39 Health Concerns in Older Adulthood
Chronic Conditions
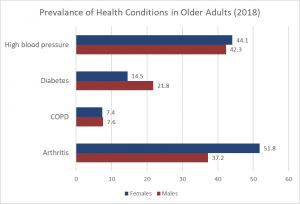
Chronic illnesses are illnesses that are ongoing, generally (but not always) incurable conditions that require continuing medical attention and affect daily life. The older a cohort becomes the more prevalent are diseases associated with advanced age and the greater the average individual’s overall burden of chronic illness. Less than 50% of adults 50-64 have a chronic condition, yet 90% aged 75 and up do (Cohen, 2011). Older women are more likely to have a chronic condition than are older men (83% vs. 88%) (CDC, 2009). Table 6.39.1 lists the percentage of older adults who have certain chronic illnesses based on the 2018 Statistics Canada Health Survey. Other studies place the figure of diabetes in older adults at 26% (CDC, 2014).
Cancer and Major Cardiovascular Disease
As discussed earlier, cancer and cardiovascular disease are the overall leading causes of death, and they are especially high reasons for death in middle and late adults. Table 6.39.2 identifies the percentages of deaths due to cancer and cardiovascular disease for selected age groups in 2018; the most recent year for data .
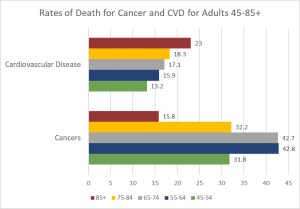
Cancer: Advancing age is a significant risk factor for cancer, with persons over 65 accounting for 60% of newly diagnosed cancer and 70% of all cancer deaths (Berger et al., 2006). Additionally, more than 70% of the mortality associated with many cancers, including prostate, bladder, colon, uterus, pancreas, stomach, rectum and lung occur in people 65 and older. Other conditions that affect older people can occur with cancer, including anemia, coronary artery diseases, congestive heart failure, chronic obstructive pulmonary diseases, renal insufficiency, cerebrovascular diseases, neurovascular complications of diabetes mellitus, and arthritis that restricts mobility (Balducci & Extermann, 2000). Comorbidity will complicate treatment.
Balducci and Extermann (2000) examined several concerns about cancer treatment in older people. With aging, there is a decline in multiple organ systems that can adversely affect the ability of medications to treat the cancer. Chemotherapy has been found to compromise the cognitive function of those being treated for cancer, and it may further exacerbate dementia and cognitive declines, conditions more likely to be found in older people. Frail individuals, defined as having limited life expectancy and near-to- exhausted functional reserves, are also not considered candidates for more toxic forms of chemotherapy. With cancer, the prevalence and risk of malnutrition are higher, and diminished visual and hearing function makes older cancer patients more susceptible to environmental injury. Screening for depression is also recommended because depression is associated with weight loss, failure to thrive, and may reduce the motivation to receive treatment. Consequently, depression has been associated with decreased survival rates in older people. Due to the projected increase in the total number of older people with cancer, it is recommended that physicians and caretakers have expertise in both oncology and geriatrics (Berger et al., 2006).
Heart Disease: There are changes to the heart that occur as we get older, and some may increase a person’s risk of heart disease. These include stiffening blood vessels and valves, which may result in leaks or problems pumping blood out of the heart (NIA, 2012). As previously stated, heart disease is the leading cause of death for older people in the US (CDC, 2016b). There are different types of heart disease, and as already discussed earlier, the most common is atherosclerosis, the buildup of fatty deposits or plaques in the walls of arteries. As plaque builds up, blood is unable to flow normally and bring oxygen throughout the body, including to the heart. Depending on where the buildup is, atherosclerosis can cause a heart attack, leg pain, or a stroke. However, atherosclerosis is not an inevitable part of getting older. Many of the problems older people have with their heart and blood vessels are caused by disease and not by getting older. For example, an older heart can normally pump blood as strong as a younger heart, while less ability to pump blood is caused by disease. Therefore, leading a heart-healthy lifestyle is most important to keeping one’s heart strong when one becomes an older person.
