41 Cognitive Development in Older People
How Does Getting Older Affect Information Processing?
There are numerous stereotypes regarding older adults as being forgetful and confused, but what does the research on memory and cognition reveal? Memory comes in many types, such as working, episodic, semantic, implicit, and prospective. There are also many processes involved in memory. Thus, it should not be a surprise that there are declines in some types of memory and memory processes, while other areas of memory are maintained or even show some improvement as we get older. This is consistent with the concepts of multidimensionality and multidiretionality in Baltes’s theory of lifespan development. In this section, we will focus on changes in memory, attention, problem solving, intelligence, and wisdom, including the effects negative age stereotypes can have on older people.
Memory
Changes in Working Memory
Working memory is the more active, effortful part of our memory system. Working memory is composed of three major systems: The phonological loop that maintains information about auditory stimuli, the visuospatial sketchpad, that maintains information about visual stimuli, and the central executive, that oversees working memory, allocating resources where needed and monitoring whether cognitive strategies are being effective (Schwartz, 2011). Schwartz reports that it is the central executive that is most negatively impacted by age. In tasks that require allocation of attention between different stimuli, older people fare worse than do younger adults. In a study by Göthe, Oberauer, and Kliegl (2007) older and younger adults were asked to learn two tasks simultaneously. Young adults eventually managed to learn and perform each task without any loss in speed and efficiency, although it did take considerable practice. None of the older adults were able to achieve this. Yet, older adults could perform at young adult levels if asked to learn each task individually. Having older adults learn and perform both tasks together was too taxing for the central executive. In contrast, in working memory tasks that do not require much input from the central executive, such as the digit span test, which uses predominantly the phonological loop, older adults perform on par with young adults (Dixon & Cohen, 2003).
Changes in Long-term Memory
Long-term memory is divided into semantic (knowledge of facts), episodic (events), and implicit (procedural skills, classical conditioning and priming) memories. Semantic and episodic memory are part of the explicit memory system, which requires conscious effort to create and retrieve. Several studies consistently reveal that episodic memory shows greater age -related declines than semantic memory (Schwartz, 2011; Spaniol, Madden, & Voss, 2006). It has been suggested that episodic memories may be harder to encode and retrieve because they contain at least two different types of memory, the event and when and where the event took place. In contrast, semantic memories are not tied to any particular time line. Thus, only the knowledge needs to be encoded or retrieved (Schwartz, 2011). Spaniol et al. (2006) found that retrieval of semantic information was considerably faster for both younger and older adults than the retrieval of episodic information, with there being little difference between the two age groups for semantic memory retrieval. They note that older adults’ poorer performance on episodic memory appeared to be related to slower processing of the information and the difficulty of the task. They found that as the task became increasingly difficult, the gap between each age groups’ performance increased for episodic memory more so than for semantic memory.
Studies which test general knowledge (semantic memory), such as politics and history (Dixon, Rust, Feltmate, & See, 2007), or vocabulary/lexical memory (Dahlgren, 1998) often find that older adults outperform younger adults. However, older adults do find that they experience more “blocks” at retrieving information that they know. In other words, they experience more tip-of- the-tongue (TOT) events than do younger adults (Schwartz, 2011).
Implicit memory requires little conscious effort and often involves skills or more habitual patterns of behavior. This type of memory shows few declines with age. Many studies assessing implicit memory measure the effects of priming. Priming refers to changes in behavior as a result of frequent or recent experiences. If you were shown pictures of food and asked to rate their appearance and then later were asked to complete words such as s_ _ p, you may be more likely to write soup than soap, or ship. The images of food “primed” your memory for words connected to food. Does this type of memory and learning change with age? The answer is typically “no” for most older adults (Schacter, Church, & Osowiecki, 1994).
Prospective memory refers to remembering things we need to do in the future, such as remembering a doctor’s appointment next week, or to take medication before bedtime. It has been described as “the flip-side of episodic memory” (Schwartz, 2011, p. 119). Episodic memories are the recall of events in our past, while the focus of prospective memories is of events in our future. In general, humans are fairly good at prospective memory if they have little else to do in the meantime. However, when there are competing tasks that are also demanding our attention, this type of memory rapidly declines. The explanation given for this is that this form of memory draws on the central executive of working memory, and when this component of working memory is absorbed in other tasks, our ability to remember to do something else in the future is more likely to slip out of memory (Schwartz, 2011). However, prospective memories are often divided into time-based prospective memories, such as having to remember to do something at a future time, or event-based prospective memories, such as having to remember to do something when a certain event occurs. When age-related declines are found, they are more likely to be time-based, than event-based, and in laboratory settings rather than in the real-world, where older adults can show comparable or slightly better prospective memory performance (Henry, MacLeod, Phillips & Crawford, 2004; Luo & Craik, 2008). This should not be surprising given the tendency of older adults to be more selective in where they place their physical, mental, and social energy. Having to remember a doctor’s appointment is of greater concern than remembering to hit the space-bar on a computer every time the word “tiger” is displayed.
