Gladys’ Health: Alzheimer’s
1999 – Diagnosed with COPD
2010 – Cognitive changes – diagnosed with Alzheimer’s disease
2015 – Oxygen therapy for COPD
2018 – Health and wellbeing deteriorated – placed in LTC facility
2019 – Dies due to complications of Alzheimer’s disease
Causes of Alzheimer’s Disease
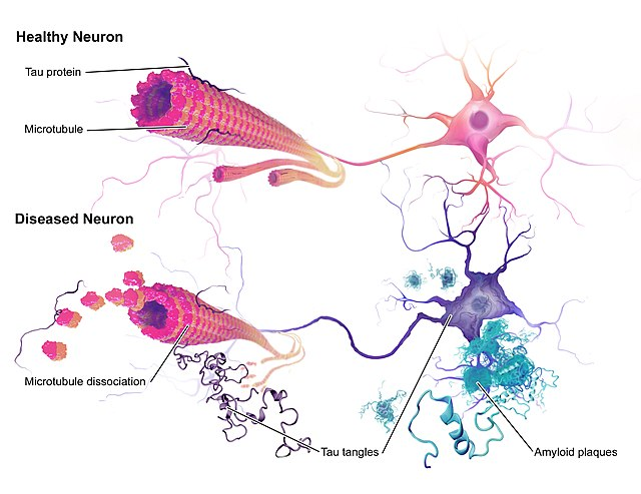
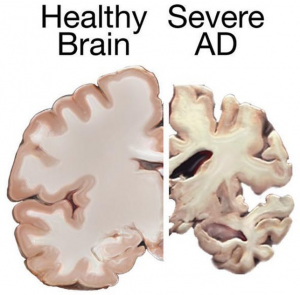
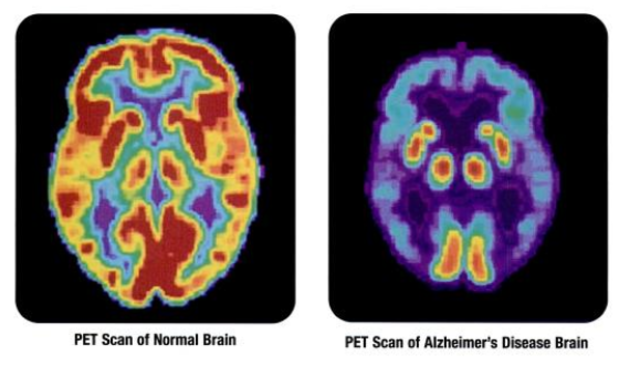
People with AD gradually suffer memory loss and a decline in thinking abilities, as well as major personality changes. These losses in cognitive function are accompanied by changes in the brain, including the build-up of amyloid plaques and tau-containing neurofibrillary tangles, which result in the death of brain cells and the breakdown of the connections between them.
Amyloid plaques and neurofibrillary tangles are the primary hallmarks of Alzheimer’s disease. Plaques are dense deposits of protein and cellular material outside and around the brain’s nerve cells. Tangles are twisted fibers that build up inside the nerve cells. Scientists have known about plaques and tangles since 1906, when a German physician, Dr. Alois Alzheimer, first identified them in the brain of woman who had died after suffering paranoid delusions and psychosis.
Personality and Behaviour Changes
Common Changes in Personality & Behaviour
- Getting upset, worried, and angry more easily
- Acting depressed or not interested in things
- Hiding things or believing other people are hiding things
- Imagining things that aren’t there
- Wandering away from home
- Pacing a lot
- Showing unusual sexual behaviour
- Hitting others
- Misunderstanding what they see or hear
- Stops caring about how they look
Managing Personality Changes
- Keep things simple; Ask or say one thing at a time
- Have a daily routine
- Reassurance that they are safe and you are there to help
- Focus on their feelings rather than their words
- Don’t argue or try to reason with them
- Try not to show frustration or anger
- Use humor when appropriate
- Allow a safe environment for pacing
- Try using music, singing, or dancing for distraction
- Ask them to help (“let’s set the table” or “I need help folding the clothes”)
Changes in Communication Skills
Persons with Alzheimer’s may have problems with:
- Finding the right word or losing their train of thought when speaking
- Understanding what words mean
- Paying attention during long conversations
- Remembering the steps in common activities
- Blocking out background noises
- Frustration if communication is not working
- Being very sensitive to the tone and loudness of voices
Making Communication Easier
Understand that Alzheimer’s causes changes in communication skills.
Try some tips that may make communication easier:
- Make eye contact and use their name
- Beware of your tone, loudness of voice, and body language
- Encourage two-way conversation for as long as possible
- Use other methods besides speaking, such as gentle touch
- Try distraction if communication creates problems
- Be patient
- Offer simple step-by-step instructions
- Try not to interrupt
- Don’t talk to the person using “baby talk” or a “baby voice”
Medications
| Drug Name | Drug Type & Use | How It Works | Common Side Effects | Manufacturer’s Recommended Dosage |
| Aricept® (donepezil) | Cholinesterase inhibitor prescribed to treat symptoms of mild, moderate, and severe Alzheimer’s | Prevents the breakdown of acetylcholine in the brain | Nausea, vomiting, diarrhea, muscle cramps, fatigue, weight loss |
|
| Exelon® (rivastigmine) | Cholinesterase inhibitor prescribed to treat symptoms of mild to moderate Alzheimer’s (patch is also for severe Alzheimer’s) | Prevents the breakdown of acetylcholine and butyrylcholine (a brain chemical similar to acetylcholine) in the brain | Nausea, vomiting, diarrhea, weight loss, indigestion, muscle weakness |
|
| Namenda® (memantine) | N-methyl D-aspartate (NMDA) antagonist prescribed to treat symptoms of moderate to severe Alzheimer’s | Blocks the toxic effects associated with excess glutamate and regulates glutamate activation | Dizziness, headache, diarrhea, constipation, confusion |
|
| Namzaric® (memantine and donepezil) | NMDA antagonist and cholinesterase inhibitor prescribed to treat symptoms of moderate to severe Alzheimer’s | Blocks the toxic effects associated with excess glutamate and prevents the breakdown of acetylcholine in the brain | Headache, nausea, vomiting, diarrhea, dizziness, anorexia |
|
| Razadyne® (galantamine) | Cholinesterase inhibitor prescribed to treat symptoms of mild to moderate Alzheimer’s | Prevents the breakdown of acetylcholine and stimulates nicotinic receptors to release more acetylcholine in the brain | Nausea, vomiting, diarrhea, decreased appetite, dizziness, headache |
|
DNR and DNH Orders
- Ontario nursing home DNR & DNH orders reduce inappropriate hospitalizations, but not entirely
- 3 in 5 nursing home residents had a DNR recorded on admission (Do Not Resuscitate)
- 1 in 7 had a DNH (Do Not Hospitalize)
- Residents with a DNR or DNH were less likely to experience hospitalization or in-hospital death
Hospitalization:
- DNR: 13% less likely
- DNH: 30% less likely
In-hospital death:
- DNR: 40% less likely
- DNH: 60% less likely