Arthritis: Arthritis and other rheumatic conditions are the most common cause of disability among US adults, and have been the most common cause of disability among US adults for the past 15 years (NIH: National Institute of Arthritis and Musculoskeletal and Skin Diseases, 2014). According to the NIH, approximately 62% of adults with arthritis are 65 years old and up. Almost 1 in 2 older adults with arthritis have some degree of mobility limitations, such as climbing stairs, walking, and grasping objects. The pain and other limitations of arthritis can also increase the risk of depression and other forms of mental distress. Osteoarthritis is the most common type of arthritis. “When the cartilage, the slick, cushioning surface on the ends of bones wears away, bone rubs against bone, causing pain, swelling and stiffness. Over time, joints can lose strength and pain may become chronic” (Arthritis Foundation, 2017, para 3). Common risk factors for osteoarthritis include genetics, obesity, age, previous injury, and other medical conditions.
Osteoporosis and Kyphosis: Osteoporosis is a disease that thins and weakens bones to the point that they become fragile and break easily. After age 50, 1 in 2 women and 1 in 4 men will experience an osteoporosis related fracture in their lifetime, often leading to hip, spine, and wrist fractures (Dailey & Cravedi, 2006). Broken hips are a very serious problem as we age. They greatly increase the risk of death, especially during the year after they break (NIH Senior Health, 2015). In the U.S., more than 53 million adults either already have osteoporosis or at a high risk due to low bone mass (NIH Senior Health, 2015). As bones weaken in the spine, adults gradually lose height and their posture becomes hunched over, which is called Kyphosis. Over time a bent spine can make it hard to walk or even sit up. Adults can prevent the loss of bone mass by eating a healthy diet with enough calcium and vitamin D, regularly exercising, limiting alcohol, and not smoking (National Osteoporosis Foundation, 2016).
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease in which the airways become damaged making it difficult to breathe. COPD includes problems such as emphysema and chronic bronchitis (NIH Senior Health, 2013). COPD kills more than 120,000 people every year, making it one of the leading causes of death. Figure 9.20 compares healthy to damaged lungs due to COPD. As COPD develops slowly, people may not notice the early signs, and may attribute the shortness of breath to age or lack of physical exercise. Most people are not diagnosed until they become middle-aged or older.. There is no cure as the damage cannot be reversed. Treatments aim at slowing further damage.
Cigarette smoking is the leading cause of COPD, but other types of tobacco smoking, such as a pipe or cigar, can cause COPD, especially if the smoke is inhaled. Heavy or long-term exposure to second hand smoke can also lead to COPD (NIH Senior Health, 2013). COPD can also occur in people who have long term exposure to other environmental irritants, such as chemical fumes, and dust from the environment and workplace.
About 1 in every 1,600 to 5,000 people have a risk for COPD because of a recessive genetic condition known as alpha-1 antitrypsin (AAT) deficiency (NIH, 2011). AAT is a protein made in the liver that protects organs, especially the lungs, from the effects of other harmful proteins. In those with the genetic defect, the AAT protein created is the wrong shape and cannot leave the liver. This can lead to a heightened risk for lung disease, and even liver disease, as the excess of the AAT protein can lead to cirrhosis, which is a disease in which the liver becomes scarred and does not function properly. While some people with ATT deficiency are not affected and live a normal life, COPD is more likely to occur in such individuals if their lungs are exposed to environmental irritants.
Shingles: According to the National Institute on Aging (2015e), shingles is a disease that affects your nerves. Shingles is caused by the same virus as chicken pox, the varicella-zoster virus (VZV). After you recover from chickenpox, the virus continues to live in some of your nerve cells. It is usually inactive, and most adults live with VZV in their body and never get shingles. However, the virus will become active in one in three adults. Instead of causing chickenpox again, it produces shingles. A risk factor for shingles includes advanced age as people have a harder time fighting off infections as they get older. About half of all shingles cases are in adults age 60 or older, and the chance of getting shingles becomes much greater by age 70. Other factors that weaken an individual’s ability to fight infections, such as cancer, HIV infections, or other medical conditions, can put one at a greater risk for developing shingles.
