5 Amanda is Referred to a Pain Clinic
5.1 Amanda Continues with Persistent but Focal Pain
Approximately three months after the injury, Amanda continued to improve with regards to pain in her left upper arm. She was motivated to get back into good health so that she would not lose her newly found job. The physiotherapy, funded by her insurance company, was useful in reducing stiffness and restoring mobility, and generally reducing pain overall. She also committed herself to exercise and to stay active. However, despite being on conservative therapy, including medications, physical therapy, and routine activity, she continued to notice persistent pain around the lower aspect of her left neck. Unlike her other pains, which had resolved, this pain tended to worsen with activity, and was particularly severe when she looked up or to the left. This pain would sometimes radiate toward her left shoulder. She was referred to a chronic pain clinic by her family physician. Amanda’s clinical assessment was suggestive of a possible diagnosis of cervical facet joint pain involving the lower facet joints. This was supported by imaging findings of mild to moderate facet changes in the suspected joints.
5.2 The Importance and Diagnosis of Facet Joint Pain
Facets joints are commonly observed to be involved in patients with whiplash. The anatomy and the role of facet joints have been discussed earlier in Chapter 3, and the injury mechanisms have been discussed in Chapter 4 (Figure 4-1 and Figure 4-2). Those with an injury of the facet joints can present with complaints of chronic axial neck pain, which typically worsens with activity. The prevalence of this persisting pain varies from 36% to 67%,1 although some well-quoted studies put it higher at 54% to 60%.2,3 The most common joints involved during whiplash injury include C2-C3 and C5-C6,2 and approximately one-half (53%) of chronic headaches following a whiplash injury is attributed to C2-C3 facet joint.4
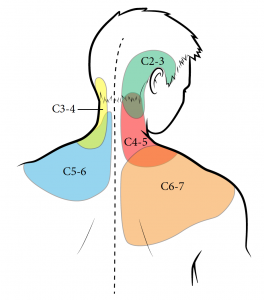
Pain of facet joint etiology is suspected when the area of pain and tenderness matches with the referral pattern indicated for the joints involved (Figure 5-1). Clinically, no specific sign or symptom sets this apart. Several human studies have reinforced the non-dermatomal referral patterns involved in this condition.5 A normal diagnostic imaging does not rule out facet joint pain. Significant pain originating from a facet joint may in turn cause secondary pain from the overlying myofascial elements. This secondary pain tends to improve temporarily (depending on the extent) with simple interventions such as manual therapy, acupuncture, stretching or trigger point injections. However, the specific management of facet joint pain involves targeted spinal interventions aimed at confirming the diagnosis and providing therapeutic management.
REVIEW 5.1
How can a diagnosis of facet joint pain be made?
- Clinical features are diagnostic
- Imaging findings are diagnostic
- An indirect diagnosis can be made by blocking the medial branches
Correct answer: 1
5.3 Interventional Management of Facet Joint Pain: Medial Branch Blocks and Radiofrequency Techniques
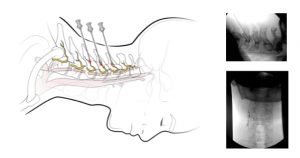
Amanda was informed of the clinical diagnosis of facet joint pain and the necessity to do cervical medial branch blocks to confirm the diagnosis. She underwent blocks of C4, C5, C6, and C7 medial branches to block the pain from C4-C5, C5-C6, and C6-C7 facet joints on the left side. Since there is a possibility of false positive response, she underwent the blocks twice to increase the diagnostic accuracy.3 As a confirmatory sign of positive diagnostic response, her pain scores decreased along with improvement in functions, for the expected duration of the diagnostic test. Amanda was then informed about radiofrequency neurotomy of those medial branches, with an aim to decrease the pain signals on a therapeutic basis (months to years). She was informed of the procedure and related expectations, including risks.6-8
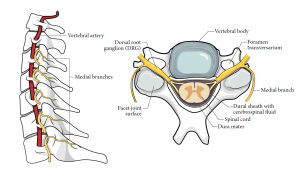
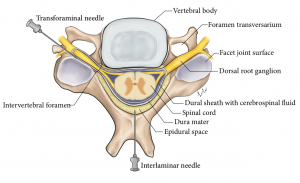
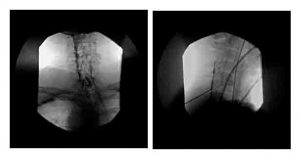