Recall versus Recognition
Memory performance often depends on whether older adults are asked to simply recognize previously learned material or recall material on their own. Generally, for all humans, recognition tasks are easier because they require less cognitive energy. Older adults show roughly equivalent memory to young adults when assessed with a recognition task (Rhodes, Castel, & Jacoby, 2008). With recall measures, older adults show memory deficits in comparison to younger adults. While the effect is initially not that large, starting at age 40 adults begin to show declines in recall memory compared to younger adults (Schwartz, 2011).
The Age Advantage
Fewer age differences are observed when memory cues are available, such as for recognition memory tasks, or when individuals can draw upon acquired knowledge or experience. For example, older adults often perform as well if not better than young adults on tests of word knowledge or vocabulary. With age often comes expertise, and research has pointed to areas where aging experts perform quite well. For example, older typists were found to compensate for age-related declines in speed by looking farther ahead at printed text (Salthouse, 1984). Compared to younger players, older chess experts focus on a smaller set of possible moves, leading to greater cognitive efficiency (Charness, 1981). Accrued knowledge of everyday tasks, such as grocery prices, can help older adults to make better decisions than young adults (Tentori, Osheron, Hasher, & May, 2001).
Attention and Problem Solving
Changes in Attention in Late Adulthood
Changes in sensory functioning and speed of processing information in late adulthood often translates into changes in attention (Jefferies et al., 2015). Research has shown that older adults are less able to selectively focus on information while ignoring distractors (Jefferies et al., 2015; Wascher, Schneider, Hoffman, Beste, & Sänger, 2012), although Jefferies and her colleagues found that when given double time, older adults could perform at young adult levels. Other studies have also found that older adults have greater difficulty shifting their attention between objects or locations (Tales, Muir, Bayer, & Snowden, 2002). Consider the implication of these attentional changes for older adults.
How do changes or maintenance of cognitive ability affect older adults’ everyday lives? Researchers have studied cognition in the context of several different everyday activities. One example is driving. Although older adults often have more years of driving experience, cognitive declines related to reaction time or attentional processes may pose limitations under certain circumstances (Park & Gutchess, 2000). In contrast, research on interpersonal problem solving suggested that older adults use more effective strategies than younger adults to navigate through social and emotional problems (Blanchard-Fields, 2007). In the context of work, researchers rarely find that older individuals perform poorer on the job (Park & Gutchess, 2000). Similar to everyday problem solving, older workers may develop more efficient strategies and rely on expertise to compensate for cognitive decline.
Problem Solving
Problem solving tasks that require processing non-meaningful information quickly (a kind of task that might be part of a laboratory experiment on mental processes) declines with age. However, many real-life challenges facing older adults do not rely on speed of processing or making choices on one’s own. Older adults resolve everyday problems by relying on input from others, such as family and friends. They are also less likely than younger adults to delay making decisions on important matters, such as medical care (Strough, Hicks, Swenson, Cheng & Barnes, 2003; Meegan & Berg, 2002).
What might explain these deficits as we age?
The processing speed theory, proposed by Salthouse (1996, 2004), suggests that as the nervous system slows as we become older our ability to process information declines. This slowing of processing speed may explain age differences on many different cognitive tasks. For instance, as we get older, working memory becomes less efficient (Craik & Bialystok, 2006). Older adults also need longer time to complete mental tasks or make decisions. Yet, when given sufficient time older adults perform as competently as do young adults (Salthouse, 1996). Thus, when speed is not imperative to the task healthy older adults do not show cognitive declines.
In contrast, inhibition theory argues that older adults have difficulty with inhibitory functioning, or the ability to focus on certain information while suppressing attention to less pertinent information tasks (Hasher & Zacks, 1988). Evidence comes from directed forgetting research. In directed forgetting people are asked to forget or ignore some information, but not other information. For example, you might be asked to memorize a list of words, but you are then told that the researcher made a mistake and gave you the wrong list, and directed to “forget” this list. You are then given a second list to memorize. While most people do well at forgetting the first list, older adults are more likely to recall more words from the “forget-to-recall” list than are younger adults (Andrés, Van der Linden, & Parmentier, 2004).