Shingles results in pain, burning, tingling, or itching in the affected area, as well as a rash and blisters. Typically, shingles develops only on one side of the body or face and in a small area rather than all over. Most cases of shingles last 3 to 5 weeks. After the shingles rash goes away, some people may be left with ongoing pain, called post-herpetic neuralgia (PHN) in the area where the rash had been (NIA, 2015e). The older one is when getting shingles, the greater the chance of developing PHN. Some people with PHN find it hard to go about their daily activities, like dressing, cooking, and eating. They can also suffer from depression, anxiety and sleeplessness. Medicines can help with pain and usually PHN will disappear. Unfortunately, the blisters from shingles may become infected or leave a scar. Blisters near or in the eye can cause lasting eye damage or blindness. A brief paralysis of the face, hearing loss, and very rarely, swelling of the brain (encephalitis) can also occur. There is a shingles vaccine recommended for those aged 60 and older. Shingles is not contagious, but one can catch chickenpox from someone with shingles.
Brain FunCtioning
Research has demonstrated that our brain loses 5% to 10% of its weight as we go from 20 to 90 years of age (Fjell & Walhovd, 2010). This decrease in brain volume appears to be due to the shrinkage of neurons, lower number of synapses, and shorter length of axons. According to Garrett (2015), the normal decline in cognitive ability throughout the lifespan has been associated with brain changes, including reduced activity of genes involved in memory storage, synaptic pruning, plasticity, and glutamate and GABA (neurotransmitters) receptors. There is also a loss in white matter connections between brain areas. Without myelin, neurons demonstrate slower conduction and impede each other’s actions. A loss of synapses occurs in specific brain areas, including the hippocampus (involved in memory) and the basal forebrain region. Older individuals also activate larger regions of their attentional and executive networks, located in the parietal and prefrontal cortex, when they perform complex tasks. This increased activation in general correlates with a reduced performance on both executive tasks and tests of working memory when compared to those younger (Kolb & Whishaw, 2011).
Despite these changes the brain exhibits considerable plasticity, and through practice and training, the brain can be modified to compensate for age-related changes (Erber & Szuchman, 2015). Park and Reuter-Lorenz (2009) proposed the Scaffolding Theory of Aging and Cognition which states that the brain adapts to neural atrophy (dying of brain cells) by building alternative connections, referred to as scaffolding. This scaffolding allows older brains to retain high levels of performance. Brain compensation is especially noted in the additional neural effort demonstrated by those individuals who are aging well. For example, older adults who performed just as well as younger adults on a memory task used both prefrontal areas, while only the right prefrontal cortex was used in younger participants (Cabeza, Anderson, Locantore, & McIntosh, 2002). Consequently, this decrease in brain lateralization appears to assist older adults with their cognitive skills in this instance.
Can we improve brain functioning?
Many training programs have been created to improve brain functioning. ACTIVE (Advanced Cognitive Training for Independent and Vital Elderly), a study conducted between 1999 and 2001 in which 2,802 individuals age 65 to 94, suggests that the answer is “yes”. These racially diverse participants received 10 group training sessions and 4 follow up sessions to work on tasks of memory, reasoning, and speed of processing. These mental workouts improved cognitive functioning even 5 years later. Many of the participants believed that this improvement could be seen in everyday tasks as well (Tennstedt et al., 2006). However, programs for older people on memory, reading, and processing speed training demonstrate that there is improvement on the specific tasks trained, but there is no generalization to other abilities in most cases (Jarrett, 2015). Further, these programs have not been shown to delay or slow the progression of Alzheimer’s disease. Although these programs are not harmful, “physical exercise, learning new skills, and socializing remain the most effective ways to train your brain” (p. 207). These activities appear to build a reserve to minimize the effects of primary aging of the brain. Cognitive reserve is a term referring to the fact that a person may be protected for a time from showing negative behavioral changes despite unfavorable changes in the brain due to physical trauma, disease, or age-associated normal changes. This protection can come both from favorable changes in the brain associated with formal education, challenging cognitive activities, and physical activity, past and present, and from inborn differences in factors such as brain size (Bott & Yutsis, 2018).