Like any other joint with possible inflammatory pathology, facet joints are injected with steroid solutions (intra-articular injections) with the aim of reducing inflammation (if existent), or modifying pain signals (mechanism uncertain).9 This is a day procedure with image guidance, usually in the form of fluoroscopy (ultrasound guidance is possible). The performance of this procedure involves necessary safety precautions and training, as it has risks inherent to a neuraxial injection. Alternatively, pain sensation from a painful joint can be reduced by dealing with the nerve(s) carrying its pain signals. Studies demonstrated that the predominant nerve supply for the facet joints come from the medial branches of the dorsal rami of a spinal nerve.1,10 The innervation is explained as follows (Figure 5-2, left). Each cervical facet joint contains small-diameter, high-threshold nociceptive fibers in the joint capsules, synovial inclusions, and subchondral bone. Each joint is innervated from a branch from above and one from below. Thus C5-C6 joint is innervated from C5 medial branch and C6 medial branch. Each medial branch originates from the dorsal ramus and curves backward (dorsal and medial), across the lateral aspect of facet pillar (Figure 5-2, right). The treatment plan involves diagnostic blocks (Figure 5-3), followed by radiofrequency neurotomy (Figure 5-4) of the involved medial branches.
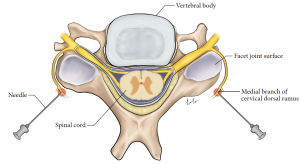
Cervical Medial Branch Blocks
This diagnostic test checks whether the patient’s pain is mediated by the specific cervical medial branches considered to be blocked. Medial branches carry pain signals from the facet joints. Blocking them would indirectly indicate whether those particular facet joints are a source of pain. Being target specific, this procedure has to be done under image guidance (commonly fluoroscopy guidance). It requires exact positioning of the needle at a bony target (Figure 5-3) where medial branches are exposed. A local anesthetic solution, usually 0.3 to 0.5 ml, is injected. Clinical success is indicated by a decrease in pain scores and improvement in functions.
This corresponds to the duration of the local anesthetic used; lidocaine and bupivacaine act for one to two hours and four to six hours, respectively. Consistent positive results in both are indicative of a positive diagnosis and predict success with the subsequent radiofrequency procedure. Like any other diagnostic test, this has established sensitivity and specificity. A single test, even if positive, can lead to a false positive diagnosis. Similarly, a double test can lead to increased specificity at the expense of some false negative results. Clinicians need to bear this in mind while employing this test, either simply as a diagnostic tool or even for predictive utility for subsequent radiofrequency neurotomy.11
Amanda underwent radiofrequency neurotomy with good results (Figure 5-4). She started to notice that her pain almost disappeared and significantly improved her functional ability. She was told that the pain may reappear after 12 to 15 months and that the procedure (radiofrequency neurotomy) could be repeated in that case.12 She was informed of the importance of physical therapy and regular exercises to keep her neck muscles active and desensitized (See Chapter 8.2 and online tool).
Radiofrequency Neurotomy
Radiofrequency neurotomy causes localized necrosis of tissues due to heat. The apparatus involves an radiofrequency generator to which a special conducting needle is connected. The application of radiofrequency generates heat around the tip of the needle. This leads to a controlled coagulative necrosis.13 An oval-shaped zone of necrosis occurs just around the needle tip. The temperature is measured and controlled (at 80°C) by a thermocouple present at the tip of the needle. During this process, the radiofrequency needle is placed at the same site as for the medial branch block, but through a parallel direction of insertion to the respective medial branch. This is intended to catch the medial branch (small nerve) within its necrosis zone. The procedure has to be performed under image guidance. Motor nerve testing is conducted to rule out the proximity of the needle to the ventral rami, before carrying out the radiofrequency lesion.
