Jack’s Health: Diabetic Foot Ulcers
Jack’s Story Continues
- Jack is found by his daughter unkempt, SOB, limping slightly, and has a strange odor coming from him
- States he has not been eating or managing his blood sugars and insulin well
- Has not bathed since his wife went to hospital (unable to access the bathtub safely)
- Blood glucose level is 12.4 mmol/L
- Heart rate 130 BPM
- Daughter finds an open, oozing wound on Jack’s foot
Symptoms and Diagnosis
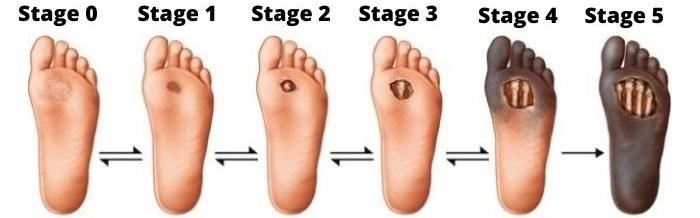
Wagner Ulcer Classification System:
- 0: no open lesions, may have healed lesion
- 1: superficial ulcer without penetration to deeper layers
- 2: deeper ulcer, reaching tendon, bone, or joint capsule
- 3: deeper tissues involved, with abscess, osteomyelitis, or tendonitis
- 4: gangrene in a portion of forefoot or heel
- 5: extensive gangrenous involvement of the entire foot
Causes
Poor circulation – blood does not flow to feet efficiently, also making ulcers more difficult to heal
Hyperglycemia – can slow healing process
Nerve damage – tingling and pain, decrease or loss of feeling
Irritated or wounded foot – reduced sensitivity results in painless wounds
Wearing inappropriate footwear – may be significant in wound progression
Treatment
Treatment primarily depends on the stage of the ulcer. Essential to start treatment as soon as possible – helps prevent infection and provides better results sooner
- Antibiotics if applicable (C&S of wound site)
- Shoes designed for individuals with DM
- Debridement
- Foot baths
- Disinfecting the skin around the ulcer
- Keeping the ulcer dry with frequent dressing changes
- Dressings containing calcium alginates to inhibit bacterial growth
- Surgical procedures – shave bone or removing foot abnormalities (bunions or hammertoes)
- Other treatment options ineffective – amputation
Prevention
- Washing feet every day
- Keeping toenails adequately trimmed, but not too short
- Keeping feet dry and moisturized
- Changing socks frequently
- Seeing a podiatrist for corn and callus removal
- Wearing proper-fitting shoes