems, including arthritis, cancer, diabetes, joint pain, sciatica, and shingles are responsible for most of the pain felt by older adults (Molton & Terrill, 2014). Cancer is a special concern, especially “breakthrough pain” which is a severe pain that comes on quickly while a patient is already medicated with a long-acting painkiller. It can be very upsetting, and after one attack many people worry it will happen again. Some older individuals worry about developing an addiction to pain medication, but if medicine is taken exactly as prescribed, addiction should not be a concern (NIH, 2015b). Lastly , side effects from pain medicine including constipation, dry mouth, and drowsiness may occur that can adversely affect us as older people as at earlier points in our lives.
Some older individuals put off going to the doctor because they think pain is just part of aging and nothing can help. Of course this is not true. Managing pain is crucial to ensure feelings of well-being for the older adult. When chronic pain is not managed, the individual will restrict their movements for fear of feeling pain or injuring themselves further. This lack of activity will result in more restriction, further decreased participation, and greater disability (Jensen, Moore, Bockow, Ehde, & Engel, 2011). A decline in physical activity because of pain is also associated with weight gain and obesity in adults (Strine, Hootman, Chapman, Okoro, & Balluz, 2005). Additionally sleep and mood disorders, such as depression, can also occur (Moton & Terrill, 2014). Pain is a struggle many of us have off and on or chronically throughout adulthoood. There is much to learn about coping effectively with pain. Older people like younger people have the capacity to make major strides in dealing with pain given coaching from their healthcare providers and pain specialists.
Nutrition
A healthy diet is necessary for everyone to increase mental acuteness, resistance to illness and disease, boost energy levels, improve immune system strength, recuperation speed, and have greater effectiveness in the management of chronic health problems. The effects of long-term poor nutrition become particularly apparent when we are older people (Mayer, 2016). We can improve health substantially through nutrition at any age. The science of supporting the various nutritional needs of older people is advancing. Although the challenge of “eating right” becomes greater as we get older, providing basic adequate nutrition for all, from infants to older adults, is central to a just society. Canada, the U.S., and other developed societies have the ingenuity and resources to take on.this challenge. The new MyPlate for Older Adults, a website from Tufts University, suggests that older adults should strive for 50% of their diet being fruits and vegetables; 25% grains, many of which should be whole grains; and 25% protein-rich foods, such as nuts, beans, fish, lean meat, poultry, and fat-free and low-fat dairy products such as milk, cheeses, and yogurts.
Unfortunately, changes in sensory functions, such as smell and taste, along with loss of teeth, can derail an older adult’s ability to eat right. Older adults are likely to use salt and sugar to flavor foods that no longer taste the way they once did. Several government websites provide older adults with alternatives to the salt shaker to make foods more palatable.
Media Attributions
- 090-HayflickLimitTelomeres © Azmistowski17 is licensed under a CC BY-SA (Attribution ShareAlike) license
- 091-Obama2012 © United States Government is licensed under a All Rights Reserved license
- 091-Obama2007 is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license