There are multiple studies indicating the clinical success achieved with this procedure. It is expected that, when appropriately performed, cervical radiofrequency treatment can lead to successful pain relief in up to 70% of individuals with a mean duration of relief of up to one year.1,14
Specific to WAD, systematic reviews note strong scientific evidence for radiofrequency treatment.15 The average duration of pain relief resulting from this lasts approximately one year. It can be successfully repeated to give continuing pain relief.16 It has also been shown that radiofrequency treatment of cervical medial branches can reduce the hyperexcitability of muscles associated with WAD.17 As a long-term effect, it has been shown to attenuate the nociceptive pain and psychological responses.8
Key Takeaways
- An effective treatment involving radiofrequency neurotomy of medial branches can potentially provide pain relief lasting several months to years.
- Cervical radiofrequency neurotomy is an advanced spinal intervention performed with image guidance.
- The evidence level for the use of cervical epidural steroid injections in facet joint pain is poor.
5.4 Other Interventional Modalities of Treatment: Epidural Steroid Injections and Neuromodulation
In some patients, axial neck pain can be associated with chronic radicular pain involving some part of the upper extremity. This could result from multiple causes such as nonacute disc herniation, whiplash-associated injury in a patient with age-related degeneration involving spinal stenosis, or facet arthropathy causing hypertrophy and narrowing of the spinal canal. When chronic pain of this nature does not respond to conservative therapy, alternative spinal interventions are tried.
Cervical Epidural Steroid Injections
This is commonly done for patients with radicular pain due to involvement of cervical nerve roots. This indication is supported by level II evidence (low-quality RCTs) in the literature.18 However, in practice, it is sometimes also considered for chronic cervical axial pain. The evidence support for this is poor.19 As shown in Figure 5-5, the steroid solution can be deposited near the site of pathology from two approaches. Both are technically challenging procedures, and need considerable expertise. The mechanism involves anti-inflammatory and other effects of steroids and the washout of mediators from the injectate itself.20 Most commonly, an interlaminar epidural steroid injection is performed between C7-T1 under fluoroscopic guidance (Figure 5-6). However, a transforaminal approach can deposit the injectate more specifically at the affected level. Image guidance is a must for this approach. Expectation of success and decision on a repeat injection is based on individual case response.
Neurostimulation
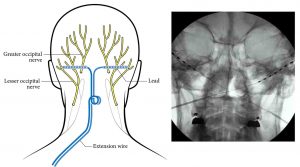
In patients with disabling, chronic cervical pain, spinal cord or peripheral nerve stimulators are an option. The response is better with pain of a radicular nature (neuropathic) compared with a nonspecific pain of an axial nature.21 The spinal cord stimulation, more accurately termed as dorsal column stimulation, involves placement of percutaneous (smaller and thinner) or paddle (flatter and broader) leads with electrical contacts (Figure 5-7 and Figure 5-8, respectively). The placement of the percutaneous leads can be done with the patient awake while the paddle leads require surgical laminectomy for placement. The electrical contacts stimulate the spinal dorsal column in the epidural space to bring about nonpainful paresthesia, captured within the zone of pain.22
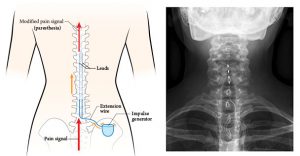

Although the mechanism of analgesia resembles the well-known gate control theory, there are other postulated mechanisms as well. The process involves a trial procedure, where temporary leads are placed. The patient’s perception, both in pain relief and satisfaction, indicates trial success or failure. Following a successful trial, the leads are connected to an impulse generator that is inserted in a subcutaneous pouch (Figure 5-7, left panel). This leads to provision of pain relief for an indefinite time period. The peripheral nerve stimulator follows a similar concept, but it is inserted near a peripheral nerve to cover a corresponding area of pain (Figure 5-9).23 The option of neurostimulators is expensive and is not routinely supported by insurance companies or provincial health providers. For poorly understood reasons, there is a reduced efficacy after a span of four to five years.
