Gladys’ Health: Chronic Obstructive Pulmonary Disease (COPD)
Diagnosis
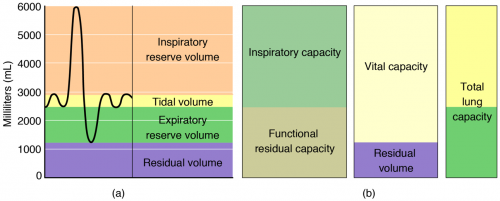
COPD is diagnosed through pulmonary (or lung) function tests. The most common of these tests is spirometry, which measures the amount of air you can inhale and exhale, and whether your lungs deliver enough oxygen to your blood.
During the test, you blow into a large tube connected to a small machine to measure how much air your lungs can hold and how fast you can blow the air out of your lungs.
Other pulmonary function tests include:
- Pulse oximetry
- Blood gases
- End tidal CO₂
- Peak expiratory flow rate
- Bronchial challenge testing
- Exercise tests
- Respiratory muscle pressure measurement
- Lung volumes by helium dilution
- Diffusing capacity
Gladys’s Pulmonary Function Test Results
- FEV₁ – the forced expiratory volume in 1 second
- FVC – the forced vital capacity
- Your FEV₁ is influenced by other factors including age, sex, height, and ethnicity. The FEV₁/FVC ratio is used to define obstructive defect and used to diagnose the disease progression.
| Pulmonary Function Test | Instrument | Measures | Function |
| Spirometry | Spirometer | Forced vital capacity (FVC) | Volume of air that is exhaled after maximum inhalation |
| Forced expiratory volume (FEV) | Volume of air exhaled during one forced breath | ||
| Forced expiratory flow, 25-75 percent | Air flow in the middle of exhalation | ||
| Peak expiratory flow (PEF) | Rate of exhalation | ||
| Maximum voluntary ventilation (MVV) | Volume of air that can be inspired and expired in 1 minute | ||
| Slow vital capacity (SVC) | Volume of air that can be slowly exhaled after inhaling past the tidal volume | ||
| Total lung capacity (TLC) | Volume of air in the lungs after maximum inhalation | ||
| Functional residual capacity (FRC) | Volume of air left in the lungs after normal expiration | ||
| Residual volume (RV) | Volume of air in the lungs after maximum exhalation | ||
| Total lung capacity (TLC) | Maximum volume of air that the lungs can hold | ||
| Expiratory reserve volume (ERV) | Volume of air that can be exhaled beyond normal exhalation | ||
| Gas diffusion | Blood gas analyzer | Arterial blood gases | Concentration of oxygen and carbon dioxide in the blood |
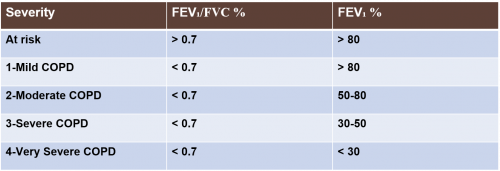
GOLD System of Grading COPD
GOLD stands for the Global Initiative for Chronic Obstructive Lung Disease. The National Heart, Lung, and Blood Institute, National Institutes of Health, and the World Health Organization started it in 1997.
The GOLD system bases the stage of COPD on several things:
- Symptoms
- How many times your COPD has gotten worse
- Hospitalizations for COPD exacerbation
- Spirometry results
COPD Stages
COPD Risk Factors Among Women
- 3.17 million deaths (5% of all global deaths) were caused by COPD in 2015
- WHO reports a prevalence of 251 million cases of COPD in 2016
- More women are being diagnosed with COPD
- Higher mortality rates than men
Most common risk factors:
- Smoking
- Exposure to secondhand smoke
- Air pollution
- Occupational dust and fumes
Influence of sex on COPD involves several factors:
- Differential susceptibility to the effects of tobacco
- Anatomic, hormonal, and behavioural differences
- Differential response to therapy
COPD and Food
- The process of changing food to fuel in the body is called metabolism.
- Oxygen and food are the raw materials of the process.
- Energy and carbon dioxide are the finished products.
- Carbon dioxide is a waste product that is exhaled.
- Metabolism of carbohydrates produces the most carbon dioxide for the amount of oxygen used.
- Metabolism of fat produces the least.
- For some COPD patients, eating a diet with fewer carbohydrates and more fat helps them breathe easier.
Nutritional Guidelines
- Choose complex carbohydrates.
- Limit simple carbohydrates.
- Eat 20 to 30 grams of fiber each day.
- Eat a good source of protein.
- Choose mono- and polyunsaturated fats.
- Limit foods that contain trans fats and saturated fats.
- Drink plenty of water – keeps you hydrated and keeps the mucus thin
- Vitamins and minerals:
- Steroids may increase your need for calcium
- Calcium carbonate or calcium citrate with vitamin D
- Sodium may cause edema and may increase blood pressure
Diet Tips
- Rest before eating.
- Eat more food early in the day if you are usually too tired to eat later on.
- Avoid foods that cause gas or bloating. Tends to make breathing more difficult.
- Eat 4 to 6 small meals a day. Enables the diaphragm to move freely and lets the lungs fill and empty more easily.
- Drinking fluids with meals may make you feel too full. Drink an hour before or after meals.
- Consider adding nutritional supplements at night to avoid feeling full during the day.
COPD and Exercise
Moderate exercise can improve:
- The body’s use of oxygen
- Energy levels
- Anxiety, stress, and depression
- Sleep
- Self-esteem
- Cardiovascular fitness
- Muscle strength
- SOB
Exercises help blood circulate, help your heart send oxygen to your body, and strengthen your respiratory muscles.
Types of Exercises for COPD
Pulmonary Rehabilitation consists of education and exercise classes that teach about lungs, the disease, and how to exercise and be more active with less SOB.
Examples include:
- Stretching
- Aerobic
- Resistance
COPD and Emotional Health
Most COPD patients experience feelings of sadness, fear, and worry.
If those feelings start to affect ability to keep up with normal activities and life enjoyment, they may be symptoms of anxiety and depression.
Managing anxiety and depression can increase ability to stick with treatment, improve physical health, and reduce medical costs.
Things to do:
- Talk to your healthcare team about your feelings
- Take care of yourself
- Connect with others who understand
Medications for COPD
Bronchodilators
- Relax the muscles around the airways (short- and long-acting)
- Beta₂-Agonists relax tightened muscles around airways, opening the airways, making breathing easier
- Anticholinergics prevent the muscles around the airways from tightening, helps clear mucus from lungs
Anti-inflammatories
- Known as corticosteroids or steroids
- Inhaler device or oral pill
- Reduces swelling and mucus production
- Long-term use of steroids have serious side effects
Combination Medications
- A corticosteroid, an anticholinergic, and a beta₂-agonist
- Most common combinations:
- Short-acting beta₂-agonist & short-acting anticholinergic
- Long-acting beta₂-agonist and corticosteroid
- Long-acting anticholinergic and corticosteroid
- Long-acting beta₂-agonist and long-acting anticholinergic
- Long-acting beta₂-agonist, long-acting anticholinergic, and corticosteroid
Vaccinations
- Influenza
- Pneumonia