Parkinson’s disease is characterized by motor tremors, loss of balance, poor coordination, rigidity, and difficulty moving (Garrett, 2015). Parkinson’s affects approximately 1% of those over the age of 60, and it appears more frequently in family members in a little less than 10% of cases. Twenty-eight chromosomal areas have been implicated in Parkinson’s disease, but environmental factors have also been identified and include brain injury. Being knocked unconscious once increases the risk by 32%, and being knocked out several times increases the risk by 174% (Garrett, 2015). Other environmental influences include toxins, industrial chemicals, carbon monoxide, herbicides and pesticides (Olanow & Tatton, 1999). The symptoms are due to the deterioration of the substantia nigra, an area in the midbrain whose neurons send dopamine-releasing axons to the basal ganglia which affects motor activity. Treatment typically includes the medication levodopa (L-dopa), which crosses the blood-brain barrier and is converted into dopamine in the brain. Deep brain stimulation, which involves inserting an electrode into the brain that provides electrical stimulation, has resulted in improved motor functioning (Garrett, 2015).
Sleep: Similar to other adults, older adults need between 7 to 9 hours of sleep per night, but they tend to go to sleep earlier and get up earlier than those younger. This pattern is called advanced sleep phase syndrome and is based on changes in circadian rhythms (National Sleep Foundation, 2009). There are sleep problems in older adults, and insomnia is the most common problem in those 60 and older (NIA, 2016). People with insomnia have trouble falling asleep and staying asleep. There are many reasons why we may have insomnia as an older person, including certain medications, being in pain, having a medical or psychiatric condition, and even worrying before bedtime about not being able to sleep. Using over the counter sleep aids or medication may only work when used for a short time. Consequently, sleep problems should be discussed with a health care professional.
As we get older, other sleep disorders also become more common, including sleep apnea, restless legs syndrome, periodic limb movement disorder, and rapid eye movement sleep behavior disorder (NIA, 2016). Sleep apnea refers to repeated short pauses in breathing, while an individual sleeps, that can lead to reduced oxygen in the blood. Snoring is a common symptom of sleep apnea and it often worsens with age. Untreated sleep apnea can lead to impaired daytime functioning, high blood pressure, headaches, stroke, and memory loss. Restless legs syndrome feels like there is tingling, crawling, or pins and needles in one or both legs, and this feeling is worse at night. Periodic limb movement disorder causes people to jerk and kick their legs every 20 to 40 seconds during sleep. Rapid eye movement sleep behavior disorder occurs when one’s muscles can move during REM sleep and sleep is disrupted.
According to the National Sleep Foundation (2009), there are many medical conditions that affect sleep, and these conditions include gastroesophageal reflux disease, diabetes mellitus, renal failure, respiratory diseases such as asthma, and immune disorders. Diseases such as Parkinson’s disease and multiple sclerosis also commonly cause problems sleeping. Lastly, Alzheimer’s disease can interfere with sleeping patterns. Individuals, especially those in the middle to late disease stages, may wake up many times during the night, wander when up, and yell, which can alter the amount of time they sleep. Both minor and more significant sleep problems in older adults can lead to increased risk of accidents, falls, chronic fatigue, decreased quality of life, cognitive decline, reduced immune function, and depression (Buman, 2013).
Because of sleep problems experienced when we get older, research has looked into whether exercise can improve sleep quality for older people. Results show that 150 minutes per week of exercise can improve sleep quality (Buman, 2013). This amount of exercise is also recommended to improve other health areas including lowering the risk for heart disease, diabetes, and some cancers. Aerobic activity, weight training, and balance programs are all recommended. For the small minority of older people who live in assisted living facilities even light exercise, such as stretching and short walks, can improve sleep. High intensity activity is not necessary to see improvements. Overall, the effects of exercise on sleep may be larger for us when we are older compared to when we were younger since our sleep quality as older people is more likely to be less than ideal before we start an exercise program.
Media Attributions
- Table 9.6
- Table 9.7. Death Percentages for Cancer and Cardiovascular Disease for Selected Age Groups (45-85+)