5.5 Discharge from the Pain Clinic
Amanda gradually returns to normal activities and continues with her physiotherapy for two more months (see Chapter 8). She continues on a self-managed program. Two weeks after the radiofrequency treatment, Amanda feels there is no need for analgesic medication.
5.6 References
- Bogduk N. On cervical zygapophysial joint pain after whiplash. Spine 2011;36(25 Suppl):S194-9.
- Barnsley L, Lord SM, Wallis BJ, Bogduk N. The prevalence of chronic cervical zygapophysial joint pain after whiplash. Spine 1995;20:20-5; discussion 6.
- Lord SM, Barnsley L, Wallis BJ, Bogduk N. Chronic cervical zygapophysial joint pain after whiplash. A placebo-controlled prevalence study. Spine 1996;21:1737-44; discussion 44-5.
- Lord SM, Barnsley L, Wallis BJ, Bogduk N. Third occipital nerve headache: a prevalence study. J Neurol Neurosurg Psychiatry 1994;57:1187-90.
- Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: A study in normal volunteers. Spine 1990;15:453-7.
- Engel A, Rappard G, King W, Kennedy DJ. The effectiveness and risks of fluoroscopically-guided cervical medial branch thermal radiofrequency neurotomy: a systematic review with comprehensive analysis of the published data. Pain Med 2016;17:658-69.
- Klessinger S. Cervical medial branch radiofrequency neurotomy. Pain Med 2012;13:621.
- Smith AD, Jull G, Schneider GM, Frizzell B, Hooper RA, Sterling M. Modulation of cervical facet joint nociception and pain attenuates physical and psychological features of chronic whiplash: a prospective study. PM & R 2015;7:913-21.
- Mukai A, Kancherla V. Interventional procedures for cervical pain. Phys Med Rehabil Clin N Am 2011;22:539-49, x.
- Bogduk N, Aprill C. On the nature of neck pain, discography and cervical zygapophysial joint blocks. Pain 1993;54:213-7.
- Barnsley L, Lord S, Wallis B, Bogduk N. False-positive rates of cervical zygapophysial joint blocks. Clin J Pain 1993;9:124-30.
- Husted DS, Orton D, Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for cervical facet joint pain. J Spinal Disord Tech 2008;21:406-8.
- Cosman ER Jr, Cosman ER Sr. Electric and thermal field effects in tissue around radiofrequency electrodes. Pain Med 2005;6:405-24.
- Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. New Engl J Med 1996;335:1721-6.
- Seferiadis A, Rosenfeld M, Gunnarsson R. A review of treatment interventions in whiplash-associated disorders. Eur Spine J 2004;13:387-97.
- McDonald GJ, Lord SM, Bogduk N. Long-term follow-up of patients treated with cervical radiofrequency neurotomy for chronic neck pain. Neurosurgery 1999;45:61-7; discussion 7-8.
- Smith AD, Jull G, Schneider G, Frizzell B, Hooper RA, Sterling M. Cervical radiofrequency neurotomy reduces central hyperexcitability and improves neck movement in individuals with chronic whiplash. Pain Med 2014;15:128-41.
- Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med 2013;38:175-200.
- Diwan S, Manchikanti L, Benyamin RM, et al. Effectiveness of cervical epidural injections in the management of chronic neck and upper extremity pain. Pain Physician 2012;15:E405-34.
- Rathmell JP. The proper role for epidural injection of corticosteroids. Anesthesiology 2014;121:919-21.
- Vallejo R, Kramer J, Benyamin R. Neuromodulation of the cervical spinal cord in the treatment of chronic intractable neck and upper extremity pain: a case series and review of the literature. Pain Physician 2007;10:305-11.
- Linderoth B, Foreman RD, Meyerson BA. Mechanisms of action of spinal cord stimulation. In: Lozano A, Gildenberg P, Tasker R, eds. Textbook of Stereotactic and Functional Neurosurgery: Springer Berlin Heidelberg; 2009. p. 2331-47.
- Kapural L, Sable J. Peripheral nerve stimulation for occipital neuralgia: surgical leads. Prog Neurol Surg 2011;24:86-95.
