Mary’s Health: Osteoporosis (OP)
Typically, there are no symptoms in the early stages of OP.
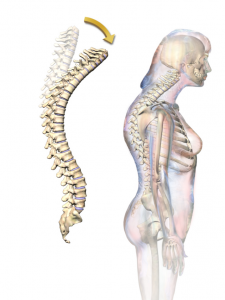
Mary though the back pain was part of growing old, along with the being a ‘bit shorter’ & the slight stoop in her posture.
Overview
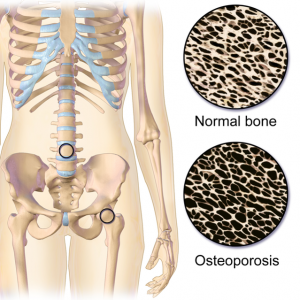
- Causes bones to become weak & brittle
- A fall or even mild stress can cause a fracture
- OP related fractures most commonly occur in the hip, wrist, or spine
- Bone is living tissue that is constantly being broken down & replaced
- OP occurs when the creation of new bone doesn’t keep up with the loss of old bone
- OP affect men & women of all races
- White & Asian women (especially post-menopause) are at higher risk
Causes
- After the early 20s the process of making new bone slows
- Most people reach their peak bone mass by age 30
- How likely you are to develop OP depends partly on how much bone mass you attained in your youth
- Peak bone mass is somewhat inherited and also varies by ethnic group
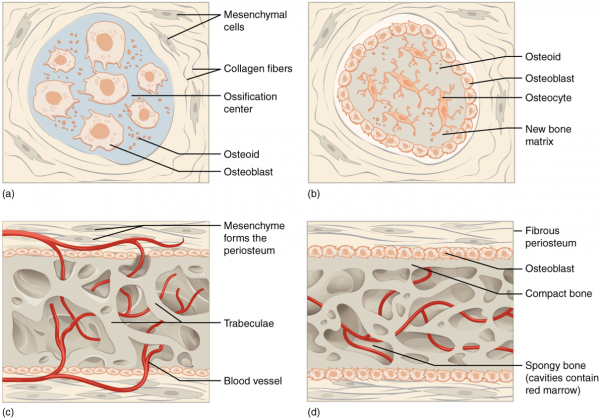
Intramembranous Ossification
Intramembranous ossification follows four steps:
- Mesenchymal cells group into clusters, and ossification centers form.
- Secreted osteoid traps osteoblasts, which then become osteocytes.
- Trabecular matrix and periosteum form.
- Compact bone develops superficial to the trabecular bone, and crowded blood vessels condense into red marrow.
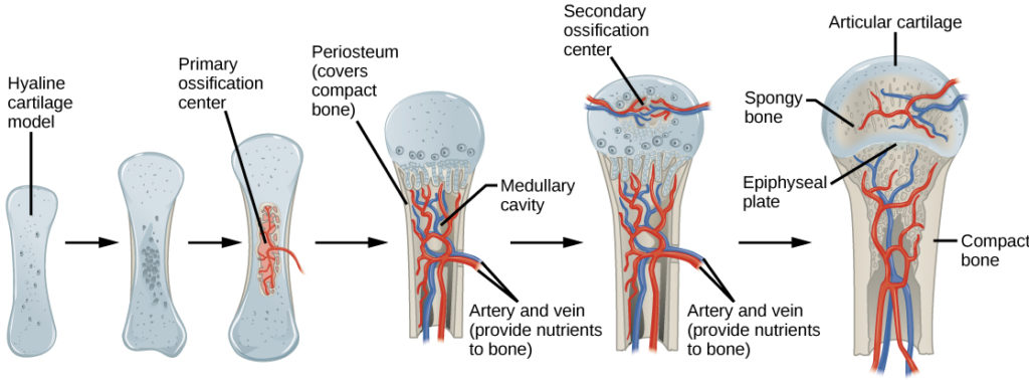
Endochondral Ossification
Endochondral ossification follows six steps:
- Mesenchymal cells differentiate into chondrocytes.
- The cartilage model of the future bony skeleton and the perichondrium form.
- Capillaries penetrate cartilage. Perichondrium transforms into periosteum. Periosteal collar develops. Primary ossification center develops.
- Cartilage and chondrocytes continue to grow at ends of the bone.
- Secondary ossification centers develop.
- Cartilage remains at epiphyseal (growth) plate and at joint surface as articular cartilage.
Risk Factors
| Modifiable Risks | Non-modifiable Risks |
| Alcohol | Age |
| Smoking | Ethnicity |
| Low body mass index (BMI) | Female gender |
| Poor nutrition | Family history of fractures |
| Eating disorders | Previous fractures |
| Insufficient physical activity | Menopause/hysterectomy |
| Low dietary calcium intake | Hormonal status |
| Vitamin D deficiency | Long-term glucocorticoid therapy |
| Frequent falls | Primary/secondary hypogonadism in men |
Complications
Bone fractures:
- Particularly in the spine or hip
- Often caused by a fall & can result in disability
- Increase risk of death within the first year after injury
- Spinal fractures can occur without injury
- Vertebrae can weaken to the point of crumpling
Prevention:
- Good nutrition
- Maintain a health body weight
- Calcium
- Vitamin D
- Exercise
- Limit alcohol consumption
- Quit smoking