Cognitive losses exaggerated
While there are information processing losses in late adulthood, overall loss has been exaggerated (Garrett, 2015). One explanation is that the type of tasks that people are tested on in research studies tends to involve meaningless information. For example, older individuals are not motivated to remember a random list of words in a study, but they are motivated for more meaningful material related to their life, and consequently perform better on those tests. Another reason is that the research is often cross-sectional. When age comparisons occur longitudinally, however, the research results show less loss (Schaie, 1994). A third reason is that the loss may be due to a lack of opportunity in various skills. When older adults practiced skills, they performed as well as they had previously. Although diminished performance speed is especially noteworthy in older people, Schaie (1994) found that statistically removing the effects of speed diminished the individual’s performance declines significantly. In fact, Salthouse and Babcock (1991) demonstrated that processing speed accounted for all but 1% of age-related differences in working memory when testing individuals from 18 to 82. Finally, it is well established that our hearing and vision decline as we age. Longitudinal research has proposed that deficits in sensory functioning explain age differences in a variety of cognitive abilities (Baltes & Lindenberger, 1997).
Intelligence and Wisdom
When looking at scores on traditional intelligence tests, tasks measuring verbal skills show minimal or no age-related declines, while scores on performance tests, which measure solving problems quickly, decline as we get older (Botwinick, 1984). This profile mirrors crystalized and fluid intelligence. As you recall from last chapter, crystallized intelligence encompasses abilities that draw upon experience and knowledge. Measures of crystallized intelligence include vocabulary tests, solving number problems, and understanding texts. Fluid intelligence refers to information processing abilities, such as logical reasoning, remembering lists, spatial ability, and reaction time. Baltes (1993) introduced two additional types of intelligence to reflect cognitive changes in aging. Pragmatics of intelligence are cultural exposure to facts and procedures that are maintained as one gets older and are similar to crystalized intelligence. Mechanics of intelligence are dependent on brain functioning and decline with age, similar to fluid intelligence. Baltes indicated that pragmatics of intelligence show little decline and typically increase with age. Additionally, pragmatics of intelligence may compensate for the declines that occur with mechanics of intelligence. In summary, global cognitive declines are not typical as one ages, and individuals compensate for some cognitive declines, especially processing speed.
Wisdom is the ability to use the accumulated knowledge about practical matters that allows for sound judgment and decision making. A wise person is insightful and has knowledge that can be used to overcome obstacles in living. Does getting older bring wisdom? While living longer brings experience, it does not always bring wisdom. Paul Baltes and his colleagues (Baltes & Kunzmann, 2004; Baltes & Staudinger, 2000) suggest that wisdom is rare. In addition, the emergence of wisdom can be seen in late adolescence and young adulthood, with there being relatively modest gains on average in wisdom over the course of adulthood (Staudinger & Gluck, 2011). This would suggest that factors other than age are stronger determinants of wisdom. Occupations and experiences that emphasize others rather than self, along with personality characteristics, such as openness to experience and generativity, are more likely to provide the building blocks of wisdom (Baltes & Kunzmann, 2004). Age combined with certain types of experience and/or personality brings wisdom.
Neurocognitive Disorders
Historically, the term dementia was used to refer to an individual experiencing a marked decline from their past level in one or more of these areas: memory, language, abstract thinking, reasoning, decision making, and problem-solving (Erber & Szuchman (2015). However, in the latest edition of the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) (American Psychiatric Association, 2013) the term dementia has been replaced by neurocognitive disorder. A Major Neurocognitive Disorder is diagnosed as a significant cognitive decline from a previous level of performance in one or more cognitive domains and interferes with independent functioning, while a Minor Neurocognitive Disorder is diagnosed as a modest cognitive decline from a previous level of performance in one of more cognitive domains and does not interfere with independent functioning. There are several different neurocognitive disorders that are typically first diagnosed in older adulthood. Determining the exact type can be difficult because the symptoms and diagnostic test findings may overlap with each other. Diagnosis often relies on medical history, physical exam, laboratory tests, and changes noted in behavior by family and/or the healthcare team (and sometimes documented in detail by neuropsychological assessment). Alzheimer’s disease, Vascular Neurocognitive Disorder and Neurocognitive Disorder with Lewy bodies will be discussed below.
Alzheimer’s disease
Probably the most well-known and most common major neurocognitive disorder for older individuals is Alzheimer’s disease. In 2016 an estimated 5.4 million Americans were diagnosed with Alzheimer’s disease (Alzheimer’s Association, 2016), which was approximately one in nine aged 65 and over. In Canada it is estimated that more than 747,000 people are living with Alzheimer’s disease or another dementia (Alzheimer’s Association, 2019, https://www.alz.org/ca/dementia-alzheimers-canada.asp#about). Alzheimer’s disease has a gradual onset with subtle personality changes and memory loss that differs from normal age-related memory problems occurring first. Confusion, difficulty with change, and deterioration in language, problem-solving skills, and personality become evident next. In the later stages, the individual loses physical coordination and is unable to complete everyday tasks, including self-care and personal hygiene (Erber & Szuchman, 2015). Lastly, individuals lose the ability to respond to their environment, to carry on a conversation, and eventually to control movement (Alzheimer’s Association, 2016). On average people with Alzheimer’s survive eight years, but some may live up to 20 years. The disease course often depends on the individual’s age and whether they have other health conditions.
The greatest risk factor for Alzheimer’s disease is age, but there are genetic and environmental factors that can also contribute. Some forms of Alzheimer’s are hereditary, and with the early onset type, several rare genes have been identified that directly cause Alzheimer’s. People who inherit these genes tend to develop symptoms in their 30s, 40s and 50s. Five percent of those identified with Alzheimer’s disease are younger than age 65. When Alzheimer’s disease is caused by deterministic genes, it is called familial Alzheimer’s disease (Alzheimer’s Association, 2016). Traumatic brain injury is also a risk factor, as well as obesity, hypertension, high cholesterol, and diabetes (Carlson, 2011).
According to Erber and Szuchman (2015) the problems that occur with Alzheimer’s disease are due to the “death of neurons, the breakdown of connections between them, and the extensive formation of plaques and tau, which interfere with neuron functioning and neuron survival” (p. 50). Plaques are abnormal formations of protein pieces called beta-amyloid. Beta-amyloid comes from a larger protein found in the fatty membrane surrounding nerve cells. Because beta-amyloid is sticky, it builds up into plaques (Alzheimer’s Association, 2016). These plaques appear to block cell communication and may also trigger an inflammatory response in the immune system, which leads to further neuronal death.
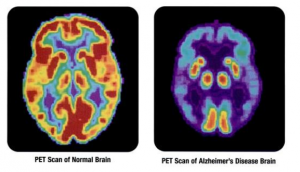
Tau is an important protein that helps maintain the brain’s transport system. When tau malfunctions, it changes into twisted strands called tangles that disrupt the transport system. Consequently, nutrients and other supplies cannot move through the cells and they eventually die. The death of neurons leads to the brain shrinking and affecting all aspects of brain functioning. For example, the hippocampus is involved in learning and memory, and the brain cells in this region are often the first to be damaged. This is why memory loss is often one of the earliest symptoms of Alzheimer’s disease. Figure 6.41.1 illustrates the difference between an Alzheimer’s brain and a healthy brain.
Vascular Neurocognitive Disorder
Vascular Neurocognitive Disorder is the second most common major neurocognitive disorder affecting 0.2% in the 65-70 years age group and 16% of individuals 80 years and older (American Psychiatric Association, 2013). Vascular neurocognitive disorder is associated with a blockage of cerebral blood vessels that affects one part of the brain rather than a general loss of brain cells seen with Alzheimer’s disease. Personality is not as affected in vascular neurocognitive disorder, and more males are diagnosed than females (Erber and Szuchman, 2015). It also comes on more abruptly than Alzheimer’s disease and has a shorter course before death. Risk factors include smoking, diabetes, heart disease, hypertension, or a history of strokes.
Neurocognitive Disorder with Lewy bodies: According to the National Institute on Aging (2015a), Lewy bodies are microscopic protein deposits found in neurons seen postmortem. They affect chemicals in the brain that can lead to difficulties in thinking, movement, behavior and mood. Neurocognitive Disorder with Lewy bodies is the third most common major neurocognitive disorder and affects more than 1 million Americans. It typically begins at age 50 or older, and appears to affect slightly more men than women. The disease lasts approximately 5 to 7 years from the time of diagnosis to death, but can range from 2 to 20 years depending on the individual’s age, health, and severity of symptoms. Lewy bodies can occur in both the cortex and brain stem which results in cognitive as well as motor symptoms (Erber & Szuchman, 2015). The movement symptoms are similar to those with Parkinson’s disease and include tremors and muscle rigidity. However, the motor disturbances occur at the same time as the cognitive symptoms, unlike with Parkinson’s disease when the cognitive symptoms occur well after the motor symptoms. Individuals diagnosed with Neurocognitive Disorder with Lewy bodies also experience sleep disturbances, recurrent visual hallucinations, and are at risk for falling.
Media Attributions
- 092-AlzheimersBrain3 © Health and Human Services Department, National Institutes of Health, National Institute on Aging

